Abstract
Objectives
The aim of this study was to determine the relationship of ovarian volume (OV) to age, height, and weight in Korean young women with the polycystic ovary syndrome (PCOS) undergoing ultrasonography (US) and to investigate the relationship between ovarian follicle count and volume on US and serum hormone levels including the levels of the anti-Müllerian hormone (AMH) and gonadotropin.
Methods
A total of 272 Korean nulliparous women aged 15 to 39 years who were newly diagnosed with PCOS at a university hospital were included in this study. Evaluation of the ovaries and measurement of OVs in all cases were randomly performed by ultrasound. The OV and follicle number (FN) were obtained in all cases.
Results
In Korean women with PCOS, mean OV was 7.9 ± 3.6 cm3 (right) and 6.7 ± 3.1 cm3 (left). Mean FN in the PCOS group was 14.2 ± 4.6 (right) and 13.8 ± 4.3 (left). OV and ovarian FN were unrelated to patient weight, height and body mass index. The left ovarian FN was related to patient age. AMH levels ranged from 5.31 to 43.1 ng/mL and the mean level was 13.9 ± 7.2 ng/mL. Serum AMH was related to OV and FN, and serum total testosterone was related to FN in Korean women with PCOS.
Polycystic ovary syndrome (PCOS) is an etiologically heterogeneous condition which involves overproduction of ovarian androgens leading to a variable range of symptoms including hirsutism, acne, and anovulation.1 Ovarian morphology, especially the ovarian size / ovarian volume (OV) and number of pre-antral follicles, is the key and consistent feature of polycystic ovaries. There might be ethnic differences in the ovarian dimensions or morphology used to define PCOS among different populations.
OV and follicle number (FN) also decrease with age, with the age-related decrease in FN seemingly greater than that of OV.2
Women with PCOS are likely to have a higher antral follicle count and a greater OV. Women with PCOS have higher anti-Müllerian hormone (AMH) concentrations than controls, and a high serum AMH level is regarded as a useful tool for the diagnosis of PCOS; however, the associations between these inappropriate hormonal characteristics of PCOS and the increased OV remain unresolved.3456
In this study, we investigated the clinical and biochemical characteristics and measured OV and FN in Korean nulliparous women with PCOS.
Nulliparous female patients aged 15 to 39 years who first visited the hospital for irregular menstruation and were diagnosed with PCOS between January 2010 and December 2015 were included in the study. This study was approved by the Institutional Review Board of the Catholic University Hospital.
All PCOS patients were diagnosed using the following 2003 Rotterdam criteria (2 out of 3): 1) oligo-anovulation (menstrual cycle of > 35 days); 2) clinical and/or biochemical signs of hyperandrogenism; and 3) PCOS as identified by ultrasonography (US). PCOS on US was defined as follows: 1) the presence of ≥ 12 follicles in each ovary measuring 2 to 9 mm in diameter; and/or 2) increased OV (> 10 mL). Exclusion criteria for this study were as follows: a history of ovarian surgery; hormonal treatment in the previous 3 months or PCOS-related treatment before this research; and an ovarian mass or cyst (more than 10 mm in diameter) detected by ultrasound examination in this study. Age, parity, and body mass index (BMI) of all cases were recorded.
All PCOS subjects in Korea were examined by a single examiner (KMJ), and participants were evaluated by transrectal and transvaginal US according to their sexual activity.
Ultrasound examination was performed in all participants with Voluson S7 (General Electric Systems, Seongnam, Korea) equipped with a 7-MHz transvaginal transducer. For each ovary, the total number of visible antral follicles measuring 2 to 9 mm in diameter was counted by continuous scanning of the entire ovary, from the inner margin to the outer margin in longitudinal cross-section. The OV was calculated using the simplified formula for a prolate ellipsoid (0.5 × length × width × thickness).7 FN was established by scanning each ovary from the inner margin to the outer margin in longitudinal cross-section and obtaining the number of all countable follicles.
Blood samples were drawn for the determination of serum levels of total testosterone, free testosterone, androstenedione and dehydroepiandrosterone-sulfate (DHEA-S). The serum AMH level was measured using the AMH Gen II assay (Beckman Coulter Inc., Brea, CA, USA).
All the data were analyzed on a personal computer using the SPSS 13.0 for Windows statistical package (SPSS Inc., Chicago, IL, USA). The data are presented as proportion and mean ± standard deviation (SD). The Kruskal-Wallis test confirmed that the data were not normally distributed (and are presented as mean ± SD), and hence, the Student's t-test was used to compare the differences between the groups. Spearman's correlation was used to analyze the relationship between hormone assay and OV, and FN.
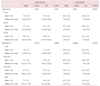
All target groups included young women who were premenopausal without the experience of delivery, and their average age was 23.6 ± 5.3 years. Women aged 20 to 29 years (n = 166) accounted for 61% of the study population (Table 1). The age of menarche was 13.8 ± 1.9 years, average height was 161.3 ± 5.9 cm, body weight was 59.8 ± 13.2 kg, and BMI was 23.0 ± 5.0 kg/m2. Among the overall women in the cohort, the proportion of obese women whose BMI was more than 25 was 25.3%. Further, 94.1% of the women had menstrual irregularity and the average duration of menstrual cycle was 6.2 ± 2.2 days. Also, 70.2% of the women had experienced dysmenorrhea.
On comparison of bilateral OV and FN, the right OV was 7.9 ± 3.6 cm3, and FN was 14.2 ± 4.6. The average left OV was 6.7 ± 3.1 cm3, and FN was 13.8 ± 4.3.
There was no effect on bilateral OV according to age and BMI, and ovarian FN was not affected by BMI. However, left ovarian FN was significantly decreased (P = 0.0343) with increasing age. In all women included in our study, the right OV was significantly larger than the left OV (P < 0.0001; Table 2).
In our study, the average AMH level was 13.9 ± 7.2 ng/mL, total testosterone level was 66.2 ± 35.6 ng/dL, free testosterone level was 1.3 ± 0.9 ng/dL, DHEA-S level was 206.0 ± 106.3 ug/dL, sex hormone-binding globulin (SHBG) level was 37.0 ± 20.3 nmol/L, and 17-hydroxyprogesterone (OHP) level was 1.38 ± 0.54 ng/mL. The study also evaluated the correlation between hormone level and OV, and OV and AMH had a positive relationship (Right [Rt.] OV: r = 0.4, Left [Lt.] OV: r = 0.314; Table 3). Bilateral ovarian follicles and total testosterone (Rt. OV: r = 0.354, Lt. OV: r = 0.364), and AMH (Rt. OV: r = 0.607, Lt. OV: r = 0.381) had a significantly positive correlation (Table 4).
PCOS is the most common female endocrine disease, affecting 5% to 10% of the female population. OV and FN differed among various ethnic subgroups of women, and the differences could not be explained by age or BMI. In another study by Welt et al.3, OV and FN were found to be higher in African-American than Asian women and FN was higher in Caucasian than Asian women with PCOS. They concluded that phenotypic differences in different populations may indicate genetic variability, or may point to genetic or environmental modifiers of the PCOS phenotype in different ethnic groups.8
OV rises through childhood and adolescence and is maximal in the average woman at 20 years of age, declining thereafter towards the menopause and beyond.
Kelsey et al.9 studied that in the average case OV rises from 0.7 mL (95% CI: 0.4-1.1 mL) at 2 years of age to a peak of 7.7 mL (95% CI: 6.5-9.2 mL) at 20 years of age with a subsequent decline to about 2.8 mL (95% CI: 2.7-2.9 mL) at the menopause and smaller volumes thereafter.
Alsamarai et al.10 concluded that OV and FN decrease with age in women with PCOS. Christensen et al.11 found that OV was not related to age in 428 healthy women aged between 18 and 45 years. In Chinese study12, they found a moderate negative correlation of age with OV, suggesting that there are no major changes in OV during reproductive ages until the perimenopause. In our study, we could not identify any relationship between age and OV in the PCOS group. This may be due to selection of nulliparous women under 40 years in the study.
Mean OV was statistically larger in PCOS patients than in the control group, but there was no significant difference between the non-obese and obese women with PCOS.13 In our study, there was no difference between OV, ovarian FN and weight, height, and BMI, and this result was due to the inclusion of young nulliparous women.
The threshold for distinguishing polycystic ovaries from normal ovaries varied from 8 to 17.6 cm3 among different studies.141516 The main reason for this may be the difference in methods used to determine the OV, or difference in ethnicity. There is also some controversy about the use of FN as an ultrasound predictor of PCOS. But most studies that use FN for the diagnosis of PCOS have set the threshold at 10.14 In our Korean women with PCOS, the right OV was 7.9 ± 3.6 cm3 and the left OV was 6.7 ± 3.1 cm3. Our results showed that the OV was smaller than that in a previous study (Lee et al.'s study17 [8.8 ± 4.4 cm3]) and Rotterdam criteria. Right ovarian FN was 14.2 ± 4.6 and left ovarian FN was 13.8 ± 4.3, and ovarian FN was adequate to diagnose PCOS in Korean women. In a Turkish study, they found that 6.43 cm3 was a diagnostic threshold of OV for Turkish women with PCOS, which is a lower diagnostic threshold in comparison to the Rotterdam criteria,16 and this indciates the means difference in ethnicity in the diagnosis of PCOS. Our study shows that FN is a good parameter for the diagnosis of PCOS.
AMH is regarded as the most useful marker of the status of ovarian reserve,18 and a highly significant relationship between the serum AMH level and ovarian FN on US was reported in numerous studies.3619 The pathogenesis of PCOS has been cased mainly to disordered folliculogenesis causing oligo-ovulatory cycles or impaired folliculogenesis with increased preantral and small antral follicle counts, which resulted in high serum AMH levels.20 Although several cutoff values of AMH have been proposed, the optimal threshold remains unclear due to varying sensitivity and specificity. In our study, AMH levels were positively correlated with the OV (Rt. OV: r = 0.40, P = 0.002, Lt. OV: r = 0.314, P = 0.019) although the OV was smaller than that mentioned in the Rotterdam criteria.
The present study showed a positive correlation between the serum AMH level and OV, and ovarian FN in women with PCOS. Yoo et al.19 reported that the AMH levels are significantly correlated with the OV in Korean women with PCOS.
There is a good correlation between AMH levels and the number of small follicles as well as OV. The level of AMH is higher in patients with PCOS, which can be helpful in the diagnosis of this syndrome.2021 Due to the use of various methods to analyze plasma AMH levels, it is difficult to compare previous studies and specify diagnostic norms that would be characterized by high sensitivity and specificity for patients with the features of PCO.1820
The serum AMH levels were also positively associated with testosterone levels and OV.22 It has been suggested that testosterone is the most sensitive androgen measurement and it is often measured when conducting clinical research studies in women with PCOS.23 Larger OVs and FNs correlated with higher serum testosterone and androstenedione levels and these suggest that FN on ultrasound and related OV are associated with hyperandrogenic state in women with PCOS.
In our study, the average serum level of total testosterone was 66.2 ± 35.6 ng/dL, free testosterone level was estimated to be 1.3 ± 0.8 ng/dL, mean OV was 7.9 ± 3.6 cm3 (Rt.), 6.7 ± 3.1 cm3 (Lt.), and follicle count was 14.2 ± 4.6. As a result of the AMH test, mean serum density was 13.9 ± 7.2 ng/mL and tehse results correlated with Welt's study.3
Our study attempted to provide Korean PCOS data on AMH and to establish the relevance between AMH and clinical and biochemical characteristics of PCOS, and serum AMH level was related to both total testosterone and ovarian morphology under sonography.
The measurement of AMH is an important marker of ovarian ageing, but it has not been shown to be helpful in assessing ovarian reserve in the individual.
The present study has limitations that mostly stem from its retrospective study design and a relatively small sample size and nulliparous women without experience of pregnancy.
In conclusion, our study showed that the serum AMH was significantly correlated with the OV and total testosterone and the serum AMH level were related to the ovarian FN in Korean women with PCOS. These results suggest that serum total testosterone and AMH are more useful to represent the status of the OV and FN in women with PCOS. Also, ovarian FN is a more important diagnostic predictor in the diagnosis of PCOS in Korean women. Further prospective large-scale trials are needed to confirm this preliminary finding.
Figures and Tables
Acknowledgement
The statistical consultation was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI14C1062).
This study was supported by Department of Obstetrics and Gynecology, The Catholic University of Korea.
References
1. Homburg R. Polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2008; 22:261–274.
2. Hsu MI. Changes in the PCOS phenotype with age. Steroids. 2013; 78:761–766.
3. Welt CK, Arason G, Gudmundsson JA, Adams J, Palsdóttir H, Gudlaugsdóttir G, et al. Defining constant versus variable phenotypic features of women with polycystic ovary syndrome using different ethnic groups and populations. J Clin Endocrinol Metab. 2006; 91:4361–4368.
4. Ehrmann DA, Kasza K, Azziz R, Legro RS, Ghazzi MN. Effects of race and family history of type 2 diabetes on metabolic status of women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2005; 90:66–71.
5. Kumar A, Woods KS, Bartolucci AA, Azziz R. Prevalence of adrenal androgen excess in patients with the polycystic ovary syndrome (PCOS). Clin Endocrinol (Oxf). 2005; 62:644–649.
6. Carmina E, Chu MC, Longo RA, Rini GB, Lobo RA. Phenotypic variation in hyperandrogenic women influences the findings of abnormal metabolic and cardiovascular risk parameters. J Clin Endocrinol Metab. 2005; 90:2545–2549.
7. Carmina E, Koyama T, Chang L, Stanczyk FZ, Lobo RA. Does ethnicity influence the prevalence of adrenal hyperandrogenism and insulin resistance in polycystic ovary syndrome? Am J Obstet Gynecol. 1992; 167:1807–1812.
8. Vink JM, Sadrzadeh S, Lambalk CB, Boomsma DI. Heritability of polycystic ovary syndrome in a Dutch twin-family study. J Clin Endocrinol Metab. 2006; 91:2100–2104.
9. Kelsey TW, Dodwell SK, Wilkinson AG, Greve T, Andersen CY, Anderson RA, et al. Ovarian volume throughout life: a validated normative model. PLoS One. 2013; 8:e71465.
10. Alsamarai S, Adams JM, Murphy MK, Post MD, Hayden DL, Hall JE, et al. Criteria for polycystic ovarian morphology in polycystic ovary syndrome as a function of age. J Clin Endocrinol Metab. 2009; 94:4961–4970.
11. Christensen JT, Boldsen J, Westergaard JG. Ovarian volume in gynecologically healthy women using no contraception, or using IUD or oral contraception. Acta Obstet Gynecol Scand. 1997; 76:784–789.
12. Ng EH, Yeung WS, Fong DY, Ho PC. Effects of age on hormonal and ultrasound markers of ovarian reserve in Chinese women with proven fertility. Hum Reprod. 2003; 18:2169–2174.
13. Zhang HY, Guo CX, Zhu FF, Qu PP, Lin WJ, Xiong J. Clinical characteristics, metabolic features, and phenotype of Chinese women with polycystic ovary syndrome: a large-scale case-control study. Arch Gynecol Obstet. 2013; 287:525–531.
14. Yeh HC, Futterweit W, Thornton JC. Polycystic ovarian disease: US features in 104 patients. Radiology. 1987; 163:111–116.
15. Atiomo WU, Pearson S, Shaw S, Prentice A, Dubbins P. Ultrasound criteria in the diagnosis of polycystic ovary syndrome (PCOS). Ultrasound Med Biol. 2000; 26:977–980.
16. Köşüş N, Köşüş A, Turhan NÖ, Kamalak Z. Do threshold values of ovarian volume and follicle number for diagnosing polycystic ovarian syndrome in Turkish women differ from western countries? Eur J Obstet Gynecol Reprod Biol. 2011; 154:177–181.
17. Lee DE, Park SY, Lee SR, Jeong K, Chung HW. Diagnostic usefulness of transrectal ultrasound compared with transvaginal ultrasound assessment in young Korean women with polycystic ovary syndrome. J Menopausal Med. 2015; 21:149–154.
18. You SY, Park SY, Yang GY, Jeong KA, Kim YJ, Chung HW. Anti-Müllerian hormone in women with polycystic ovary syndrome. Korean J Obstet Gynecol. 2012; 55:315–324.
19. Yoo JH, Kim HO, Cha SW, Park CW, Yang KM, Song IO, et al. Age specific serum anti-Müllerian hormone levels in 1,298 Korean women with regular menstruation. Clin Exp Reprod Med. 2011; 38:93–97.
20. La Marca A, Broekmans FJ, Volpe A, Fauser BC, Macklon NS. Anti-Mullerian hormone (AMH): what do we still need to know? Hum Reprod. 2009; 24:2264–2275.
21. Wachs DS, Coffler MS, Malcom PJ, Chang RJ. Serum anti-mullerian hormone concentrations are not altered by acute administration of follicle stimulating hormone in polycystic ovary syndrome and normal women. J Clin Endocrinol Metab. 2007; 92:1871–1874.
22. Carlsen SM, Vanky E, Fleming R. Anti-Müllerian hormone concentrations in androgen-suppressed women with polycystic ovary syndrome. Hum Reprod. 2009; 24:1732–1738.
23. Robinson S, Rodin DA, Deacon A, Wheeler MJ, Clayton RN. Which hormone tests for the diagnosis of polycystic ovary syndrome? Br J Obstet Gynaecol. 1992; 99:232–238.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download