Abstract
We present 2 cases of complicated mechanical thrombectomy involving tandem cervical internal carotid artery and middle cerebral artery occlusion using the Solitaire FR stent and simultaneous carotid stent angioplasty. During the procedures, the Solitaire stents containing the thrombus were wedged into the open-cell carotid stents, which were already deployed for proximal flow restoration. We describe the methods used to avoid and overcome such complications.
The use of mechanical thrombectomy for acute intracranial arterial occlusion is increasing, with favorable clinical and radiological results. The Solitaire stent is a popular device for intracranial thrombectomy because it enables recanalization of the occluded vessel without the use of intra-arterial thrombolytic agents, thereby reducing the risk of cerebral hemorrhagic complications.3)13)15)18) However, tandem lesions with cervical internal carotid artery (ICA) steno-occlusion and intracranial major arterial occlusion are challenging and require special attention for proximal flow restoration.6)8)11)12)21)23) Whether to open the proximal occlusion first or last and whether to place a stent remain controversial.1)5)14)19)22) We present 2 cases of successful recanalization of tandem lesions involving middle cerebral artery (MCA) occlusion and cervical ICA steno-occlusion using a retrievable Solitaire FR stent. However, these 2 procedures were problematic because the thrombus-containing Solitaire stents became lodged in the already deployed open-cell carotid stents.
A 62-year-old man was hospitalized for abrupt onset of grade 2 left hemiparesis and aphasia, which occurred 2 hours before admission. His initial National Institute of Health Stroke Scale (NIHSS) score was 10. He had been taking antihypertensive medication and oral hypoglycemic agents for long-standing hypertension and diabetes mellitus. Brain magnetic resonance imaging (MRI) revealed hyper-acute cerebral infarction of the right basal ganglia and multiple regions of the right MCA territory. MR angiography (MRA) showed right cervical internal ICA occlusion with poor collateral circulation from the posterior region and the contralateral side. Perfusion computed tomography (CT) showed severe decrease in perfusion in the right MCA territory. Because of the discrepancies between diffusion and perfusion, mechanical thrombectomy, following our institutional protocols for acute major stroke, was initiated. Acetylsalicylic acid (500 mg) and clopidogrel (300 mg) were administered to the patient through a Levin tube.
The procedure was performed under general anesthesia because the patient was agitated; the activated clotting time (ACT) was maintained at 1.5–2.0 times the basal ACT. A balloon-guided catheter was inserted into the right common carotid artery (CCA). The course from the femoral artery to the CCA was very tortuous. Angiography showed severe atherosclerotic stenosis and occlusion of the ICA from its proximal cervical origin, in addition to M1 occlusion (Fig. 1A, B). To increase the possibility of full recanalization of both the distal and proximal lesions, proximal blood flow restoration was initiated. Balloon angioplasty to open the occluded cervical ICA was performed using a Sterling balloon (Boston Scientific, Natick, MA, USA). Three attempts at ballooning resulted in slight recanalization. However, the opening was too narrow to allow increased blood flow into the intracranial vessels. Therefore, carotid stent angioplasty was performed using a Protégé stent (eV3, MN, USA) (Fig. 1C), followed by intra-arterial mechanical thrombectomy for the occluded MCA using a 4 × 20-mm Solitaire stent (eV3, Irvine, CA, USA). After stent deployment and thrombus capture, the stent and its delivery microcatheter were gently and continuously retrieved. During retrieval, negative suction/aspiration of the guide catheter with a 50-mL syringe was performed simultaneously. However, when the Solitaire stent arrived at the mid-point of the carotid stent, its mesh structure was caught and wedged in the open-cell strut angle of the stent (Fig. 1D). To-and-fro movement of the microcatheter and the Solitaire stent failed to release the stentriever. Full retrieval of the stent into the microcatheter was futile because of the captured clot in the stentriever (Fig. 1E). Because of the severe tortuosity of the vessel, it was impossible to advance the guide catheter to capture the stent and microcatheter. An Amplatz Super Stiff Guidewire (Boston Scientific) was inserted into the guide catheter, but manipulation around the Solitaire stent was unsuccessful. After using various combinations of prescribed methods, we finally succeeded in releasing the Solitaire stent from the carotid stent. However, the same complication occurred twice during passage through the carotid stent. Eventually, the Solitaire stent and microcatheter were removed safely by gentle massage over the carotid stent and simultaneous to-and-fro movement of the stentriever system. The occluded MCA was fully recanalized (modified Thrombolysis in Cerebral Infarction [mTICI] Grade 3). Post-thrombectomy diffusion MRI revealed no evidence of further infarction; the following day, the patient's NIHSS score was 5. The patient underwent active rehabilitation and had a modified Rankin score of 1 at 3-month follow-up.
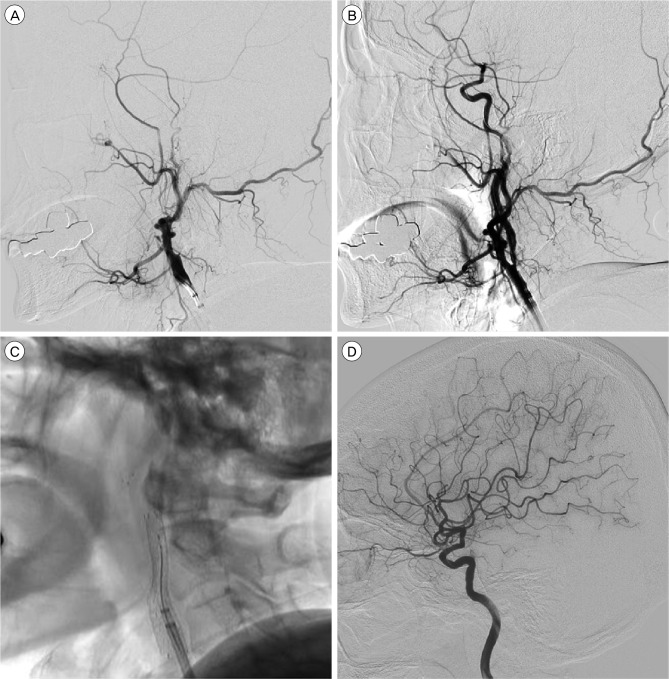
A 64-year-old woman was admitted with left hemiplegia. She had right ICA occlusion with NIHSS score of 18 (Fig. 2A). Emergent recanalization was performed. On the basis of our experience in the abovementioned case, we partially recanalized the cervical ICA with a balloon and then performed intracranial thrombectomy with a Solitaire stent prior to carotid stenting (Fig. 2B). After recanalization (mTICI Grade 2b), a Protégé stent was deployed in the cervical ICA with distal emboli protection. However, after 5 minutes, thrombus formation and re-occlusion occurred in the superior trunk of the MCA. Thus, another thrombectomy with a Solitaire stent was performed. The guide catheter was advanced into the distal CCA within the proximal region of the carotid stent. There was no available intermediate distal access catheter in our institute at the time of the procedure. We deployed the stent in the superior trunk of the M2 segment and retrieved it to achieve recanalization (mTICI Grade 3). However, during stent retrieval, the above mentioned scenario re-occurred (Fig. 2C). Capture of the wedged stent by advancing the guide catheter was impossible because of the small caliber of the cervical ICA and the rough and irregular surface of the open-cell cervical ICA stent. However, in this case, the stent and microcatheter were easily released by a to-and-fro movement of both instruments. Reperfusion (mTICI Grade 3) was achieved (Fig. 2D). The patient recovered, with an NIHSS score of 4 the following day.
Simultaneous occlusion of the cervical ICA and the intracranial arteries is encountered frequently, and the treatment for such cases should be tailored individually. Mechanical thrombectomy using various devices such as the Solitaire stent or a Penumbra catheter has become popular.7)8)20)23)
The cases presented here highlight the possible dangers of using the Solitaire stent in intracranial thrombectomy after the deployment of a self-expanding open-cell carotid stent. The captured thrombus in the Solitaire stent widened the stentriever considerably, and consequently, the stent mesh structure was caught by the crown, open-cell angle of the carotid stent, rendering it impassable. Because of the tortuosity of the proximal vessel and various other reasons, the guide catheter could not be advanced to capture the wedged stent. The effort to separate the stent using a guide wire was unsuccessful. Finally, gentle massage over the carotid stent with to-and-fro movement of the microcatheter and stent was effective in freeing the Solitaire.
As noted, the construction of the open-cell carotid stent was the primary source of hindrance in the cases we encountered.16) To avoid similar problems, choosing a closed-cell carotid stent such as a Wall stent is advisable. However, main drawback of the closed-cell stent is the phenomenon of shortening. And advancing the guiding catheter into the stent to help retrieval of the stentriever can make the stent shorter than expected. Therefore, this method should be addressed carefully.
Additionally, the use of a 5- or 6-Fr coaxial distal access catheter with indwelling Solitaire stent and delivery catheter may prevent such complications. Performing carotid stent angioplasty as the final procedure, or using another thrombectomy device such as a Penumbra catheter instead of the Solitaire stent, may be viable alternatives.2)9)10)17) If advancing the guide catheter and capturing the Solitaire stent is possible, such difficulties may be easily resolved. Cobb et al. reported a complicated case requiring surgical removal of the retained Solitaire stent inside the carotid stent after mechanical thrombectomy.4) In the reported cases, we rectified the problem by employing massage over the carotid stent, with to-and-fro movement of the system, demonstrating that gentle manipulation of the delivery catheter and stent can be effective.
In endovascular procedures using the Solitaire stent for simultaneous occlusion of the cervical ICA and intracranial arteries, caution is warranted to avoid wedging the Solitaire stent in the open-cell carotid stent. Awareness of potential problems is essential. Changing the order of procedures, selecting other devices for carotid stenting and thrombectomy, adding a distal access device before an intracranial procedure or gentle carotid stent massage with to-and-fro stentriever movement may prevent or resolve problems that arise.
References
1. Akpinar CK, Gurkas E, Aytac E. Carotid angioplasty-assisted mechanical thrombectomy without urgent stenting may be a better option in acute tandem occlusions. Interv Neuroradiol. 2017; 8. 23(4):405–411. PMID: 28504557.

2. Behme D, Knauth M, Psychogios MN. Retriever wire supported carotid artery revascularization (ReWiSed CARe) in acute ischemic stroke with underlying tandem occlusion caused by an internal carotid artery dissection: Technical note. Interv Neuroradiol. 2017; 6. 23(3):289–292. PMID: 28162027.

3. Castano C, Dorado L, Guerrero C, Millan M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010; 8. 41(8):1836–1840. PMID: 20538693.
4. Cobb MIH, Smith TP, Brown PA, Gonzalez LF, Zomorodi AR. Carotid Endarterectomy to Remove Retained Solitaire Stent Retriever inside Carotid Stent after Mechanical Thrombectomy. J Stroke Cerebrovasc Dis. 2017; 5. 26(5):e90–e95. PMID: 28318956.

5. Cohen JE, Gomori JM, Rajz G, Itshayek E, Eichel R, Leker RR. Extracranial carotid artery stenting followed by intracranial stent-based thrombectomy for acute tandem occlusive disease. J Neurointerv Surg. 2015; 6. 7(6):412–417. PMID: 24727131.

6. Cohen JE, Gomori M, Rajz G, Moscovici S, Leker RR, Rosenberg S, et al. Emergent stent-assisted angioplasty of extracranial internal carotid artery and intracranial stent-based thrombectomy in acute tandem occlusive disease: technical considerations. J Neurointerv Surg. 2013; 9. 5(5):440–446. PMID: 22753268.

7. Forlivesi S, Pancheri E, Moretto G, Bovi P, Cappellari M. Early secondary prevention after initially ineffective revascularization treatments for acute ischemic stroke due to tandem occlusion. Blood Coagul Fibrinolysis. 2017; 9. 28(6):493–495. PMID: 28319471.

8. Grigoryan M, Haussen DC, Hassan AE, Lima A, Grossberg J, Rebello LC, et al. Endovascular treatment of acute ischemic stroke due to tandem occlusions: large multicenter series and systematic review. Cerebrovasc Dis. 2016; 12. 41(5-6):306–312. PMID: 26881779.

9. Hui FK, Hussain MS, Elgabaly MH, Sivapatham T, Katzan IL, Spiotta AM. Embolic protection devices and the Penumbra 054 catheter: utility in tandem occlusions in acute ischemic stroke. J Neurointerv Surg. 2011; 3. 3(1):50–53. PMID: 21990789.

10. Jankowitz B, Grandhi R, Horev A, Aghaebrahim A, Jadhav A, Linares G, et al. Primary manual aspiration thrombectomy (MAT) for acute ischemic stroke: safety, feasibility and outcomes in 112 consecutive patients. J Neurointerv Surg. 2015; 1. 7(1):27–31. PMID: 24385557.
11. Lockau H, Liebig T, Henning T, Neuschmelting V, Stetefeld H, Kabbasch C, et al. Mechanical thrombectomy in tandem occlusion: procedural considerations and clinical results. Neuroradiology. 2015; 6. 57(6):589–598. PMID: 25404414.

12. Mbabuike N, Gassie K, Brown B, Miller DA, Tawk RG. Revascularization of tandem occlusions in acute ischemic stroke: review of the literature and illustrative case. Neurosurg Focus. 2017; 4. 42(4):E15.

13. Miteff F, Faulder KC, Goh AC, Steinfort BS, Sue C, Harrington TJ. Mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB): experience in 26 patients with acute cerebral artery occlusion. AJNR Am J Neuroradiol. 2011; Jun-Jul. 32(6):1078–1081. PMID: 21493763.
14. Mpotsaris A, Bussmeyer M, Buchner H, Weber W. Clinical outcome of neurointerventional emergency treatment of extra- or intracranial tandem occlusions in acute major stroke: antegrade approach with wallstent and solitaire stent retriever. Clin Neuroradiol. 2013; 9. 23(3):207–215. PMID: 23354342.

15. Mpotsaris A, Bussmeyer M, Loehr C, Oelerich M, Buchner H, Weber W. Mechanical thrombectomy in severe acute stroke: preliminary results of the Solitaire stent. J Neurol Neurosurg Psychiatry. 2012; 1. 83(1):117–118. PMID: 21212105.
16. Muller-Hulsbeck S, Schafer PJ, Charalambous N, Schaffner SR, Heller M, Jahnke T. Comparison of carotid stents: an in-vitro experiment focusing on stent design. J Endovasc Ther. 2009; 4. 16(2):168–177. PMID: 19456191.
17. Padalino DJ, Deshaies EM. Tandem middle cerebral artery-internal carotid artery occlusions: reduced occlusion-to-revascularization time using a trans-anterior communicating artery approach with a penumbra device. J Neurosurg. 2012; 3. 116(3):665–671. PMID: 22196094.

18. Perez MA, Miloslavski E, Fischer S, Bazner H, Henkes H. Intracranial thrombectomy using the Solitaire stent: a historical vignette. J Neurointerv Surg. 2012; 11. 4(6):e32. PMID: 22170823.
19. Rangel-Castilla L, Rajah GB, Shakir HJ, Shallwani H, Gandhi S, Davies JM, et al. Management of acute ischemic stroke due to tandem occlusion: should endovascular recanalization of the extracranial or intracranial occlusive lesion be done first. Neurosurg Focus. 2017; 4. 42(4):E16.

20. Shao Q, Zhu L, Li T, Wang Z, Li L, Bai W, et al. Management of tandem internal carotid and middle cerebral arterial occlusions with endovascular multimodal reperfusion therapy. Int J Neurosci. 2016; 12. 126(12):1077–1083. PMID: 26577278.

21. Sivan-Hoffmann R, Gory B, Armoiry X, Goyal M, Riva R, Labeyrie PE, et al. Stent-retriever thrombectomy for acute anterior ischemic stroke with tandem occlusion: a systematic review and meta-analysis. Eur Radiol. 2017; 1. 27(1):247–254. PMID: 27085698.

22. Spiotta AM, Lena J, Vargas J, Hawk H, Turner RD, Chaudry MI, et al. Proximal to distal approach in the treatment of tandem occlusions causing an acute stroke. J Neurointerv Surg. 2015; 3. 7(3):164–169. PMID: 24561885.

23. Weiner GM, Feroze R, Panczykowski DM, Aghaebrahim A, Ares W, Agarwal N, et al. Endovascular treatment of tandem common carotid artery origin and distal intracranial occlusion in acute ischemic stroke. World Neurosurg. 2017; 1. 97:360–365. PMID: 27751921.

Fig. 1
(A) Angiogram shows total occlusion of the right cervical ICA. (B) After partial balloon recanalization of the cervical ICA, the angiogram reveals MCA occlusion. (C) To improve proximal blood flow, the steno-occlusive carotid lesion is treated with an open-cell stent. (D) The Solitaire stent harboring the captured thrombus is caught in the open-cell carotid stent. Manipulation of a stiff guide wire around the Solitaire stent is ineffective. (E) A gross picture of the Solitaire stent capturing the thrombus. The captured thrombus renders the stent wide open, which results in subsequent complications. ICA = internal carotid artery; MCA = middle cerebral artery.
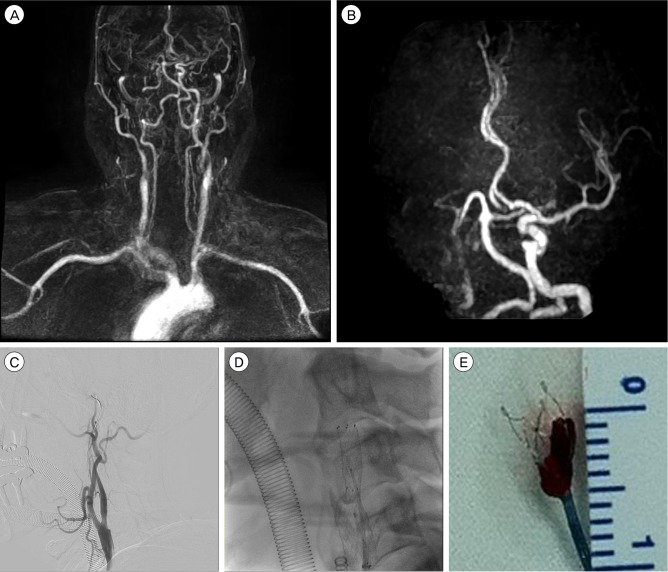
Fig. 2
(A) Initial angiogram shows total occlusion of the cervical ICA. (B) Using balloon angioplasty, this lesion is recanalized but still stenotic. MCA was still occluded after proximal recanalization. The MCA lesion was recanalized with mechanical thrombectomy using a Solitaire stent. However, after stent angioplasty for the cervical stenotic lesion using an open-cell stent, a thrombotic occlusion in the superior trunk of the MCA developed. Therefore, another mechanical thrombectomy using the Solitaire stent was performed. (C) This image shows that the Solitaire stent harboring the thrombus is caught in the distal end of the carotid stent during retrieval. (D) Complete recanalization can be observed after the complicated procedure. ICA = internal carotid artery; MCA = middle cerebral artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download