This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To increase the rate of successful external cephalic version (ECV) and to minimize the complications, it is important to identify the predictors of success. Therefore, the purpose of this study was to investigate whether the height of the elevated fetal buttock (HOB) is a valuable predictor of successful ECV or not.
Methods
This prospective study was conducted from August 2016 to June 2018. A total of 139 pregnant women with breech presentation were enrolled in the study. HOB from the maternal pubic symphysis was measured on ultrasonography. The predictability and cut-off value of HOB for successful ECV were evaluated.
Results
Among the 139 patients, 114 (82%) had successful ECV. The adjusted odds ratio for multiparity, amniotic fluid index (AFI) >14 cm, and HOB >7.8 cm were 10.80 (95% confidence interval [CI], 1.57–74.94), 5.26 (95% CI, 1.06–26.19), and 10.50 (95% CI, 1.03–107.12), respectively. Areas under the curve (AUCs) for AFI, HOB, and parity were 0.66 (95% CI, 0.54–0.78), 0.74 (95% CI, 0.64–0.85), and 0.69 (95% CI, 0.62–0.76), respectively. HOB had the largest AUC, but there were no significant differences among the AUCs of other factors. The cut-off value of HOB was 6 cm.
Conclusion
This study showed that the AUC of HOB was greater than that of parity and AFI, although it was not statistically significant. As HOB is a noninvasive and comprehensive marker to predict successful ECV, consideration of HOB would be helpful before conducting ECV. Further studies are needed.
Keywords: Breech presentation, External cephalic version, Predictive value
Introduction
Breech presentation occurs in approximately 3–4% of women with singleton pregnancies [
1]. As breech presentation is risky for maintenance of pregnancy and delivery, practitioners perform several measures to prevent the adverse effects.
External cephalic version (ECV) is a procedure performed to change the fetal presentation from breech to cephalic by exerting pressure through the maternal abdominal wall [
2]. ECV reduces the rate of cesarean section in breech presentation in the late gestational period and the risk of fetal morbidity and mortality [
3].
In 2012, the rate of cesarean delivery was 32.8% in the United States of America and 36.0% in Korea [
2]. In 2018, the American College of Obstetricians and Gynecologists published recommendations reaffirming the existing guidelines that obstetricians should offer and perform ECV if possible [
45]. The success rate of ECV varies from 30% to 80% [
24]. However, ECV is associated with various complications, such as placental abruption, fetal-maternal hemorrhage, fracture of the fetal femur, prolonged fetal tachycardia, and sinusoidal pattern of the fetal heart rate [
5].
Factors associated with successful ECV should be detected to increase the success and uptake rate of ECV and to minimize complications. The known factors associated with successful ECV are maternal height, weight, body mass index (BMI), parity, placental location, estimated birth weight (EBW), and amniotic fluid index (AFI). Among these, the predictors of successful ECV are parity and AFI [
46]. Additionally, some clinical factors are associated with successful ECV, such as the surgeon's experience and dexterity with the procedure [
7].
However, prediction of the success of ECV is limited using the primary factors, such as maternal BMI, EBW, breech type, AFI, and parity. Secondary markers can comprehensively reflect the basic and primary factors and are useful for the objective prediction of successful ECV. Additionally, a condition for successful ECV is free-floating elevation of the fetal buttocks from the maternal pelvis by the surgeon. Therefore, we determined the height of the elevated fetal buttock (HOB) by measuring the distance between the pubic symphysis, confirmed on ultrasonography, and the fetal buttock elevated manually by the surgeon (
Fig. 1). If HOB were the most reliable factor for successful ECV, complications, such as fetal bradycardia and PROM, because of failed ECV would be reduced by applying HOB before ECV is performed. Therefore, the purpose of this study was to evaluate HOB as a marker of successful ECV.
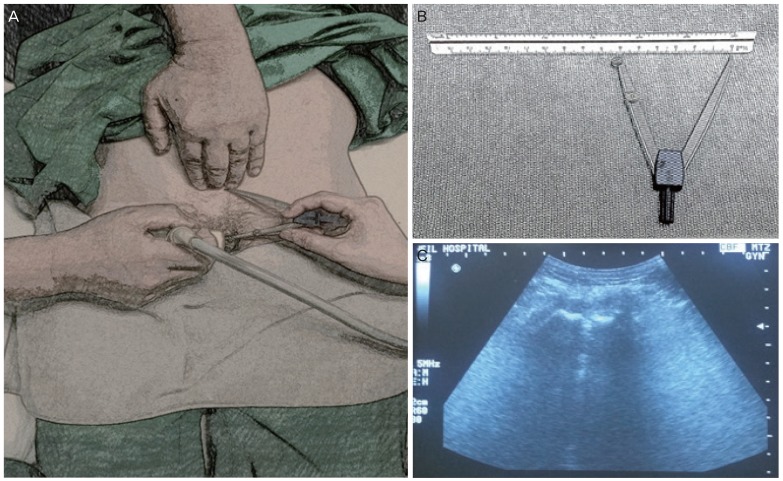
Fig. 1
Measurement of height of the elevated fetal buttock (HOB). (A) HOB by an operator's hand was measured from the maternal symphysis pubis under ultrasonography. (B) A compass and a ruler for measurement. (C) Symphysis pubis seen on ultrasonography.
Materials and methods
The study was prospectively designed and conducted from August 2016 to June 2018.
A total of 139 pregnant women with breech presentation were enrolled in the study. No participant presented with contraindications for ECV, such as preeclampsia, multiple pregnancy, antepartum hemorrhage, oligohydramnios, uteroplacental insufficiency, intrauterine growth retardation, or non-reassuring fetal monitoring pattern. Most ECVs were performed with ritodrine tocolysis, under epidural analgesia, following at least 30 minutes of fetal monitoring to ensure a normal fetal heart rate and uterine contractions in the delivery unit at the Cheil General Hospital & Women's Healthcare Center. However, some pregnant women did not consent to ritodrine tocolysis or epidural analgesia.
The ECV team comprised of 4 members, including a main supervisor (clinical surgeon), a sonographer (resident), and 2 helpers, including one nurse. Before initiating ECV, HOB was measured by the surgeon and a helper using a compass and a ruler. The surgeon pushed the fetal buttock upward toward the uterine fundus manually, and the resident measured HOB from the maternal pubic symphysis (
Fig. 1). Further, EBW, type of breech presentation, location of the placenta, presence of myoma, and AFI were checked on ultrasonography. The surgeon stood on the other side of the sonographer. In the process, if the fetus was descending or engaged too much in the pelvic cavity, a team member pushed the fetal buttock upward from the pelvic cavity for free floating of the fetus. If necessary, the other member stood on the opposite side of the surgeon and pushed the fetal head toward the direction of easy flow. The sonographer ran a probe along the shifting fetal head and checked the fetal heartbeat during each ECV trial. We tried to avoid exceeding 10 minutes for a single trial, and the maximum number of consecutive trials was limited to 3. ECV was discontinued immediately if the fetal heart rate showed a non-reassuring pattern or if the patient complained of an intolerable discomfort despite the use of epidural analgesia. Following ECV, we considered the procedure successful when the presentation showed a fetal head without umbilical cord compression or any odd positioning of extremities, such as the hands or feet placed under the fetal head. After a successful procedure, the patient was placed in the lateral decubitus position, and fetal monitoring was continued additionally for 3 hours. Ritodrine and analgesia were stopped. After confirmation of a reassuring fetal heartbeat and lack of regular contractions, the patient was discharged.
Univariate analyses were performed using the χ2 test or Fisher's exact test for categorical data and the student's t-test for continuous data. Multivariate analyses were performed using the logistic regression. Area under the curve (AUC) was calculated using the receiver operating characteristics (ROC) curve, and the cut-off value was obtained. The cut-off value was considered as the maximum value in the Youden's index (sensitivity+specificity-1). A P-value <0.05 was considered statistically significant.
Results
Among the 139 patients who underwent ECV after HOB measurement, 114 (82%) had successful ECV, while 25 (18%) had failed ECV. There were no fetal complications, such as abnormal fetal heart rate or rupture of the amniotic membrane, during the measurement, and the patients did not complain of any discomfort.
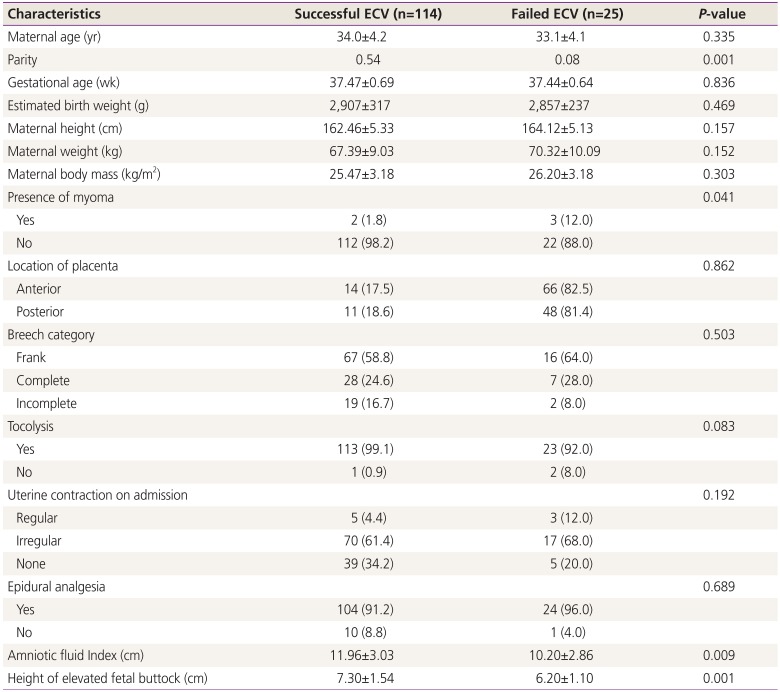
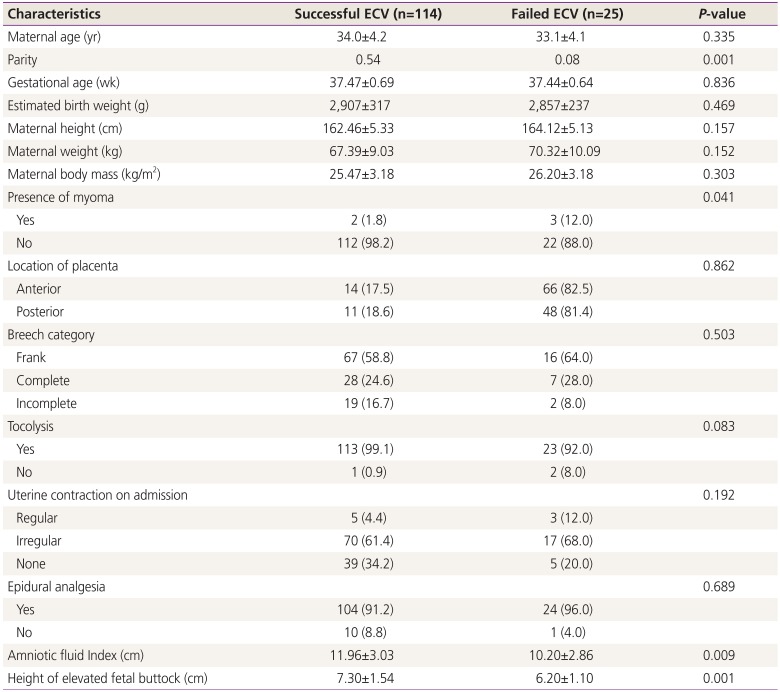
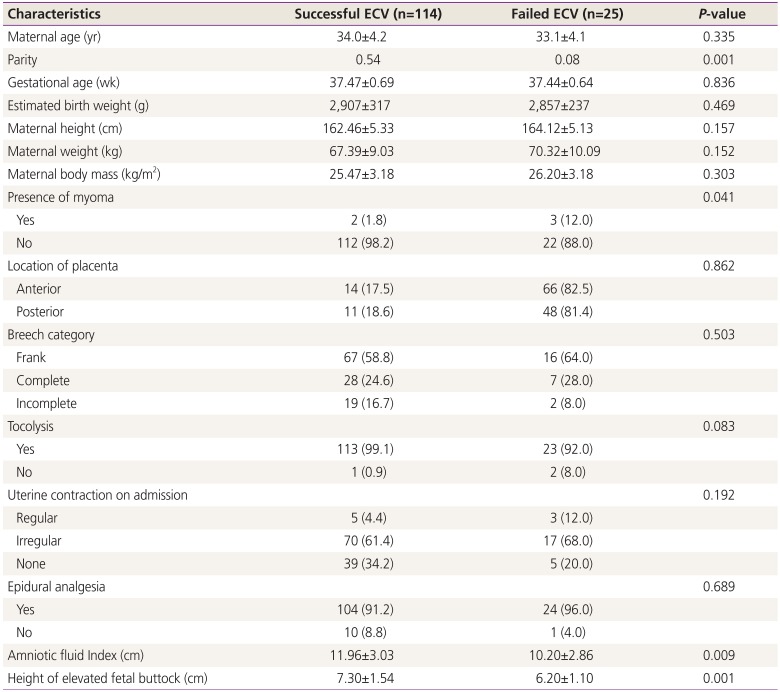
The demographic predictors of successful ECV, such as maternal age, gestational age, EBW, BMI, location of the placenta, breech category, tocolysis, uterine contraction on admission, and epidural analgesia, were not significantly different between the successful and failed group. The statistically significant variables associated with successful ECV were parity (
P=0.001), presence of myoma (
P=0.041), AFI (
P=0.009), and HOB (
P=0.001) (
Table 1).
Table 1
Demographics and prediction factors for successful external cephalic version (ECV)
|
Characteristics |
Successful ECV (n=114) |
Failed ECV (n=25) |
P-value |
|
Maternal age (yr) |
34.0±4.2 |
33.1±4.1 |
0.335 |
|
Parity |
0.54 |
0.08 |
0.001 |
|
Gestational age (wk) |
37.47±0.69 |
37.44±0.64 |
0.836 |
|
Estimated birth weight (g) |
2,907±317 |
2,857±237 |
0.469 |
|
Maternal height (cm) |
162.46±5.33 |
164.12±5.13 |
0.157 |
|
Maternal weight (kg) |
67.39±9.03 |
70.32±10.09 |
0.152 |
|
Maternal body mass (kg/m2) |
25.47±3.18 |
26.20±3.18 |
0.303 |
|
Presence of myoma |
|
|
0.041 |
|
Yes |
2 (1.8) |
3 (12.0) |
|
|
No |
112 (98.2) |
22 (88.0) |
|
|
Location of placenta |
|
|
0.862 |
|
Anterior |
14 (17.5) |
66 (82.5) |
|
|
Posterior |
11 (18.6) |
48 (81.4) |
|
|
Breech category |
|
|
0.503 |
|
Frank |
67 (58.8) |
16 (64.0) |
|
|
Complete |
28 (24.6) |
7 (28.0) |
|
|
Incomplete |
19 (16.7) |
2 (8.0) |
|
|
Tocolysis |
|
|
0.083 |
|
Yes |
113 (99.1) |
23 (92.0) |
|
|
No |
1 (0.9) |
2 (8.0) |
|
|
Uterine contraction on admission |
|
|
0.192 |
|
Regular |
5 (4.4) |
3 (12.0) |
|
|
Irregular |
70 (61.4) |
17 (68.0) |
|
|
None |
39 (34.2) |
5 (20.0) |
|
|
Epidural analgesia |
|
|
0.689 |
|
Yes |
104 (91.2) |
24 (96.0) |
|
|
No |
10 (8.8) |
1 (4.0) |
|
|
Amniotic fluid Index (cm) |
11.96±3.03 |
10.20±2.86 |
0.009 |
|
Height of elevated fetal buttock (cm) |
7.30±1.54 |
6.20±1.10 |
0.001 |
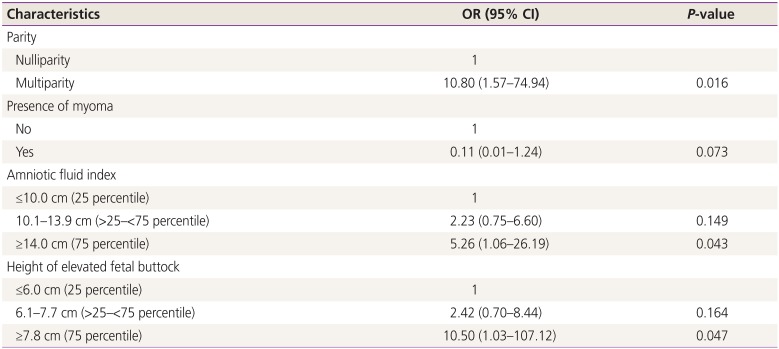
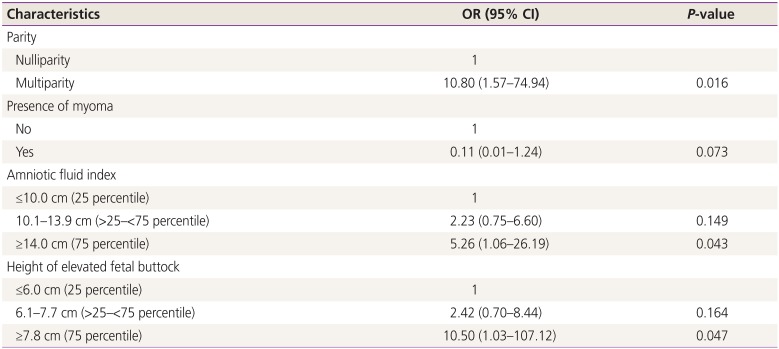
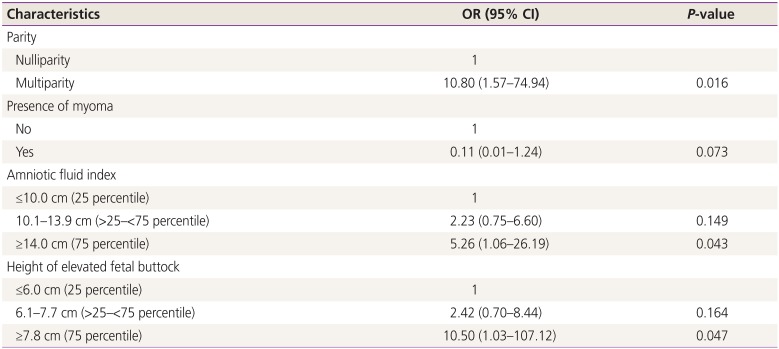
In the multivariate logistic regression analysis, the odds ratio (OR) for multiparity was 10.80 (95% confidence interval [CI], 1.57–74.94) times that of nulliparity; OR for AFI >14 cm was 5.26 (95% CI, 1.06–26.19) times that of AFI <10 cm; and OR for HOB >7.8 cm was 10.50 (95% CI, 1.03–107.12) times that of HOB ≤6 cm and was statistically significant. However, OR for the presence of myoma was not statistically significant (
P=0.073) (
Table 2).
Table 2
Logistic regression analysis for prediction factors of successful external cephalic version
|
Characteristics |
OR (95% CI) |
P-value |
|
Parity |
|
|
|
Nulliparity |
1 |
|
|
Multiparity |
10.80 (1.57–74.94) |
0.016 |
|
Presence of myoma |
|
|
|
No |
1 |
|
|
Yes |
0.11 (0.01–1.24) |
0.073 |
|
Amniotic fluid index |
|
|
|
≤10.0 cm (25 percentile) |
1 |
|
|
10.1–13.9 cm (>25–<75 percentile) |
2.23 (0.75–6.60) |
0.149 |
|
≥14.0 cm (75 percentile) |
5.26 (1.06–26.19) |
0.043 |
|
Height of elevated fetal buttock |
|
|
|
≤6.0 cm (25 percentile) |
1 |
|
|
6.1–7.7 cm (>25–<75 percentile) |
2.42 (0.70–8.44) |
0.164 |
|
≥7.8 cm (75 percentile) |
10.50 (1.03–107.12) |
0.047 |
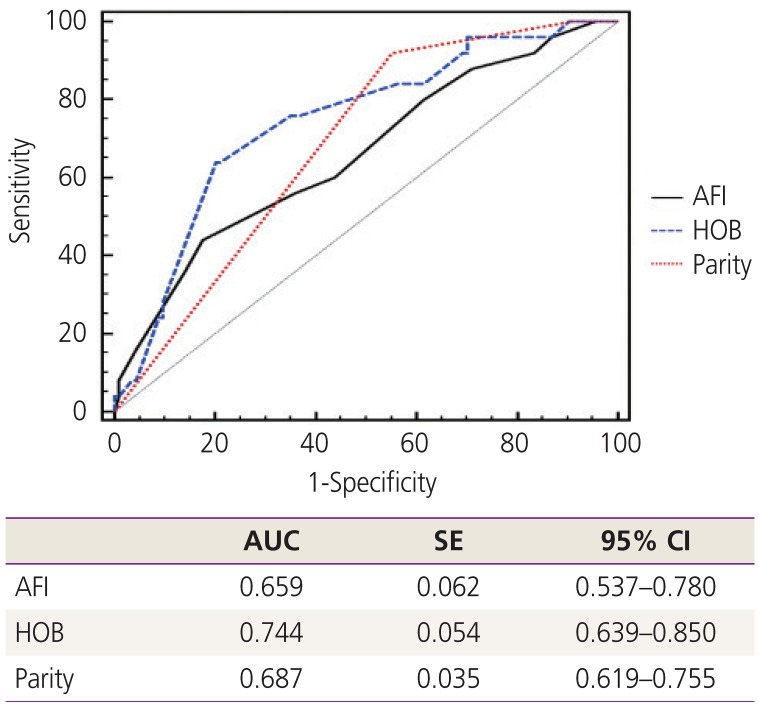
AUCs for AFI, HOB, and parity were 0.659 (95% CI, 0.537–0.780), 0.744 (95% CI, 0.639–0.850), and 0.687 (95% CI, 0.619–0.755), respectively. The AUC for HOB was the largest, indicating that it had the greatest influence on the success of ECV. However, there were no statistically significant differences among the AUCs. The
P-value for the AUC between AFI and HOB was 0.213, between AFI and parity was 0.685, and between HOB and parity was 0.348 (
Fig. 2). The cut-off value of HOB was 6 cm.
Fig. 2
Receiver operating characteristics curve and AUC for validity test with HOB, parity, AFI for prediction of successful external cephalic version.
AUC, areas under the curve; SE, standard error; CI, confidence interval; AFI, amniotic fluid index; HOB, height of elevated fetal buttock.
Discussion
Our study found that HOB, measured (or determined) by the supervisor (clinical surgeon), might be the most useful predictor of successful ECV compared to other factors such as parity and AFI. The optimal cut-off value of HOB was 6 cm.
According to a recent study in the United States, the ECV success rate was 57.2% in the 4,981 ECV attempts from 2003 to 2014 [
4]. In this study from 2016 to 2018, the success rate was 82% in 114 patients with successful ECV among a total of 139 patients. In accordance with the previous study, 188 out of 290 ECV trials from 2013 to 2017 were successful, and the overall success rate was 64.8%. The success rate was 80% in the recent 100 ECV attempts [
7].
Among previous studies investigating the predictable factors for successful ECV, Burgos et al. [
6] found that parity, placental location, AFI, and the type of breech presentation were associated with successful ECV. Additionally, Kok et al. [
8] found placental location as a significant factor. Mowat and Gardener [
9] noted that multiparity and AFI were predictable factors for successful ECV, whereas lower AFI and nulliparity reduced the success rate of ECV. Similar to previous studies, our study also found parity and AFI to be helpful predictors of successful ECV in addition to HOB. Our study also found that the presence of myoma was a significant predictor of unsuccessful ECV in the univariate analysis; however, it was non-significant in the multivariate analysis. Yoshida et al. [
10] reported that the presence of myoma is not significantly associated with ECV success or failure (
P=0.180).
There are some strengths of this study. To our knowledge, HOB is a secondary marker that can comprehensively reflect the basic and elementary factors, such as maternal age, maternal BMI, parity, EBW, AFI, type of breech, uterine tone, and location of the placenta. As this study shows, HOB is an important and reliable predictor of successful ECV. HOB measurement is noninvasive and safe for the fetus, without any complications, such as fetal distress or rupture of membranes. The procedure does not cause any maternal discomfort. In addition, this predictive factor has the largest AUC compared to other previously known significant factors, such as parity and AFI. The optimal cut-off value of HOB, which was 6 cm on the ROC curve, was selected as the maximal value in the Youden's Index (sensitivity+specificity-1). When the cut-off value of HOB is over 6 cm, the success rate can reach the maximum potential. Therefore, HOB is a significant marker in evaluation of ECV success rate and safe ECV.
The limitation of our study was the small sample size. More cases and further studies are necessary for generalizable findings. Although HOB had a greater AUC compared to parity or AFI on the ROC curve, no statistical significance was observed. Therefore, a larger sample size is necessary. Another limitation was a possible error in measuring HOB. Although the measurements were performed by the same surgeon, the assistant was different. However, compared to AFI, which is measured at 4 sites on the mother's abdomen and can be affected by fetal movement, the error in HOB measurement is likely to be lower.
We conclude that HOB is a noninvasive, convenient, and comprehensive marker of efficient and safe ECV and can be used for wide adoption of ECV.