1. Kalashnikova LA, Zueva YV, Pugacheva OV, Korsakova NK. Cognitive impairments in cerebellar infarcts. Neurosci Behav Physiol. 2005; 35:773–779. PMID:
16132255.

2. Glickstein M, Strata P, Voogd J. Cerebellum: history. Neuroscience. 2009; 162:549–559. PMID:
19272426.

3. Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998; 121(Pt 4):561–579. PMID:
9577385.

4. O'Halloran CJ, Kinsella GJ, Storey E. The cerebellum and neuropsychological functioning: a critical review. J Clin Exp Neuropsychol. 2012; 34:35–56. PMID:
22047489.
5. Gottwald B, Wilde B, Mihajlovic Z, Mehdorn HM. Evidence for distinct cognitive deficits after focal cerebellar lesions. J Neurol Neurosurg Psychiatry. 2004; 75:1524–1531. PMID:
15489381.

6. Hokkanen LS, Kauranen V, Roine RO, Salonen O, Kotila M. Subtle cognitive deficits after cerebellar infarcts. Eur J Neurol. 2006; 13:161–170. PMID:
16490047.

7. Townsend J, Courchesne E, Covington J, Westerfield M, Harris NS, Lyden P, et al. Spatial attention deficits in patients with acquired or developmental cerebellar abnormality. J Neurosci. 1999; 19:5632–5643. PMID:
10377369.

8. Neau JP, Arroyo-Anllo E, Bonnaud V, Ingrand P, Gil R. Neuropsychological disturbances in cerebellar infarcts. Acta Neurol Scand. 2000; 102:363–370. PMID:
11125751.

9. Lezak MD. Neuropsychological assessment. 4th ed. New York: Oxford University Press;2004. p. 343–761.
10. Kang Y, Jang S, Na DL. Seoul Neuropsychological Screening Battery (SNSB-II). 2nd ed. Seoul: Human Brain Research & Consulting Co.;2012. p. 11–83.
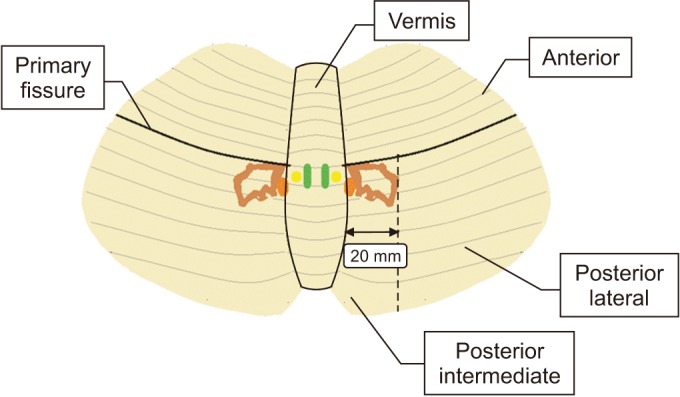
11. Voogd J, Glickstein M. The anatomy of the cerebellum. Trends Neurosci. 1998; 21:370–375. PMID:
9735944.

12. Schmahmann JD. From movement to thought: anatomic substrates of the cerebellar contribution to cognitive processing. Hum Brain Mapp. 1996; 4:174–198. PMID:
20408197.

13. Diedrichsen J, Maderwald S, Kuper M, Thurling M, Rabe K, Gizewski ER, et al. Imaging the deep cerebellar nuclei: a probabilistic atlas and normalization procedure. Neuroimage. 2011; 54:1786–1794. PMID:
20965257.

14. Dimitrova A, Weber J, Redies C, Kindsvater K, Maschke M, Kolb FP, et al. MRI atlas of the human cerebellar nuclei. Neuroimage. 2002; 17:240–255. PMID:
12482081.

15. Dimitrova A, Zeljko D, Schwarze F, Maschke M, Gerwig M, Frings M, et al. Probabilistic 3D MRI atlas of the human cerebellar dentate/interposed nuclei. Neuroimage. 2006; 30:12–25. PMID:
16257240.

16. Schweizer TA, Alexander MP, Cusimano M, Stuss DT. Fast and efficient visuotemporal attention requires the cerebellum. Neuropsychologia. 2007; 45:3068–3074. PMID:
17640689.

17. Gottwald B, Mihajlovic Z, Wilde B, Mehdorn HM. Does the cerebellum contribute to specific aspects of attention? Neuropsychologia. 2003; 41:1452–1460. PMID:
12849763.

18. Leggio MG, Tedesco AM, Chiricozzi FR, Clausi S, Orsini A, Molinari M. Cognitive sequencing impairment in patients with focal or atrophic cerebellar damage. Brain. 2008; 131(Pt 5):1332–1343. PMID:
18334535.

19. Middleton FA, Strick PL. Anatomical evidence for cerebellar and basal ganglia involvement in higher cognitive function. Science. 1994; 266:458–461. PMID:
7939688.

20. Leiner HC, Leiner AL, Dow RS. Reappraising the cerebellum: what does the hindbrain contribute to the forebrain? Behav Neurosci. 1989; 103:998–1008. PMID:
2679667.

21. Arnsten AF, Rubia K. Neurobiological circuits regulating attention, cognitive control, motivation, and emotion: disruptions in neurodevelopmental psychiatric disorders. J Am Acad Child Adolesc Psychiatry. 2012; 51:356–367. PMID:
22449642.

22. Middleton FA, Strick PL. Basal ganglia and cerebellar loops: motor and cognitive circuits. Brain Res Brain Res Rev. 2000; 31:236–250. PMID:
10719151.

23. Petersen SE, Fiez JA. The processing of single words studied with positron emission tomography. Annu Rev Neurosci. 1993; 16:509–530. PMID:
8460901.

24. Kim SG, Ugurbil K, Strick PL. Activation of a cerebellar output nucleus during cognitive processing. Science. 1994; 265:949–951. PMID:
8052851.

25. Klingberg T, Roland P, Kawashima R. The neural correlates of the central executive function during working memory: a PET study. Hum Brain Mapp. 1995; 1(Suppl 1):414.
26. Leblanc R, Meyer E, Bub D, Zatorre RJ, Evans AC. Language localization with activation positron emission tomography scanning. Neurosurgery. 1992; 31:369–373. PMID:
1513446.

27. Leiner HC, Leiner AL, Dow RS. Does the cerebellum contribute to mental skills? Behav Neurosci. 1986; 100:443–454. PMID:
3741598.

28. Allen G, McColl R, Barnard H, Ringe WK, Fleckenstein J, Cullum CM. Magnetic resonance imaging of cerebellar-prefrontal and cerebellar-parietal functional connectivity. Neuroimage. 2005; 28:39–48. PMID:
16023375.

29. Desmond JE, Gabrieli JD, Wagner AD, Ginier BL, Glover GH. Lobular patterns of cerebellar activation in verbal working-memory and finger-tapping tasks as revealed by functional MRI. J Neurosci. 1997; 17:9675–9685. PMID:
9391022.

30. Chen SH, Desmond JE. Temporal dynamics of cerebro-cerebellar network recruitment during a cognitive task. Neuropsychologia. 2005; 43:1227–1237. PMID:
15949507.

31. Molinari M, Leggio MG, Silveri MC. Verbal fluency and agrammatism. Int Rev Neurobiol. 1997; 41:325–339. PMID:
9378596.

32. Linde L, Bergstrom M. The effect of one night without sleep on problem-solving and immediate recall. Psychol Res. 1992; 54:127–136. PMID:
1620796.

33. Schmahmann JD, Macmore J, Vangel M. Cerebellar stroke without motor deficit: clinical evidence for motor and non-motor domains within the human cerebellum. Neuroscience. 2009; 162:852–861. PMID:
19531371.

34. Tatu L, Moulin T, Bogousslavsky J, Duvernoy H. Arterial territories of human brain: brainstem and cerebellum. Neurology. 1996; 47:1125–1135. PMID:
8909417.
35. Elizabeth O, Molliver ME. Organizational principles and microcircuitry of the cerebellum. Int Rev Psychiatry. 2001; 13:232–246.

36. Rudrauf D, Mehta S, Bruss J, Tranel D, Damasio H, Grabowski TJ. Thresholding lesion overlap difference maps: application to category-related naming and recognition deficits. Neuroimage. 2008; 41:970–984. PMID:
18442925.

37. Rorden C, Karnath HO. Using human brain lesions to infer function: a relic from a past era in the fMRI age? Nat Rev Neurosci. 2004; 5:813–819. PMID:
15378041.

38. D'Angelo E, De Zeeuw CI. Timing and plasticity in the cerebellum: focus on the granular layer. Trends Neurosci. 2009; 32:30–40. PMID:
18977038.
39. Malm J, Kristensen B, Karlsson T, Carlberg B, Fagerlund M, Olsson T. Cognitive impairment in young adults with infratentorial infarcts. Neurology. 1998; 51:433–440. PMID:
9710015.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download