Abstract
Purpose
This study was conducted to objectively and subjectively compare the accuracy and reliability of 2-dimensional (2D) photography and 3-dimensional (3D) soft tissue imaging.
Materials and Methods
Facial images of 50 volunteers (25 males, 25 females) were captured with a Nikon D800 2D camera (Nikon Corporation, Tokyo, Japan), 3D stereophotogrammetry (SPG), and laser scanning (LS). All subjects were imaged in a relaxed, closed-mouth position with a normal smile. The 2D images were then exported to Mirror® Software (Canfield Scientific, Inc, NJ, USA) and the 3D images into Proplan CMF® software (version 2.1, Materialise HQ, Leuven, Belgium) for further evaluation. For an objective evaluation, 2 observers identified soft tissue landmarks and performed linear measurements on subjects' faces (direct measurements) and both linear and angular measurements on all images (indirect measurements). For a qualitative analysis, 10 dental observers and an expert in facial imaging (subjective gold standard) completed a questionnaire regarding facial characteristics. The reliability of the quantitative data was evaluated using intraclass correlation coefficients, whereas the Fleiss kappa was calculated for qualitative data.
Results
Linear and angular measurements carried out on 2D and 3D images showed excellent inter-observer and intra-observer reliability. The 2D photographs displayed the highest combined total error for linear measurements. SPG performed better than LS, with borderline significance (P=0.052). The qualitative assessment showed no significant differences among the 2D and 3D imaging modalities.
Soft tissue evaluation is an important component of dentomaxillofacial diagnoses, treatment planning, treatment outcome monitoring, and postoperative follow-up.12345 The methods that have been used to assess soft tissue morphology can be classified as direct or indirect anthropometry.3 The reliability of direct anthropometry and its application as a gold standard have already been validated, but it has certain limitations; for example, it is time-consuming and invasive, and requires patient cooperation.36 Indirect anthropometry techniques such as 2-dimensional (2D) and 3-dimensional (3D) surface imaging have been utilized to overcome the limitations associated with direct methods.
Over the past decade, advances in 3D surface capturing techniques have become an area of interest in the field of facial imaging. Unlike 2D imaging, which requires multiple photographs for soft tissue assessment, similar information can be obtained from a single 3D image. The two most commonly utilized 3D surface imaging technologies are 3D laser scanning (LS) and stereophotogrammetry (SPG). Several studies have proven the reliability and accuracy of these modalities for soft tissue evaluation.57891011 Unlike LS, SPG has a fast acquisition time, thereby eliminating inaccuracies related to motion artefacts. The availability of 3D imaging systems offers a possibility to perform automated 3D facial analyses, and these systems have been widely applied in the fields of prosthodontics, dental implantology, orthodontics and maxillofacial surgery.41213
Recently, some studies have quantitatively validated the application of 3D imaging systems, mainly focusing on SPG, LS, and structured light scanning.141516 However, only a few studies have compared 3D imaging systems to each other and to direct anthropology or 2D imaging systems.3171819 To our knowledge, quantitative and qualitative comparisons of SPG, LS, and 2D images with direct anthropometry as a gold standard have not yet been reported in the literature. Therefore, the aim of this study was to conduct a comparative evaluation of the objective and subjective reliability and accuracy of 3D imaging modalities versus standard 2D facial photography.
After receiving ethical approval (reference no: B32220 1316317) from the Ethical Review Board of the University Hospitals Leuven, Belgium, 50 healthy Caucasian subjects (25 males, 25 females) were recruited for the study. All participants provided written informed consent. The exclusion criteria were maxillofacial abnormalities and excess facial hair, which might disguise anatomical landmarks.18
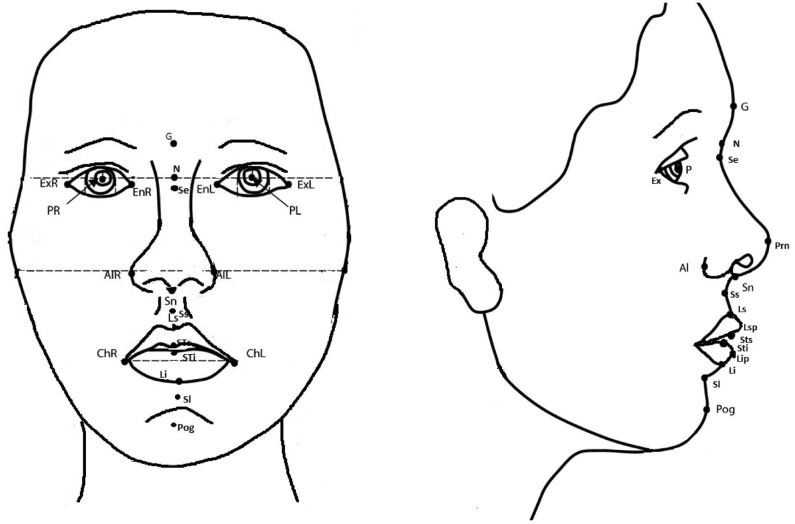
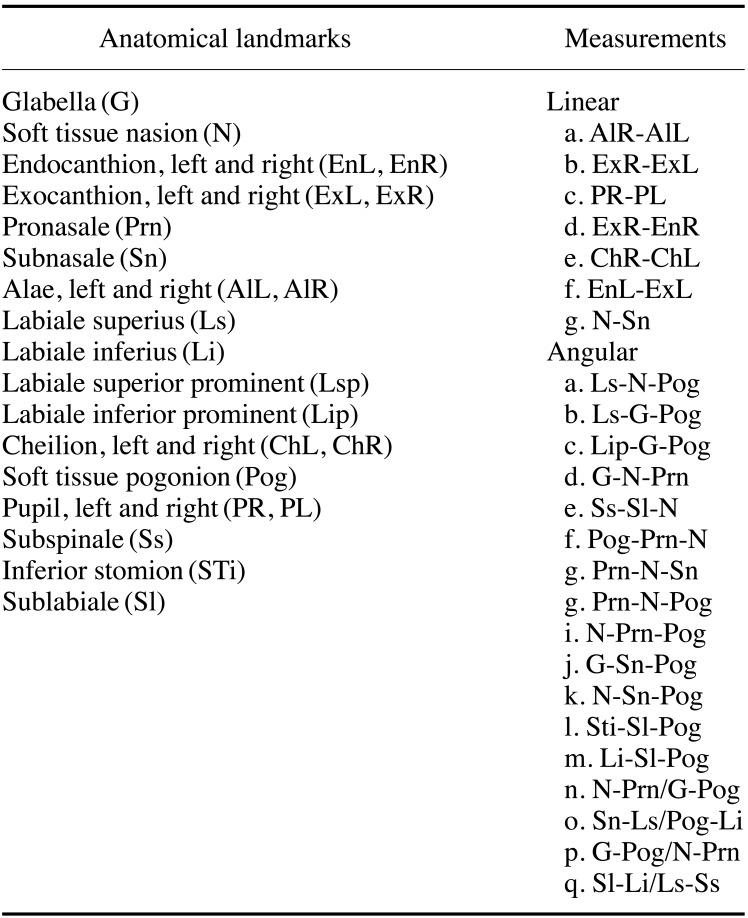
Participants were seated in a natural head position with relaxed lips and a closed mouth. Soft tissue anatomical landmarks were then marked on their faces directly following inspection and palpation for linear measurements (Table 1, Fig. 1). Direct anthropometry acted as a gold standard for evaluating linear distances in relaxed facial expressions in comparison to indirect techniques. Pupillary distance was assessed directly without placing any marks.
Two sets of 2D and 3D pictures images were collected from all participants. The images were taken with participants in a relaxed position, with a closed mouth and a normal smile. Before the images were captured, subjects were positioned in a natural head posture.20 After capture, the images were checked, and image acquisition was repeated if they were blurred, too bright, not well oriented, or missing a part, or if the subject had his/her eyes closed. The indirect techniques utilized to capture images included 2D, SPG, and LS imaging systems.
In a clinical setup, 2D photographs were acquired (Fig. 2A) with a professional camera (Nikon D800; Nikon Corporation, Tokyo, Japan). The image capturing process was standardized by utilizing a reproducible set-up of a camera, tripod, and chair with a fixed distance to the camera lens. An L-shaped ruler was placed to the upper right of the individuals for calibration. For each subject, a total of 5 relaxed non-smiling pictures and 5 pictures with a normal smile (frontal, left oblique, right oblique, and lateral) were acquired. Thereafter, images were exported to Mirror® Software (Canfield Scientific, Inc, NJ, USA) in JPEG format for evaluation.
All subjected were scanned twice (relaxed position and normal smile) utilizing Planmeca ProFace™, which is a 3D facial scanning protocol integrated within the ProMax® 3D Mid (Planmeca OY, Helsinki, Finland) CBCT machine. Before the image was captured, each participant's head was fixed and the chin was placed on a chin-support to avoid distortion. Volunteers were asked to remove any objects (glasses, jewellery) that might potentially cause artefacts from light reflection during the scan of the head and neck region. All images were saved and exported in the OBJ file format to Proplan CMF® 2.1 (Materialise HQ, Leuven, Belgium) for assessment (Fig. 2B). Thereafter, a quantitative and qualitative assessment was conducted of all 2D and 3D images after the observers were trained and calibrated. All observations were performed under standardized conditions on the same computer.
Three-dimensional stereophotogrammetric images with a relaxed facial expression and normal smile were acquired using a portable 3D Vectra® H1 (Canfield Scientific Inc., Parsippany, NJ, USA) camera after calibration of the device. This 3D camera consisted of a stereo-optic system with ranging lights for easy patient positioning and had an on-board modular intelligent flash unit. It provided images with a 0.8-mm geometry resolution and had a 165 mm×270 mm×100 mm (x, y, z) capture volume and a capture time of 2.0 ms.21 Three pictures were taken for each participant, which were than stitched into a single 3D image utilizing VECTRA® Face Sculptor® software (Fig. 2C). For each capture, subjects were asked to remain stable. The first image was captured by holding the camera at the patient's chest level (30 cm below the mid-face and angled upward) and positioning it at a 45° angle from the front towards the right side of the face. The second image was acquired from the front, with the camera held at level of the patient's nose and positioned directly in front of the patient. The third image was captured for the left side by following the same protocol as used for the right side. After stitching, images were exported in the OBJ file format to Proplan CMF® 2.1 software (Materialise HQ, Leuven, Belgium) for further evaluation.
Two observers identified soft tissue landmarks and performed linear measurements on subjects' faces directly (as an objective gold standard) and both linear and angular measurements indirectly on the images captured using 2D and 3D imaging modalities. Direct anthropometry involved the measurement of linear distances on patients in a relaxed, closed-mouth position using a digital sliding calliper in a well-illuminated room. In contrast, both linear and angular measurements were performed after identifying soft tissue anatomical landmarks on 2D and 3D images (Table 1, Fig. 1). All images were landmarked and assessed twice by each observer at an interval of 4 weeks to determine inter-observer and intra-observer reliability.
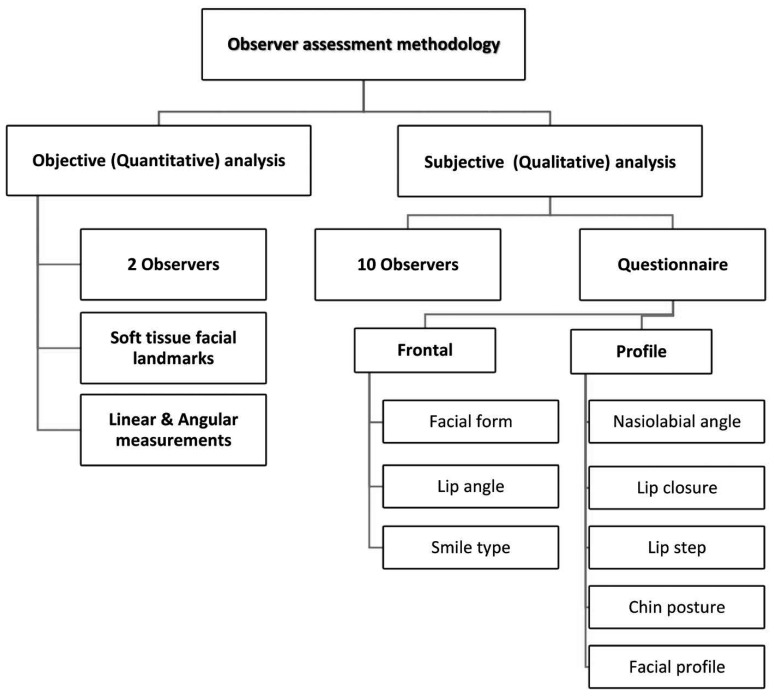
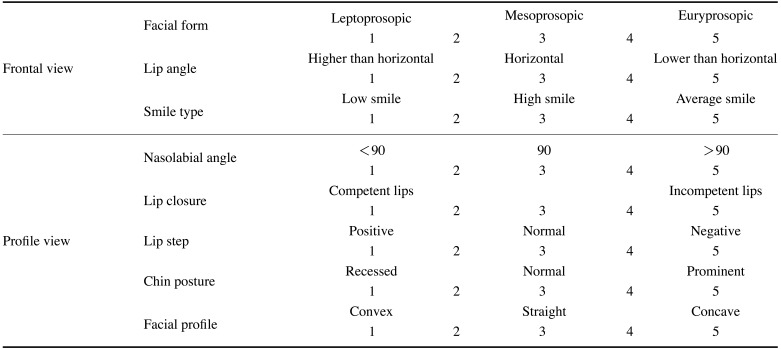
For the qualitative analysis, 10 dental observers and 1 expert (subjective gold standard) experienced in facial imaging completed a questionnaire (Table 2) related to facial characteristics on 2D and 3D images twice at an interval of 4 weeks for calculating inter-observer and intra-observer reliability. Respondents used a 5-point Likert scale to assess their confidence level for each given answer (1: not confident at all, 2: somewhat confident, 3: neutral, 4: confident 5: very confident). Figure 3 illustrates the flowchart for both the quantitative and qualitative assessments.
Data analysis was performed utilizing S-Plus 8.0 for Linux (Tibco, Palo Alto, CA, USA). Inter-observer and intra-observer agreement for quantitative data was estimated using intraclass correlation coefficients (ICCs), where <0.40, poor; 0.40–0.59, fair; 0.60–0.74, good; and 0.75–1.00, excellent.22 A bootstrapped sample was acquired, and the overall standard error was calculated for the quantitative analysis of linear measurements with direct anthropometry as the gold standard, and for analysing angular and linear differences between all indirect imaging modalities.
For the qualitative analysis, the Fleiss kappa index was applied to assess agreement between and within observers (<0.00, poor agreement; 0.00–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–1.00, almost perfect agreement).23 Confidence scores were compared between imaging techniques using a linear mixed model with the observer as random factor. Furthermore, the observers' scoring was compared to that of an expert and the significance of differences was calculated. A P value of <0.05 was considered to indicate statistical significance for both the quantitative and qualitative data.
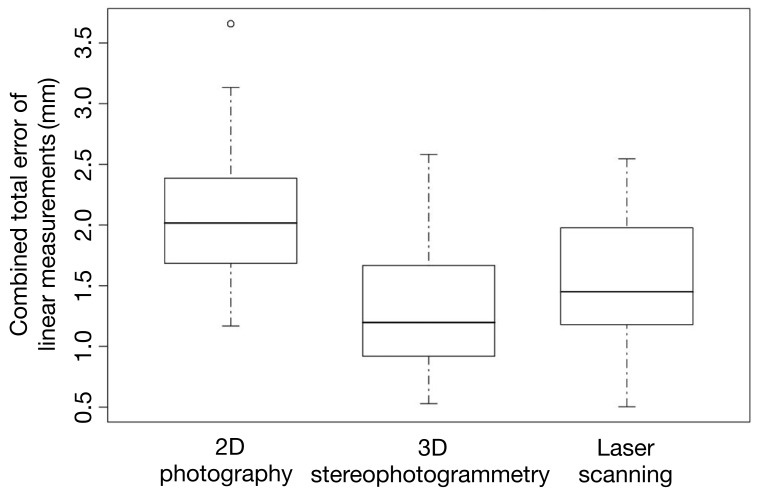
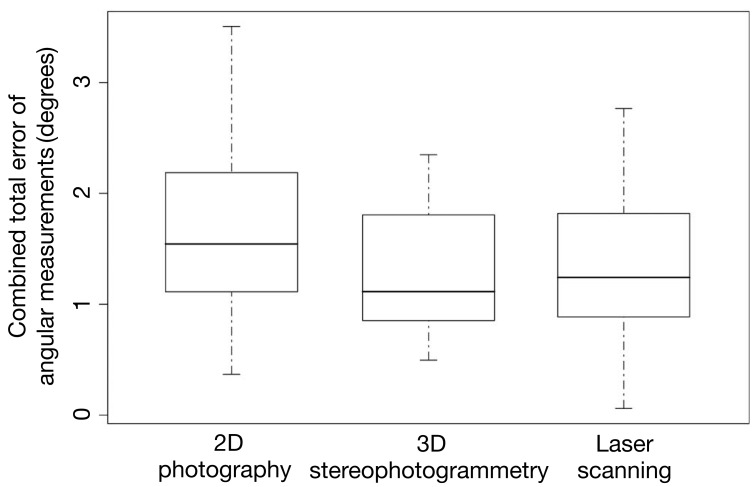
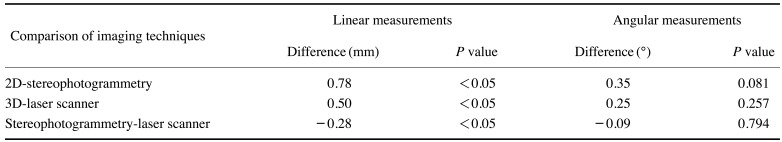
Residual analysis using a normal quantile plot showed that the basic assumption of residual normality was met. The measurements made through both direct and indirect anthropometry showed excellent inter-observer (ICCs, 0.96–0.99) and intra-observer reliability (ICCs ≥0.99). In comparison to direct anthropometry, 2D imaging showed the highest overall combined error for linear measurements. In contrast, SPG showed the least amount of error (Fig. 4). As shown in Table 3, both 3D imaging systems showed significantly less error for linear measurements than 2D imaging (P<0.05) and SPG was more accurate than LS, with borderline significance (P=0.052). For angular measurements, SPG was also more accurate than 2D imaging and LS (Fig. 5), but no significant difference was observed (P>0.05).
For qualitative assessments, the Fleiss kappa analysis showed overall moderate inter-observer agreement (kappa, 0.46–0.52) and substantial intra-observer agreement (kappa, 0.71-0.73) for all imaging modalities. Both the expert's and observers' opinions favoured SPG and LS over 2D imaging. However, no significant difference in the confidence scores was noted between imaging modalities.
The present study compared the quantitative and qualitative reliability and accuracy of two different 3D imaging technologies and 2D imaging. In the quantitative analysis, the 2D and 3D imaging systems all showed excellent inter-observer and intra-observer agreement. The highest error rate compared to direct anthropometry was found for 2D imaging. The qualitative assessment showed no significant differences among the 2D and 3D imaging systems.
Laser scanning has been previously compared to direct measurements.2717 Aung et al. suggested that LS was reliable around the nose, circumoral, and orbital regions. Weinberg et al. also found that LS showed very high precision and good agreement with direct anthropometry.219 Zogheib et al. compared 2D imaging and laser scanning to direct measurements and found that linear measurements with LS were closer to the clinical standard than measurements made with 2D imaging, while in the present study, SPG had significantly less error than both 2D and LS.24 The images captured with LS showed distortions around the eye region, and the measurements had higher variability than those obtained using SPG, even though it was lower than the variability of 2D imaging. This variability in LS accuracy could have resulted from motion artefacts owing to patient movement, facial expressions, or eye distortion caused by the blinking reflex.19
For soft tissue evaluation, it is crucial to have a realistic and complete representation of the face. To achieve this, SPG has been highly recommended based on its precision and high-quality output.141925 De Menezes et al. reported that SPG was reliable and reproducible for most the linear distances, in accordance with the findings of the present study.26 Dindaroglu et al. compared 2D imaging and stereophotogrammetry with direct anthropometry and found that the highest mean difference was lower for 3D imaging than for 2D imaging based on comparisons with direct measurements, which also aligns with our findings.3 Even though quantitative studies exist in the literature, these devices have barely been compared in a qualitative manner.242728 Stebel et al. qualitatively compared 2D and 3D stereophotogrammetry images to evaluate nasolabial aesthetics and found that SPG was more reliable and informative than 2D imaging, which corresponds with our findings.28 However, in our study, the observers were more confident with LS than with 2D images, in contrast with the findings of Zogheib et al.24
The main limitations of this study are related to laser scanning, such as motion artefacts in the orbital region related to the blinking reflex, the application of chin support, and a long capture process, which might have influenced the results.12729 To overcome these limitations, we recommend utilizing marker-free fixed 3D stereophotogrammetric systems such as the 3D Vectra® H1, 3dMDface™ (3dMD LLC, Atlanta, USA) and Di3D™ (Dimensional Imaging, Glasgow, UK) imaging systems.30 The reliability of the subjective observations might have been affected by the experience and relatively small number of the observers. Furthermore, subjective aesthetic evaluations were not included in the qualitative analysis, but should be incorporated in future soft tissue anthropometric studies.
In conclusion, stereophotogrammetry was found to be a reliable and accurate tool for the morphological evaluation of soft tissue in comparison to 2D imaging and laser scanning.
References
1. Germec-Cakan D, Canter HI, Nur B, Arun T. Comparison of facial soft tissue measurements on three-dimensional images and models obtained with different methods. J Craniofac Surg. 2010; 21:1393–1399. PMID: 20856027.

2. Weinberg SM, Scott NM, Neiswanger K, Brandon CA, Marazita ML. Digital three-dimensional photogrammetry: evaluation of anthropometric precision and accuracy using a Genex 3D camera system. Cleft Palate Craniofac J. 2004; 41:507–518. PMID: 15352857.

3. Dindaroğlu F, Kutlu P, Duran GS, Görgülü S, Aslan E. Accuracy and reliability of 3D stereophotogrammetry: a comparison to direct anthropometry and 2D photogrammetry. Angle Orthod. 2016; 86:487–494. PMID: 26267357.

4. Andrade LM, Rodrigues da Silva AM, Magri LV, Rodrigues da Silva MA. Repeatability study of angular and linear measurements on facial morphology analysis by means of stereophotogrammetry. J Craniofac Surg. 2017; 28:1107–1111. PMID: 28212123.

5. Su S, Sinha S, Gabriel V. Evaluating accuracy and reliability of active stereophotogrammetry using MAVIS III Wound Camera for three-dimensional assessment of hypertrophic scars. Burns. 2017; 43:1263–1270. PMID: 28363664.

6. Farkas LG, Bryson W, Klotz J. Is photogrammetry of the face reliable? Plast Reconstr Surg. 1980; 66:346–355. PMID: 7422721.

7. Aung SC, Ngim RC, Lee ST. Evaluation of the laser scanner as a surface measuring tool and its accuracy compared with direct facial anthropometric measurements. Br J Plast Surg. 1995; 48:551–558. PMID: 8548155.

8. Kusnoto B, Evans CA. Reliability of a 3D surface laser scanner for orthodontic applications. Am J Orthod Dentofacial Orthop. 2002; 122:342–348. PMID: 12411877.

9. Da Silveira AC, Martinez O, Da Silveira D, Daw JL Jr, Cohen M. Three-dimensional technology for documentation and record keeping for patients with facial clefts. Clin Plast Surg. 2004; 31:141–148. PMID: 15145659.

10. Ceinos R, Tardivo D, Bertrand MF, Lupi-Pegurier L. Inter- and intra-operator reliability of facial and dental measurements using 3D-stereophotogrammetry. J Esthet Restor Dent. 2016; 28:178–189. PMID: 26887926.

11. Baysal A, Sahan AO, Ozturk MA, Uysal T. Reproducibility and reliability of three-dimensional soft tissue landmark identification using three-dimensional stereophotogrammetry. Angle Orthod. 2016; 86:1004–1009. PMID: 27023408.

12. Lam WY, Hsung RT, Choi WW, Luk HW, Cheng LY, Pow EH. A clinical technique for virtual articulator mounting with natural head position by using calibrated stereophotogrammetry. J Prosthet Dent. 2018; 119:902–908. PMID: 28969919.

13. Hassan B, Giménez Gonzáles B, Tahmaseb A, Jacobs R, Bornstein MM. Three-dimensional facial scanning technology: applications and future trends. Forum Implantol. 2014; 10:77–86.
14. Fink M, Medelnik J, Strobel K, Hirschfelder U, Hofmann E. Metric precision via soft-tissue landmarks in three-dimensional structured-light scans of human faces. J Orofac Orthop. 2014; 75:133–143. PMID: 24577017.

15. Kusnoto B, Evans CA. Reliability of a 3D surface laser scanner for orthodontic applications. Am J Orthod Dentofacial Orthop. 2002; 122:342–348. PMID: 12411877.

16. Lincoln KP, Sun AY, Prihoda TJ, Sutton AJ. Comparative accuracy of facial models fabricated using traditional and 3D imaging techniques. J Prosthodont. 2016; 25:207–215. PMID: 26381058.

17. Ramieri GA, Spada MC, Nasi A, Tavolaccini A, Vezzetti E, Tornincasa S, et al. Reconstruction of facial morphology from laser scanned data. Part I: reliability of the technique. Dentomaxillofac Radiol. 2006; 35:158–164. PMID: 16618848.

18. Weinberg SM, Naidoo S, Govier DP, Martin RA, Kane AA, Marazita ML. Anthropometric precision and accuracy of digital three-dimensional photogrammetry: comparing the Genex and 3dMD imaging systems with one another and with direct anthropometry. J Craniofac Surg. 2006; 17:477–483. PMID: 16770184.
19. Naini FB, Akram S, Kepinska J, Garagiola U, McDonald F, Wertheim D. Validation of a new three-dimensional imaging system using comparative craniofacial anthropometry. Maxillofac Plast Reconstr Surg. 2017; 39:23. PMID: 28894726.

20. Borman H, Ozgür F. A simple instrument to define the Frankfurt horizontal plane for soft-tissue measurements of the face. Plast Reconstr Surg. 1998; 102:580–581. PMID: 9703107.

21. Canfiled [Internet]. VECTRA H1 user guide. Parsippany: Canfield;cited 2019 Apr 23. Available from: http://canfieldupgrade.com/assets/media/VECTRA-H1-User-Guide.pdf.
22. Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994; 6:284–290.

23. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID: 843571.

24. Zogheib T, Jacobs R, Bornstein MM, Agbaje JO, Anumendem D, Klazen Y, et al. Comparison of 3D scanning versus 2D photography for the identification of facial soft-tissue landmarks. Open Dent J. 2018; 12:61–71. PMID: 29492171.

25. Metzler P, Sun Y, Zemann W, Bartella A, Lehner M, Obwegeser JA, et al. Validity of the 3D VECTRA photogrammetric surface imaging system for cranio-maxillofacial anthropometric measurements. Oral Maxillofac Surg. 2014; 18:297–304. PMID: 23559195.

26. de Menezes M, Rosati R, Ferrario VF, Sforza C. Accuracy and reproducibility of a 3-dimensional stereophotogrammetric imaging system. J Oral Maxillofac Surg. 2010; 68:2129–2135. PMID: 20646812.

27. Storms AS, Vansant L, Shaheen E, Coucke W, de Llano-Pérula MC, Jacobs R, et al. Three-dimensional aesthetic assessment of class II patients before and after orthognathic surgery and its association with quantitative surgical changes. Int J Oral Maxillofac Surg. 2017; 46:1664–1671. PMID: 28751183.

28. Stebel A, Desmedt D, Bronkhorst E, Kuijpers MA, Fudalej PS. Rating nasolabial appearance on three-dimensional images in cleft lip and palate: a comparison with standard photographs. Eur J Orthod. 2016; 38:197–201. PMID: 25900054.

29. Hajeer MY, Ayoub AF, Millett DT, Bock M, Siebert JP. Three-dimensional imaging in orthognathic surgery: the clinical application of a new method. Int J Adult Orthodon Orthognath Surg. 2002; 17:318–330. PMID: 12593004.
30. Tzou CH, Artner NM, Pona I, Hold A, Placheta E, Kropatsch WG, et al. Comparison of three-dimensional surface-imaging systems. J Plast Reconstr Aesthet Surg. 2014; 67:489–497. PMID: 24529695.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download