Abstract
We report a non-puerperal uterine inversion with nulliparous women caused by huge pedunculated submucosal fibroid. Massive bleeding from protruding mass through vagina brought the heart to stop in 42-year-old nulliparous woman. She became cardiopulmonary resuscitation survivor in emergency room and then underwent laparotomy which ended in successful myomectomy rather than hysterectomy considering her demand for future fertility. Meticulous and adequate fluid therapy and transfusion was also administered to recover from hypovolemic status. Pathologic report confirmed benign submucosal fibroid with degeneration, necrosis and abscess formation. Thus, clinician should be aware of uterine inversion when encountered with huge protruding vaginal mass and consider uterus-preserving management as surgical option when the future fertility is concerned.
Uterine inversion is briefly depicted as the indentation and depression of the fundus extending downwards up to the various levels of the vaginal canal. It is a rare entity experienced in two different conditions; puerperal or non-puerperal. Non-puerperal inversion occurs less frequently limited to case reports in postmenopausal women and it is associated with the traction effect of mass lesions, such as benign submucosal myoma.1 It also occurs when other endometrial pathology exist in uterus such as endometrial carcinoma, sarcoma or endometrial polyp.2 Mechanism of possible explanations could be a thin uterine wall, rapid growth of the fundal location of the tumor with the dilatation of the cervix. The authors report non-puerperal uterine inversion presented with hypovolemic shock.
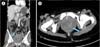
A 42-year-old nulliparous woman with pulseless heart activity was brought into the emergent department of Pusan National University Yangsan Hospital possibly due to hypovolemia from protruding vaginal mass with active bleeding. She successfully got return of spontaneous circulation after 5 minutes of cardiopulmonary resuscitation (CPR) and the gynecologist on call was soon called for evaluation. A maximum 22 cm wide solid mass that was ulcerative and necrotic from its surface was identified and presumptive diagnosis of uterine prolapse was made. Her laboratory findings revealed hemoglobin of 3 g/dL with leucocytosis. After six units of blood were transfused, her vital signs became stable soon. After securing hemodynamic stability, computed tomography (CT) revealed a submucosal fibroid of 19 × 10 cm in size (Fig. 1A) with extravasation of contrast media at 5 o'clock of the mass (Fig. 1B). She soon underwent emergent explorative laparotomy and the huge necrotic mass was protruding from the vaginal introitus (Fig. 2A). Bilateral ovaries and fallopian tubes were intact and the concave inverted uterus filled the pelvic cavity without visualization of uterine fundus (Fig. 2B). Pedunculated mass could not be resected through vagina and uterine inversion was not restored manually. So the pedunculated mass at fundus was resected at the neck of its stalk after uterus was opened by vertical incision. We repaired the myometrium by double layer suture for her future fertility. For furthering prophylactic bleeding control that might follow after surgery, bilateral internal iliac arteries were ligated. Gross finding of bilateral adnexa was free and we finished the surgery after securing Jackson-Pratt drainage catheter in pelvis.
Postoperative course was uneventful including 3-day stay in an intensive care unit. Pathologic report demonstrated the degenerated the 22 × 11.5 × 5.8 cm sized submucosal fibroid with abscess and necrosis in serosa which was consistent with the preoperative findings (Fig. 3). On postoperative day 11th, she was discharged without complication. Wound was healed clearly and she denied any complaints at the time of discharge and so far following up. She restore menstruation at 2 months after operation.
The majority of uterine inversion has relation with the delivery of placenta in the third stage of labor.1 However, there was a few reports about uterine inversion in non-puerperal women.2,3 Pulling power from intrauterine masses such as fibroids, sarcomas and carcinomas might cause fundal inversion chronically. Uterine leiomyoma are known to cause inversion in 78% to 85% of cases.4 In most cases, patients came to the emergent department with complaints of vaginal mass with bleeding. Most cases of uterine inversion were multiparous women, however, our case was nulliparous. The extremely large size of the pedunculated submucosal myoma over 20 cm was the possible explanation in this case. Clinical presentations of non-puerperal uterine inversion include vaginal bleeding, mass descending through the introitus, and lower abdominal pain.5 Our case present a most aggressive way other than classic courses of chronic non-puerperal uterine inversion because she had hypovolemic shock due to massive bleeding and had received CPR at emergent room. Some reported intra-abdominal uterine inversion of which diagnosis was made after pelvic magnetic resonance imaging (MRI).6 However, in most cases so far reported the diagnosis was obvious only with visual inspection of protruding mass whatever the exact pathologic diagnosis of it was. CT is not used as the first line examination in such pelvic masses, but it can be an option in conditions that MRI is not possible as our case. Contrast enhanced examination is helpful for delineation of uterine inversion and for searching the sites of bleeding.
There were various methods in the literature suggested different procedures to reposition the non-puerperal uterine inversion after enucleating the fibroid.7 This could be accomplished by either vaginal or abdominal route followed by hysterectomy. Preserving fertility by saving uterus may not be applicable to all other cases. Considering that our patient was nulliparous woman, malignancies such as leiomyosarcoma is rare disease in its incidence, and intraoperative finding was not suggestive of malignancy influenced our decision of mass resection and myometrial repair instead of hysterectomy. Just like other gynecologic condition, hysterectomy should be meticulously decided even in managing in such a critical clinical setting. Many cases of uterine inversion were occurred in multiparous and postmenopausal women. Hysterectomy may be the last consideration in this situation, if the patients want preserving uterus due to worrying about sexual function or loss her femininity.7 Rathod et al.2 reported vaginal myomectomy for chronic uterine inversion due to benign fibroid in more hemodynamically stable young patient who desired future pregnancy. Uterine inversion in non-puerperal is a quite rare complication but it might be accompanied with severe bleeding enough to cause resuscitation. We report a case of non-puerperal uterine inversion in nulliparous women with preserving uterus after successful CPR due to massive hemorrhage. Clinicians should be aware of uterine inversion when encountered with huge protruding vaginal mass and must consider uteruspreserving operative management when the future fertility is concerned. Also, uterus could be preserved using technique of our case even in postmenopausal women, if the patients want to conserve uterus.
Figures and Tables
Fig. 1
Coronal plane on contrast enhanced computed tomography (CT) revealed the prolapsed mass in the uterus and retraction of fundus. (B) Axial plain on contrast enhanced CT revealed extravasation of contrast media (arrow), suggestive of active bleeding from the mass in the uterus.
References
1. Eigbefoh JO, Okogbenin SA, Omorogbe F, Mabayoje PS. Chronic uterine inversion secondary to submucous fibroid: a case report. Niger J Clin Pract. 2009; 12:106–107.
2. Rathod S, Samal SK, Pallavee P, Ghose S. Non puerperal uterine inversion in a young female- a case report. J Clin Diagn Res. 2014; 8:OD01–OD02.
3. Kulkarni KK, Ajmera SK. A rare case of non-puerperal acute uterine inversion. J Obstet Gynaecol India. 2014; 64:364–365.
4. Lupovitch A, England ER, Chen R. Non-puerperal uterine inversion in association with uterine sarcoma: case report in a 26-year-old and review of the literature. Gynecol Oncol. 2005; 97:938–941.
5. Krenning RA. Nonpuerperal uterine inversion. Review of literature. Clin Exp Obstet Gynecol. 1982; 9:12–15.
6. Mihmanli V, Kilic F, Pul S, Kilinc A, Kilickaya A. Magnetic resonance imaging of non-puerperal complete uterine inversion. Iran J Radiol. 2015; 12:e9878.
7. Simms-Stewart D, Frederick S, Fletcher H, Char G, Mitchell S. Postmenopausal uterine inversion treated by subtotal hysterectomy. J Obstet Gynaecol. 2008; 28:116–117.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download