This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
Primary dysmenorrhea occurs in more than 50% of women of reproductive age. This survey evaluated the effects of Menstrugole on the alleviation of primary dysmenorrhea.
Methods
This study was performed in western Iran between August 15 and December 15, 2017, in female students with primary dysmenorrhea. The students were randomly divided into 2 groups and received placebo or a Menstrugole capsule for 3 days in each of 2 menstrual cycles. The visual analog scale was used to assess pain severity. The χ2 test, one-way analysis of variance, and the paired t-test were used for statistical evaluation.
Results
We compared the severity of pain between the 2 groups. There was a significant change in the mean pain score during the first (P<0.001) and second months (P<0.001) after the use of Menstrugole, compared with that in the placebo group.
Conclusion
Menstrugole decreased pain severity in female students, and can be considered by health care providers for treatment of primary dysmenorrhea.
Keywords: Dysmenorrhea, Adolescent, Analgesics
Introduction
Primary dysmenorrhea occurs in more than 50% of women of reproductive age. It is usually defined as cramping pain in the lower abdomen with onset of menstruation and within 6–12 months after menarche in the absence of pelvic disease. The prevalence of primary dysmenorrhea is 30–90% in different countries [
12]. It is distinguished from secondary dysmenorrhea, which is due to pelvic pathology such as endometriosis.
Nonsteroidal anti-inflammatory drugs and oral hormonal contraceptives have been used to reduce symptoms of dysmenorrhea, although side effects may not be well tolerated [
3]. Alternative and complementary treatments for dysmenorrhea include herbal and dietary therapies, behavioral intervention, acupressure, spinal manipulation, transcutaneous electrical nerve stimulation, and acupuncture [
4567].
Menstrugole is used as an analgesic and antispasmodic drug in primary dysmenorrhea. A capsule contains about 80 mg of dried extract of
Apium graveolens (celery),
Pimpinella anisum (anise), and
Crocus sativus (saffron). The essential oils have antispasmodic effects and the main contributor to this effect is anethole, which is found in anise. Anethole has a chemical composition similar to that of catecholamines such as adrenaline, noradrenalin, and dopamine [
3]. Studies have demonstrated the antineoplastic, antiarthritic, and powerful antioxidant activity of saffron [
8]. Anise seeds are used for analgesic, carminative, aromatic, disinfectant, and diuretic effects in traditional medicine. Menstrugole is effective in reducing menstrual pain through its effect on smooth muscle contraction and because its components (saffron, anise, and celery) have a soothing and anti-inflammatory effect. Therefore, Menstrugole induces menstruation and decreases lumbar and cramping pain [
9]. This herbal remedy is available in the Iranian market, but studies on Menstrugole are limited. Only one study was performed in Iran by Shadipour et al. [
10] in 2014. They indicated that Menstrugole diminished postpartum pain. There are no reports of the effect of Menstrugole for primary dysmenorrhea. Thus, the purpose of this survey was to evaluate the effect of Menstrugole on the treatment of primary dysmenorrhea.
Materials and methods
The present clinical trial was performed on female students in Hamadan University of Medical Sciences between August 15 and December 15, 2017. After receiving approval from the Research Ethics Committee of Hamadan University of Medical Sciences, we registered this survey at
www.irct.ir as
IRCT201707306888N18. Written voluntary consent was taken from all students. This survey was conducted according to Consolidated Standards of Reporting Trials guidelines.
Inclusion criteria for this survey were as follows: 1) age 19–23 years, 2) single status, 3) history of regular menstrual cycles and pain score more than 3 on the visual analog scale (VAS), 4) no use of hormonal treatments or other drugs to alleviate menstrual pain, and 5) no history of major psychological disorder. All students underwent ultrasound to rule out secondary dysmenorrhea. VAS pain scores were used to classify 3 groups; <3, mild dysmenorrhea; 4–6, moderate dysmenorrheal; and >6 severe dysmenorrhea. We excluded cases with mild dysmenorrhea.
Based on a report by Moslemi et al. [
11], a sample size of 80 students (40 students in each group) was required in the present study based on the desired precision level=0.7 and standard deviation=0.8, with 95% power scale and significance level of 0.05. We used balance block randomization and students were randomly divided to 2 groups. For the same purpose, we provided 4 paper cards and wrote “M” for “Menstrugole” on 2 and “P” for “placebo” on 2. The cards were pooled in a dish and randomly chosen for each student without substitution until all 4 cards were chosen. Subjects and the drug distributor were not aware of the contents of the medications. Participants received medication 3 times per day. The experimental group (oral Menstrugole capsules, 500 mg of dried extracts of celery, saffron, and anise) and placebo group (starch) were each treated from the first to the third day of menstruation for 2 cycles. We distributed Menstrugole capsules and placebo in similar packages. The VAS was used to measure changes in the dysmenorrhea pain score. Subjects were asked to evaluate the severity of dysmenorrhea with a checkmark on a 10-cm vertical line (0=no pain to 10=severe pain). The scores were determined at different times in the 2 groups and the mean scores were calculated. We compared the pain scores in the 2 groups with the
t-test and considered
P-values <0.05 statistically significant. SPSS version 16 (IBM Corp., Chicago, IL, USA) was used for statistical analysis.
Results
Of 122 students assessed for eligibility, 42 did not meet the inclusion criteria, and 79 were evaluated (39 in the Menstrugole group and 40 in the placebo group) (
Fig. 1). One student in the Menstrugole group did not return for follow-up. The mean ages of students were 21.50±1.26 and 21.45±1.22 years in the placebo and Menstrugole groups, respectively. The mean age at menarche was 13.10±2.06 and 14.40±1.26 years in the placebo and Menstrugole groups, respectively. The mean body mass index was 21.87±1.60 and 21.87±1.70 (kg/m
2) in the placebo and Menstrugole groups, respectively. Significant differences were not found between the 2 groups in baseline characteristics (
Table 1).
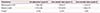
Table 2 shows the pain scores in the 2 groups (
t-test).
Fig. 1
Flow of participants through the trial.

Table 1
Baseline characteristics of participants by units of research

|
Characteristics |
Placebo group (n=40) |
Menstrugole group (n=39) |
NS |
|
Age (yr) |
21.50±1.26 |
21.45±1.22 |
0.998 |
|
Menarche age (yr) |
13.10±2.06 |
14.40±1.26 |
0.221 |
|
Body mass index (kg/m2) |
21.87±1.60 |
21.87±1.70 |
0.877 |
Table 2
Comparison of changes in mean pain scores by units of research
|
Treatments |
On admission (cycle 0) |
One month later (cycle 1) |
Two months later (cycle 2) |
|
Menstrugole (n=39) |
7.28±1.60 |
1.92±0.47 |
1.22±0.42 |
|
Placebo (n=40) |
7.57±1.64 |
7.47±0.55 |
7.68±0.79 |
|
P-valuea)
|
0.260 |
<0.001 |
0.001 |
Table 2 shows data from before and in the first and second months after the intervention in the placebo and Menstrugole groups. There were significant changes in the mean pain scores (baseline minus average after intervention) during the first (
P<0.001) and second months (
P<0.001) after use of Menstrugole in comparison with the placebo group. No side effects were observed after Menstrugole use.
Discussion
This study evaluated the effect of Menstrugole on primary dysmenorrhea. The results indicated that Menstrugole can be an effective nonpharmacological medication for primary dysmenorrhea in the first and second months after initiating use. This traditional Iranian medicine has analgesic, carminative, aromatic, disinfectant, and diuretic effects.
In 2014, Shadipour et al. [
10] examined the effect of Menstrugole on pain. They reported that mefenamic acid and Menstrugole were both useful in reducing postpartum pain. Their analysis revealed that Menstrugole and mefenamic acid were comparable in their ability to reduce pain. However, the effect of Menstrugole began later than that of mefenamic acid.
In the present study, the small sample size was a main limitation. A larger sample size can identify differences between trial groups with less error. In addition, the survey was performed in single teenagers and the results cannot be generalized to a larger population.
Traditional treatments rather than modern techniques have been preferred by Iranian women for relief of gynecological symptoms. This survey reported that Menstrugole is useful in decreasing primary dysmenorrhea. Most nonsteroidal anti-inflammatory drugs showed severe adverse effects with long-term use [
12], but Menstrugole showed no side effects. Thus, Menstrugole can be an alternative to nonsteroidal anti-inflammatory drugs.
In conclusion, Menstrugole decreased pain severity in female students, and should be considered for treatment of primary dysmenorrhea.
Acknowledgements
We would want to thank the Vice-chancellor of Search and Technology, Hamadan University of Medical Sciences, Hamadan, Iran, for financial support of this survey.
References
1. Daily JW, Zhang X, Kim DS, Park S. Efficacy of ginger for alleviating the symptoms of primary dysmenorrhea: a systematic review and meta-analysis of randomized clinical trials. Pain Med. 2015; 16:2243–2255.

2. Shobeiri F, Jenabi E, Hajiloomohajeran M, Torkamani M. Investigating the effect of stachys lavandulifolia on pain reduction in women with dysmenorrheal. Complement Med J Fac Nurs Midwifery. 2014; 4:713–719.
3. Dmitrovic R, Kunselman AR, Legro RS. Sildenafil citrate in the treatment of pain in primary dysmenorrhea: a randomized controlled trial. Hum Reprod. 2013; 28:2958–2965.

4. Jenabi E. The effect of ginger for relieving of primary dysmenorrhoea. J Pak Med Assoc. 2013; 63:8–10.
5. Mirabi P, Alamolhoda SH, Esmaeilzadeh S, Mojab F. Effect of medicinal herbs on primary dysmenorrhoea- a systematic review. Iran J Pharm Res. 2014; 13:757–767.
6. Taghi Shakeri M, Jafarnejad F, Dehnavi ZM. The prevalence of the severity of physical and psychological symptoms in premenstrual syndrome in warm and cool temperament after 8 weeks of regular aerobic exercise. Iran J Obstet Gynecol Infertil. 2017; 20:1–12.
7. Jenabi E, Fereidoony B. Effect of achillea millefolium on relief of primary dysmenorrhea: a double-blind randomized clinical trial. J Pediatr Adolesc Gynecol. 2015; 28:402–404.

8. Shojaii A, Abdollahi Fard M.. Review of pharmacological properties and chemical constituents of Pimpinella anisum
. ISRN Pharm. 2012; 2012:510795.
9. Denev RV, Kuzmanova IS, Momchilova SM, Nikolova-Damyanova BM. Resolution and quantification of isomeric fatty acids by silver ion HPLC: fatty acid composition of aniseed oil (Pimpinella anisum, Apiaceae). J AOAC Int. 2011; 94:4–8.
10. Shadipour M, Simbar M, Salamzadeh J, Nasire N. A comparative study on the effects of Menstrogol and Mefenamic acid on postpartum after-pain. Iran South Med J. 2014; 16:401–409.
11. Moslemi L, Aghamohammadi A, Bekhradi R, Zafari M. Comparing the effects of vitamin E and fennel extract on intensity of primary dysmenorrhea. J Mazandaran Univ Med Sci. 2012; 22:103–107.
12. Ostad SN, Soodi M, Shariffzadeh M, Khorshidi N, Marzban H. The effect of fennel essential oil on uterine contraction as a model for dysmenorrhea, pharmacology and toxicology study. J Ethnopharmacol. 2001; 76:299–304.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download