Abstract
Non-Hodgkin's lymphomas are a group of highly diverse malignancies and have a strong tendency to affect organs and tissues that do not ordinarily contain lymphoid cells. Primary extra nodal lymphoma of the hard palate is rare. Here, we present a case of diffuse large B cell lymphoma in a 60-year-old male patient that manifested as slightly painful ulcerated growth on the edentulous right maxillary alveolar ridge extending onto the palate, closely resembling carcinoma of the alveolar ridge. Computed tomography images showed the involvement of the maxillary sinus and right nasal cavity, along with destruction of hard palate, superiorly extending into the orbit. This case report highlights the importance of imaging to evaluate the exact extent of such large malignant lesions, which is essential for treatment planning.
Malignant lymphoma is the generic term given to tumors of the lymphoid system. This lesion can involve the lymph nodes, spleen, and sometimes the non-hematopoietic tissues. This tumor can be divided into two major categories: Hodgkin's lymphoma and non-Hodgkin's lymphoma (NHL). NHL is a heterogeneous group of malignancies characterized by an abnormal clonal proliferation of T cells, B cells, or both. The majority of the adult NHLs are of B cell origin.1 Palatal and nasal lymphomas are rare, and the majority of the lymphomas in this region originate from B cells. Since early detection of hard palate tumors is difficult by clinical examination, the vast majority of such tumors are detected after maxillary or sphenoid bone invasion.2 The present report showed a case of B cell lymphoma in a 60-year-old male patient manifested as an ulcerative growth on the right maxillary alveolar ridge extending on to the hard palate, but on imaging it was an extensive lesion involving maxillary sinus, nasal cavity, and orbit.
A 60-year-old man visited the Oral Medicine and Radiology Department, complaining of a mild intermittent pain associated with sudden ulcerated growth on the right maxillary edentulous alveolar ridge since 1 month earlier. The patient gave a history of extraction of teeth in the same region one year before. On examination, a diffuse mild extra oral swelling was present on the right cheek, with proptosis and watery discharge from the right eye (Fig. 1). On palpation, extraorally the swelling was mildly tender and discontinuity was felt on the right infra orbital margin. Intraoral examination revealed a soft well defined ulcerated growth on the right maxillary edentulous alveolar ridge, extending from the right maxillary first molar region to the maxillary tuberosity region posteriorly. The surface of the growth was covered with a yellowish necrotic material. It was slightly tender on palpation (Fig. 2).
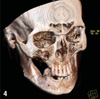
The clinical differential diagnosis included the most common malignancies in the oral cavity such as squamous cell carcinoma (SCC), minor salivary gland tumor, and carcinoma of the maxillary sinus. Panoramic radiograph revealed severe bone destruction of the right maxilla distal to the canine. The floor of the right maxillary sinus was also destroyed. Computed tomography (CT) scan was performed and sections were taken in the axial, coronal, and sagittal planes. Coronal section revealed a large soft tissue density lesion with its epicentre in the maxillary sinus, causing destruction of all walls of the maxillary sinus, extending medially into the lateral wall of the nasal septum, left nasal cavity involving the inferior and middle turbinates, laterally into the pterygopalatine fossa, superiorly into the orbit, inferiorly causing destruction of the hard palate and alveolar processes of the right maxilla in the molar region. There was no evidence of calcification (Fig. 3). Three dimensional CT reconstructions using the bone and soft tissue settings demonstrated a large lytic lesion in the right maxillary sinus destroying all walls of the maxillary sinus, hard palate, and alveolar process in the molar region (Figs. 4 and 5).
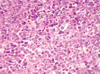
The patient was advised to undergo routine haematological examination, and an incisional biopsy was performed which revealed a cellular connective tissue stroma predominantly made up of lymphocytes, the majority being large cells and a few small cells showing vesicular nuclei with prominent nucleoli. Scattering foamy macrophages were seen amongst these cells. It was finally diagnosed as diffuse large cell lymphoma (Fig. 6). The patient was referred to the oncology department, who started chemotherapy; unfortunately, the patient passed away after two cycles of chemotherapy.
Malignant lymphoma can appear in all parts of the body, and may have varied radiographic manifestations.3 24-84% of NHLs arise from extra nodal sites. The head and neck is the second most common region for extra nodal lymphoma after the gastro intestinal tract.4 NHL is the second most common neoplasm of the head and neck region after SCC and the third most common group of malignant lesions of the oral region after SCC and salivary gland neoplasm.5,6
NHL commonly involves oropharyngeal lymphoid tissue comprising Waldeyer's ring, but occasionally involves other oral tissues.6 NHL occurs more frequently in the head and neck region in the pediatric age group,7 however our patient was a 60-year-old male. Sinuses are the primary site of NHL in 90% of the cases, most commonly invaded by diffuse large B cell lymphoma.7 In our case, the epicentre of the lesion seemed to be in the right maxillary sinus on the CT images.
The etiological factors for primary lymphoma of the oral region are unclear. A few cases of oral lymphomas were reported in association with acquired immune deficiency syndrome (AIDS), and it might even be the first presentation of AIDS in certain individuals.8 In our case, the patient was human immunodeficiency virus (HIV) negative. Primary oral and para-oral lymphoma most commonly presents as a painless local mass that gradually increases in size with superficial ulceration.9 Diagnosis of NHL in oral cavity may result from mucosal tissue/gingival swelling/masses. When oral soft tissue lesions first appear, they are relatively soft and often have an overlying ulceration, and are often characterized by absence of other symptoms. If bone is the primary site, tooth mobility and alveolar bone loss are often noted. Pain, swelling, numbness of the lip, and pathologically related fractures may be associated with the bone lesion.5 In our case, the patient presented with a slightly painful ulcerated growth on the maxillary edentulous alveolar ridge resembling SCC.
Clinical signs and symptoms of lymphomas of the paranasal sinuses include a mass in the nasal cavity, facial pain, paresthesia, recurrent sinusitis, nasal discharge, eyelid swelling, and proptosis if orbital invasion has occurred.10 Our patient showed an extraoral swelling in the right maxillary sinus region and also proptosis of the eye suggestive of extension of the lesion into the sinus and orbit.
Radiological imaging is vital for many reasons, including assessment of tumor extension, assessment of bony destruction, evidence of mucosal thickening, and choice of biopsy site and route. CT is the best imaging modality for demonstrating fine bony detail.10 Lymphoma can cause nonspecific bony destruction at and around the paranasal sinuses. The maxillary sinuses are most frequently affected, followed by the ethmoidal and frontal sinuses. The sphenoid sinuses are rarely affected. As the process of destruction continues, the bony margins of the maxillary sinuses can become eroded, especially the medial and posterior walls. Erosion of the anterior wall of the maxillary sinus was also reported.11 The epicentre was found to be in the right maxillary sinus on CT images in our case also. All walls of the maxillary sinus were eroded by the soft tissue lesion.
Lymphomas are usually submucosal, and on gross appearance, differ from SCC which is usually ulcerative.12 Our case clinically manifested as an ulcerated growth closely resembling SCC, and it was very difficult to differentiate both of the lesions clinically. Biopsy should be performed to ensure the accurate diagnosis and histological grading of lymphoma. Management also varies depending on the stage of lymphoma. Paranasal lymphomas have a poor prognosis, which is usually worse than that associated with lymphomas in other sites in the body.10
In conclusion, this report focused on the importance of CT in assessing the exact tumor extent and staging for large, clinically doubtful lesions, which was essential for diagnosis and treatment planning.
Figures and Tables
Fig. 2
Intraoral photograph shows an ulcerative growth in the right maxillary alveolar ridge extending on to the palate.

Fig. 3
Coronal CT image shows a large soft tissue density lesion with destruction of all walls of the right maxillary sinus, hard palate, and extension into the nasal cavity.
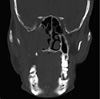
Fig. 4
Three-dimensional CT reconstruction image (bone setting) shows destruction of the maxilla, hard palate, and maxillary alveolar ridge on the right side.
References
1. Jayakrishnan R, Thomas G, Kumar A, Nair R. Non-Hodgkin's lymphoma of the hard palate. J Oral Maxillofac Pathol. 2008. 12:85–87.

2. Dalirsani Z, Mohtasham N. T-cell lymphoma of palate with nose and maxillary sinus involvement: a case report. Iran J Med Sci. 2010. 35:254–258.
3. Ueda F, Suzuki M, Matsui O, Minato H, Furukawa M. MR findings of nine cases of palatal tumor. Magn Reson Med Sci. 2005. 4:61–67.

4. Teh CS, Chong SY. An unusual presentation of lymphoma of the head and neck region. Med J Malaysia. 2011. 66:264–265.
5. Villa A, Mariani U, Villa F. T-cell lymphoma of the oral cavity: a case report. Aust Dent J. 2010. 55:203–206.

6. Vaswani B, Shah M, Shah PM, Parikh BJ, Anand AS, Sharma G. Non hodgkin's lymphoma of tongue - a case report. Indian J Med Paediatr Oncol. 2008. 29:59–61.

7. Zagolski O, Dwivedi RC, Subramanian S, Kazi R. Non-Hodgkin's lymphoma of the sino-nasal tract in children. J Cancer Res Ther. 2010. 6:5–10.
8. Maheshwari GK, Baboo HA, Shah NM, Patel MH, Shah R. Primary non-Hodgkin's lymphoma of the oral tongue. Turk J Cancer. 2001. 31:121–124.
9. Essadi I, Ismaili N, Tazi E, Elmajjaoui S, Saidi A, Ichou M, et al. Primary lymphoma of the head and neck: two case reports and review of the literature. Cases J. 2008. 1:426.

10. Park YM, Cho JH, Cho JY, Huh JS, Ahn JY. Non-Hodgkin's lymphoma of the sphenoid sinus presenting as isolated oculomotor nerve palsy. World J Surg Oncol. 2007. 5:86.

11. Al-Hakeem DA, Fedele S, Carlos R, Porter S. Extra nodal NK/T-cell lymphoma, nasal type. Oral Oncol. 2007. 43:4–14.
12. Chalastras T, Elefteriadou A, Giotakis J, Soulandikas K, Korres S, Ferekidis E, et al. Non-Hodgkin's lymphoma of nasal cavity and paranasal sinuses. A clinicopathological and immunhistochemical study. Acta Otorhinolaryngol Ital. 2007. 27:6–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download