Abstract
Purpose
The aim of this in vitro study was to determine the sensitivity and specificity of cone-beam computed tomography (CBCT) and digital periapical radiography in the detection of mesial root perforations of mandibular molars.
Materials and Methods
In this in vitro study, 48 mandibular molars were divided into 4 groups. First, the mesial canals of all the 48 teeth were endodontically prepared. In 2 groups (24 teeth each), the roots were axially perforated in the mesiolingual canal 1-3 mm below the furcation region, penetrating the root surface ("root perforation"). Then, in one of these 2 groups, the mesial canals were filled with gutta-percha and AH26 sealer. Mesial canals in one of the other 2 groups without perforation (control groups) were filled with the same materials. The CBCT and periapical radiographs with 3 different angulations were evaluated by 2 oral and maxillofacial radiologists. The specificity and sensitivity of the two methods were calculated, and P<0.05 was considered significant.
Results
The sensitivity and specificity of CBCT scans in the detection of obturated root canal perforations were 79% and 96%, respectively, and in the case of three-angled periapical radiographs, they were 92% and 100%, respectively. In non-obturated root canals, the sensitivity and specificity of CBCT scans in perforation detection were 92% and 100%, respectively, and for three-angled periapical radiographs, they were 50% and 96%, respectively.
Perforations are unfortunate complications that occur in the course of endodontic treatment even for the most skilled clinicians.1 According to previous studies, 2-12% of endodontically treated teeth have iatrogenic perforations.2 Most of these perforations occur in mandibular molars due to root curvatures and canal positions.3
A definite diagnosis of perforations in endodontically treated teeth is important, and timely detection of perforations will aid in selecting appropriate therapy, minimizing bone loss, and predicting prognosis.4
Periapical radiography has certain benefits for the diagnosis, treatment, and follow-up of patients. Multi-angled radiography plays an important role in detecting perforations.5 However, this technique cannot estimate the true size, location, and aspects of a lesion because of the compression of the 3-dimensional structure into a 2-dimensional image, overlapping anatomic structures, and the beam angle of the rays.6 Cone-beam computed tomography (CBCT) has been recently introduced as a valuable diagnostic tool in the following stages of endodontic treatment: characterizing the periapical lesion and its healing process,5 diagnosing dentoalveolar and vertical root fractures,7,8,9 characterizing root canal anomalies and root curvatures,8 assessing root resorption defects and differential diagnosis of the internal and external root resorption,8,10 and detecting broken endodontic instruments, calcified or additional roots, and canal perforations.8
According to Shemesh et al,5 CBCT showed a higher accuracy in detecting root perforations than digital periapical radiography. Also, Kamburoglu et al11 reported that CBCT was better at detecting vertical root fractures than intraoral digital radiography.
The aim of this study was to evaluate and compare CBCT with digital periapical radiography for detecting mesial root perforations in mandibular molars before and after canal obturation.
In this in vitro study, 48 human first and second mandibular molars were selected and stored in sodium chloride (0.9%) before laboratory procedures. All these teeth were sound and had 2 canals in their mesial root. Also, there was no significant difference in the mesial root curvature. The mesial root curvature was measured using Schneider's method.12 In brief, the first line was drawn parallel to the long axis of the canal, and then, the second line was drawn from the apical foramen to intersect with the first line at the point where the canal began to leave the long axis to the tooth. Then, the teeth were divided into 4 groups, each containing 12 teeth.
Digital periapical radiographs were taken with a fixed X-ray unit (Soredex, Helsinki, Finland) and #2-size image plate (Digora PCT, Soredex, Helsinki, Finland) using a parallel technique with the exposure parameters set as follows: at 60 kVp tube voltage, 7 mA tube current, and 0.2 s exposure time.
In all 4 groups, both mesial canals were prepared. In this study, a mesiolingual canal was selected for perforation due to its prominent curvature. The groups were as follows: Group A: strip perforation of the mesiolingual canal and obturation of both mesial canals; Group B: no strip perforation of the mesiolingual canal and obturation of both mesial canals; Group C: strip perforation of the mesiolingual canal and no obturation of the mesial canals; and Group D: no strip perforation of the mesiolingual canal and no obturation of the mesial canals.
The length of the mesial canal was measured using a No. 10 K-file. When the tip of this file was seen at the root apex, the length of the file was measured and the working length was considered to be 1 mm less than this measurement. The mesial canals were prepared with No. 15, No. 20, and No. 25K-files. The coronal 1/3 of the mesial canals was prepared by No. 2 and No. 3 Gates Glidden (Densely, Switzerland). Thereafter, the two mesial canals were prepared with System GT rotary instruments (NSK, Tokyo, Japan) at 300 rpm using a torque-control motor with S1, S2, F1, and F2 Protaper endodontic files (Dentsply, York, PA, USA) according to the manufacturer's instructions. The last file used was a No. 30 Mtwo (VDW, Munich, Germany) with a taper of 0.05.
Each canal was repeatedly irrigated with a freshly prepared 2% solution of sodium hypochlorite (NaOCl) using a syringe and a 27-gauge needle (12 mL for each canal). After completion of the procedure, the canals were rinsed with 12 mL of distilled water.
For root perforation, a No. 2 Gates Glidden (Dentsply, York, PA, USA), cutting in from the best diameter achieved using a diamond fissure bur, was rotated in an axial direction within the canal, penetrating through the root at 1-3 mm below the furcation in order for a No. 25 K-file to pass through the defect passively.
All root canals were dried using three size 30 paper points. AH 26 sealer (Dentsply, York, PA, USA) was mixed according to the manufacturer's instructions and introduced into the canal on two occasions, for 5 s each, by using a Lentulo spiral. Standard size 30 gutta-percha cones with a 0.02 taper were coated with the sealer and placed into the root canal. The roots were filled using the lateral condensation technique with a size B spreader and standard size 20 gutta-percha cones. The roots were coated with one layer of dental wax to simulate periodontal ligament and then mounted using the same amounts of plaster and sawdust.
Digital periapical radiographs were taken with a fixed X-ray unit (Soredex, Helsinki, Finland) and a size 2 phosphor plate (Digora PCT, Soredex, Helsinki, Finland) with a parallel technique and three horizontal angles including the direct angle, 10° mesially, and 10° distally. The imaging parameters were set at 60 kVp tube voltage, 7 mA tube current, and 0.2 s exposure time. The pixel size of the image was 85-167 µm, and the image resolution was 6-8 line pair (LP)/mm.
CBCT scans were then taken with a Cranex 3D System (Soredex, Helsinki, Finland) having a field of view (FOV) of 6 cm×8 cm; the imaging parameters were as follows: 89 kVp tube voltage, 6 mA tube current, and 130 µm voxel size high-resolution. The CBCT images, including the axial, coronal, sagittal, and multiplanar reconstruction images with a slice thickness of 0.1 mm and an interval of 0.1 mm, were reviewed in the three reconstruction planes. Two observers who were oral and maxillofacial radiologists were calibrated; they examined the images separately by using a monitor (LG Flatron 18.5-inch, Seoul, Korea) in a low-lit room. They graded their observations as 'perforation', 'no perforation', or 'questionable' (Fig. 1).
The overall agreement among the observers was calculated using Cohen's kappa. The data were analyzed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). The sensitivity, specificity, negative predictive value, positive predictive value, and likelihood ratio (LR+, LR-) with a confidence interval (CI 95%) of both CBCT scans and periapical radiographs for the detection of the perforations were calculated. The χ2 test was used to compare between CBCT scans and periapical radiographs. P<0.05 was considered significant.
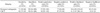
Tables 1 and 2 show the sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio of the CBCT scans and periapical radiographs for the detection of the root perforations.
CBCT revealed higher sensitivity than periapical radiographs, and both of them showed the same desirable specificity (98%) (Table 1). Seventeen of the 24 perforated teeth were detected using three-angled periapical radiography (6 teeth in the mesially angled position, 13 teeth in the direct-angle position, and 13 teeth in the distally angled position).
Both CBCT scans and periapical radiographs showed high specificity for detecting the root perforations of obturated root canals. Periapical radiographs revealed higher sensitivity even though the difference was not significant. In the teeth without obturation, although both the images showed high specificity, CBCT demonstrated higher sensitivity with a significant difference (P<0.05) (Table 2).
In the obturated root canals, three-angled periapical radiography detected 11 perforations out of 12 (5 teeth in the mesially angled position, 9 teeth in the direct-angle position, and 8 teeth in the distally angled position). In the non-obturated root canals, three-angled periapical radiography detected 6 perforations out of 12 (1 tooth in the mesially angled position, 4 teeth in the direct-angle position, and 5 teeth in the distally angled position).
Regarding the overall agreement among the observers, the k value was 0.831±0.081 in CBCT and 0.775±0.095 in the periapical radiographs, respectively.
The results of the current in vitro experiment showed that periapical radiographs were better able to detect root perforations in obturated root canals than CBCT scans. This could be attributed to the streak artifacts on CBCT due to radiopaque substances. In Hassan et al,7 the presence of a root canal filling reduced the specificity of CBCT scans in diagnosing vertical root fractures. In other studies,13,14 the beam hardening effect of canal filling substances with a high density led to incorrect reading of the CBCT scans. This could be attributed to the low-energy photons affecting the perforation detection.
In Shemesh et al,5 the CBCT scans showed a higher accuracy than periapical radiographs in detecting perforations. This difference between their report and our study could partly be explained by the differences in perforation size and location, and in CBCT devices. In their study, a No. 30 K-file was used to perforate the root apex; therefore, the size and shape of the perforation and the penetration of the filling substance into the perforation location would be different from those of our study. Also, a further study using various CBCT machines needs to be performed.
The results of periapical radiography in obturated root canals showed that one-angle radiography detected up to 75% of the perforations and three-angled radiography increased the detection to 92%. Among the angles, directangle radiography was the best.
In Shemesh et al5 and Regan et al,15 the detection of perforations and other lesions was easier when using radiography with different angles as compared to one-angle radiography. Also, the insertion of radiopaque substances such as calcium hydroxide and barium sulfide into canals improved the radiographic diagnosis.2 Therefore, the use of radiopaque filling substances and three different angles, and the presence of streak artifacts in CBCT scans may have led to the better diagnostic results of periapical radiography relative to CBCT in this study.
In the mesial canals with no obturation, periapical radiographs revealed significantly lower accuracy than CBCT scans in detecting perforations. Only 50% of the perforations could be detected on the periapical radiographs, and this might be attributed to the two-dimensional images and overlapping anatomic structures, as reported in several studies.6,16 Since CBCT scans provide three-dimensional and reconstruction images in the sagittal, axial, and coronal planes, they are more accurate than periapical radiographs in detecting the perforations in root canals with no root-filling material. In Bernardes et al,17 CBCT scans were also significantly better than three-angled periapical radiographs in detecting the defects caused by burs in teeth, as in our study. This study also indicated that the overall sensitivity of CBCT scans in detecting the perforations in non-obturated root canals was higher than that of periapical radiographs. In particular, considering the significantly lower accuracy of periapical radiographs than that of CBCT scans in detecting perforations of non-obturated canals (P<0.05), CBCT scans were regarded as more accurate imaging for detecting perforations.
This study revealed that CBCT scanning is a more sensitive technique than periapical radiography, considering the low negative likelihood ratio of CBCT even though the positive likelihood ratio was high for both these techniques. This result might be attributed to the lower sensitivity of periapical radiographs in detecting the perforations of the roots without obturation.
A major drawback of CBCT is its relatively high radiation dose as compared to that required by conventional radiography. By reducing the scanned volume, we can decrease this radiation dose.
Figures and Tables
Fig. 1
Periapical radiographs and cone-beam CT scans show the groups of perforated root canals with obturation and no obturation, and the control group.

Acknowledgments
We are grateful to Dr. Mohammad Mehdizadeh and the staff of Oral and Maxillofacial Radiology Department for their invaluable contribution to this study, and to Dr. Evangeline Foronda for the English editing of this manuscript.
References
1. Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011; 44:583–609.

2. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics. 2006; 13:95–107.

3. Tsesis I, Rosenberg E, Faivishevsky V, Kfir A, Katz M, Rosen E. Prevalence and associated periodontal status of teeth with root perforation: a retrospective study of 2,002 patients' medical records. J Endod. 2010; 36:797–800.

4. Alhadainy HA. Root perforations. A review of literature. Oral Surg Oral Med Oral Pathol. 1994; 78:368–374.
5. Shemesh H, Cristescu RC, Wesselink PR, Wu MK. The use of cone-beam computed tomography and digital periapical radiographs to diagnose root perforations. J Endod. 2011; 37:513–516.

6. Kamburoglu K, Kursun S, Yuksel S, Oztas B. Observer ability to detect ex vivo simulated internal or external cervical root resorption. J Endod. 2011; 37:168–175.
7. Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J Endod. 2009; 35:719–722.

8. Scarfe WC, Levin MD, Gane D, Farman AG. Use of cone beam computed tomography in endodontics. Int J Dent. 2009; 2009:634567.

9. Kajan ZD, Taromsari M. Value of cone beam CT in detection of dental root fractures. Dentomaxillofac Radiol. 2012; 41:3–10.

10. Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - an in vivo investigation. Int Endod J. 2009; 42:831–838.
11. Kamburoğlu K, Murat S, Yüksel SP, Cebeci AR, Horasan S. Detection of vertical root fracture using cone-beam computerized tomography: an in vitro assessment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e74–e81.

12. Schneider SW. A comparison of canal preparations in straight and curved root canals. Oral Surg Oral Med Oral Pathol. 1971; 32:271–275.

13. Bechara B, Alex McMahan C, Moore WS, Noujeim M, Teixeira FB, Geha H. Cone beam CT scans with and without artefact reduction in root fracture detection of endodontically treated teeth. Dentomaxillofac Radiol. 2013; 42:20120245.

14. Bueno MR, Estrela C, De Figueiredo JA, Azevedo BC. Mapreading strategy to diagnose root perforations near metallic intracanal posts by using cone-beam computed tomography. J Endod. 2011; 37:85–90.
15. Regan JD, Witherspoon DE, Foyle D. Surgical repair of root and tooth perforations. Endod Topics. 2005; 11:152–178.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download