This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To compare the clinical pregnancy rate (CPR) and ongoing pregnancy rate (OPR) in frozen embryo transfers (FETs) following either freeze-all policy to prevent ovarian hyperstimulation syndrome (OHSS; freeze-all group) or excess embryo cryopreservation after fresh embryo transfer (surplus group).
Methods
The freeze-all group comprised 44 FET cycles performed in 25 women between 2010 and 2016. The surplus group comprised 53 FET cycles performed in 47 women during the same period. The cumulative CPR and OPR according to duration of cryopreservation (interval between cryopreservation and FET) was estimated using Kaplan-Meier plots. Cox regression analysis was used for identifying factor to affect to cryopreservation duration in cycles with pregnancy.
Results
In day 2–4 transfer cycles, the crude CPR (40% vs. 18.2%) and OPR (20% vs. 4.5%) were similar between the 2 groups. In day 5 transfer, the crude CPR (33.3% vs. 38.7%) and OPR (33.3% vs. 29%) were also similar between the 2 groups. The cumulative CPR (100% vs. 47.5%) and OPR (100% vs. 33.3%) in day 2–4 transfer as well as the cumulative CPR (46.7% vs. 100%) and OPR (46.7% and 74.8%) in day 5 transfer were also similar between the 2 groups. The median duration of cryopreservation was significantly shorter in the freeze-all group than in the surplus group (19.8 vs. 36.9 weeks, P=0.04). Previous history of delivery was the only factor associated with a shorter cryopreservation duration in cycles with pregnancy (hazard ratio, 0.18; 95% confidence interval, 0.05–0.65; P=0.01).
Conclusion
Freezing embryos to prevent OHSS and transferring the frozen embryos later may guarantee an acceptable reproductive outcome.
Keywords: Frozen embryo transfer, Cryopreservation, Ovarian hyperstimulation syndrome
Introduction
How long does it take for the infertile couples to conceive following assisted reproductive technique? It is probably of greatest interest to both infertile couples and clinicians. Patients undergoing in vitro fertilization (IVF) cycles may not receive embryo transfer (ET) at that controlled ovarian stimulation (COS) cycle for several reasons. Whether the ET in that cycle was unsuccessful or ET was not performed, frozen embryo transfer (FET) would be performed thereafter if the embryos have been cryopreserved. Focusing on the FET cycle, it is uncertain whether there is a difference in the pregnancy outcome between the cycles following either freeze-all policy or failed fresh ET.
FET has been increasing continuously since the first report of successful pregnancy following FET [
12]. Advances in freezing-thawing techniques led to a 95% survival rate after thawing [
34]. The reliable survival rate gave rise to the freeze-all policy, a strategy to perform elective cryopreservation of all embryos without ET in fresh IVF cycles and to transfer the embryos in future frozen-thawed cycles. This policy has the additional advantage of placing embryos in a more favorable endometrium without the adverse effect of supra-physiologic levels of estrogen on the endometrium [
56]. The freeze-all policy is commonly applied for prevention of ovarian hyperstimulation syndrome (OHSS) in high responders [
7].
The OHSS is a potentially life-threatening iatrogenic complication of stimulated IVF cycles, which occurs in 1–14% of IVF cycles [
89]. During COS, high response to stimulation (multiple follicles >18, high preovulatory estradiol concentration >5,000 pg/mL) has been known to be a risk factor for OHSS [
10]. Other risk factors include polycystic ovaries on ultrasound, young age, and lean habitus. There are several preventive measures for this unwanted complication of ovarian stimulation, and freeze-all policy with later FET is the most preferred option.
Since the occurrence of late-onset OHSS depends on the rise in human chorionic gonadotropin (hCG) levels following implantation of the transferred embryos, late-onset OHSS can be almost completely prevented by avoiding ET. Early-onset OHSS, which is caused by administration of hCG for oocyte maturation, cannot be fully prevented by freeze-all policy, but the management of OHSS is more flexible given that there is no possibility of pregnancy [
11121314].
The clinical pregnancy rate (CPR) has been reported to be between 35.4% and 48.3% in FET cycles following freeze-all policy to prevent OHSS [
1516]. However, it is unclear whether this rate is higher or lower than those in FET cycles utilizing surplus embryos, which are more commonly performed. There was a possibility of reduced CPR in the freeze-all group, since reduced oocyte quality was reported in patients with severe OHSS [
17]. The only available study that compared outcomes of FET cycles according to the purpose of embryo freezing also raised concerns regarding the lower quality of embryos following freeze-all policy [
16]. Furthermore, the association between the duration of embryo freezing and CPR was not assessed in previous reports on FET cycles.
In this study, we retrospectively compared CPR and ongoing pregnancy rate (OPR) in FET cycles after freeze-all policy to prevent OHSS and in FET cycles utilizing surplus embryos.
Materials and methods
This was a retrospective study to compare the CPR and OPR in FET cycles using frozen embryos for 2 different purposes: freeze-all policy to prevent OHSS (freeze-all group) versus freezing of surplus embryos in conjunction with fresh ET (surplus group). FET cycles performed between 2010 and 2016 in 2 fertility centers (Seoul National University Bundang Hospital and the M Fertility Center) were selected. The following cycles were excluded: gestational surrogacy, cycles that used embryos derived from oocytes retrieved during surgery, and FET performed several days after a failed retrieval of the mature oocyte in the fresh cycle. A total of 97 FET cycles (in 72 women) were included in this study. This study was reviewed and approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1703/385-103).
Basic patient characteristics (women's age at the time of embryo freezing and FET, indications for IVF) and cycle characteristics, methods of endometrial preparation, endometrial thickness (EMT), number and quality of embryos transferred, duration of cryopreservation (interval between cryopreservation and FET), and pregnancy outcomes were retrieved from medical records.
For endometrial preparation, estradiol valerate (EV) and intramuscular (IM) progesterone was sequentially administered in 86 cycles. Ten cycles were performed without hormone replacement (natural cycle protocol with hCG administration) and one cycle was performed after administration of letrozole for 5 days (ovulation induction protocol). For the natural cycle protocol, no medication was administered for endometrial preparation except an IM injection of hCG. Urinary hCG (10,000 IU of IVF-C; LG Chemical, Seoul, Korea) was administered for ovulation when the dominant follicle reached a diameter of 18–20 mm as observed on ultrasound monitoring. The EMT was measured on the day of hCG triggering. In the hormonal replacement cycle, endometrial preparation was achieved with oral administration of EV and IM progesterone without prior pituitary suppression. A daily dose of 6 mg oral EV (Progynova, Bayer, Germany) was initiated on the third day of the menstrual cycle and was administered continuously. A daily IM injection of 50 mg progesterone in oil (Genefer progesterone; Genefer, Seoul, Korea) was started when the EMT exceeded 7 mm. Since the EMT <7 mm have been reported to have a low chance to conceive after IVF, if the EMT <7 mm after 8 days of EV administration, the dose of EV was increased to 8 mg per day [
18].
The quality of embryos at the time of FET was evaluated using morphological criteria based on the degree of fragmentation and the regularity of blastomeres on day 2–4 after fertilization as follows: grade A, equal-sized blastomeres and no fragments or apparent morphologic abnormalities; grade B, equal-sized blastomeres and <20% of fragments without apparent morphologic abnormalities; grade C, irregularity of blastomeres and 20–50% of fragments without apparent morphologic abnormalities; grade D, irregularity of blastomeres and >50% fragments with apparent morphologic abnormalities. A good-quality embryo was defined as an embryo that was assigned grade A or grade B. The blastocyst was evaluated on day 5 based on the blastocyst development stage and the quality of the inner cell mass and trophectoderm. A good-quality blastocyst was defined as a blastocyst that was assigned grade AA, AB, AC, BA, BB, or CA. The thawed embryos were transferred after evaluation without further incubation.
Clinical pregnancy was defined as detection of intrauterine gestational sac(s) with fetal heartbeat(s) on ultrasound. Ongoing pregnancy was defined as continued pregnancy beyond 12 weeks' gestation. Both CPR and OPR was calculated using the number of cycles with successful ETs as the denominator. The miscarriage rate was calculated as the proportion of cycles with miscarriage among the cycles with confirmed clinical pregnancy.
Numerical variables were presented as medians (95% confidence interval [CI]), and categorical variables were presented as counts (percentages). Patient characteristics were compared between the 2 groups using the Mann-Whitney U test for continuous variables and the χ2 test or Fisher's exact test for categorical variables.
To estimate the cumulative CPR and OPR according to duration of cryopreservation, a technique to analyze the data using survival analysis was required [
19]. In our survival analysis, the event was conception, and women “survived” until they conceive. Censorship occurred when patients cease to undergo IVF, or at the end of the study period. We used the duration of cryopreservation as the time variable instead of the duration of expectancy. The cumulative CPR and OPR were estimated using the Kaplan-Meier method [
20]. The Kaplan-Meier curves for the freeze-all group and surplus group were compared using the log-rank test. Cox regression analysis was used to calculate the hazard ratios (HRs) and 95% CIs of the factors that affect the cryopreservation duration in cycles with pregnancy. Statistical analysis was performed using SPSS version 22.0 (IBM Crop., Armonk, NY, USA). A
P-value <0.05 was considered statistically significant.
Results
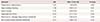
The clinical outcomes of FET cycles are presented in
Table 1. Women's age, either at embryo freezing or FET, was similar between the 2 groups. However, the median duration of cryopreservation was significantly shorter in the freeze-all group than in the surplus group. The duration of cryopreservation ranged from 2.4 to 91.4 weeks in the freeze-all group and from 4.1 to 237.3 weeks in the surplus group.
Table 1
Clinical outcomes of frozen embryo transfer cycles in the freeze-all group and the surplus group

|
Variable |
Freeze-all group |
Surplus group |
P
|
|
No. of patients |
25 |
47 |
|
|
Patients who underwent 2 FET cycles |
7 |
4 |
|
Patients who underwent 3 or more FET cycles |
5 |
1 |
|
No. of transfer cycles |
44 |
53 |
<0.001 |
|
Day 2–4 transfer |
35 (79.5) |
22 (41.5) |
|
Day 5 transfer |
9 (20.5) |
31 (58.5) |
|
Age at embryo freezing (yr) |
34 (33–36) |
35 (33–36) |
NS |
|
Age at FET (yr) |
35 (33–37) |
35 (35–37) |
NS |
|
Interval between embryo freezing and FET (wk) |
12.1 (9–16.9) |
17 (9–24) |
0.040 |
|
Parous condition |
4 (9.1) |
17 (32.1) |
0.006 |
|
Indications of IVF |
|
|
|
|
Male factor |
5 (11.4) |
11 (20.8) |
NS |
|
Tubal factor |
3 (6.8) |
11 (20.8) |
NS |
|
PCOS |
17 (38.6) |
1 (1.9) |
<0.001 |
|
Endometriosis |
2 (4.5) |
5 (9.4) |
NS |
|
Uterine factor |
0 (0) |
4 (7.5) |
NS |
|
Old age |
11 (25) |
13 (24.5) |
NS |
|
Unexplained |
5 (11.4) |
7 (13.2) |
NS |
|
Combined factors |
1 (2.3) |
0 (0) |
NS |
|
Endometrial preparation |
|
|
NS |
|
Hormonal replacement |
37 (84.1) |
49 (92.5) |
|
Natural |
7 (15.9) |
3 (5.7) |
|
Letrozole |
0 (0) |
1 (1.9) |
|
Endometrial thickness (mm)a)
|
8.5 (8–9) |
8.1 (7.7–8.7) |
NS |
|
No. of embryos transferred |
|
|
|
|
Day 2–4 transfer |
3 (2–3) |
3 (2–3) |
NS |
|
Day 5 transfer |
2 (2–2) |
2 (2–2) |
NS |
|
No. of good-quality embryos |
|
|
|
|
Day 2–4 transfer |
0 (0–1) |
1 (0–2) |
NS |
|
Day 5 transfer |
2 (2–2) |
2 (2–2) |
NS |
|
Clinical pregnancy (% per transfer cycle) |
|
|
|
|
Day 2–4 transfer |
14 (40) |
4 (18.2) |
NS |
|
Day 5 transfer |
3 (33.3) |
12 (38.7) |
NS |
|
Ongoing pregnancy (% per transfer cycle) |
|
|
|
|
Day 2–4 transfer |
7 (20) |
1 (4.5) |
NS |
|
Day 5 transfer |
3 (33.3) |
9 (29) |
NS |
|
Miscarriage (% per clinical pregnancy) |
|
|
|
|
Day 2–4 transfer |
7 (50) |
3 (75) |
NS |
|
Day 5 transfer |
0 (0) |
2 (16.7) |
NS |
The proportion of parous women was significantly higher in the surplus group, whilst the polycystic ovary syndrome (PCOS) was more prevalent in the freeze-all group. The method of endometrial preparation and the mean EMT at triggering or progesterone initiation day were similar between the 2 groups.
The mean number of embryos transferred and the mean number of good-quality embryos transferred at either day 2–4 or day 5 were similar between the 2 groups. Interestingly, the proportion of day 5 transfer was significantly lower in the freeze-all group. The crude CPR, OPR, and miscarriage rate in either day 2–4 transfer or day 5 transfer cycles was similar between the 2 groups (
Table 1).
The estimated cumulative CPR and OPR in day 2–4 transfer cycles based on the duration of cryopreservation are depicted in
Fig. 1. In the freeze-all group, cumulative CPR and OPR showed a similar pattern of an initial steep increase until 22.7 weeks followed by a plateau. In contrast, cumulative CPR and OPR reached a plateau at 33.6 weeks in the surplus group. Both cumulative CPR and OPR were higher in the freeze-all group than in the surplus group, but the difference was not statistically significant. In detail, the estimated cumulative CPR was 100% and 47.5%, in the freeze-all and surplus groups, respectively (
P=0.07,
Fig. 1A), and the estimated cumulative OPR was 100% and 33.3%, in the freeze-all and surplus groups, respectively (
P=0.06,
Fig. 1B).
Fig. 1
Kaplan-Meier estimates of (A) cumulative clinical pregnancy rate and (B) cumulative ongoing pregnancy rate based on the interval between embryo freezing at day 2–4 and frozen embryo transfer.

The estimated cumulative CPR and OPR in day 5 transfer cycles based on the duration of cryopreservation are shown in
Fig. 2. In the freeze-all group, cumulative CPR and OPR reached a plateau at 15.9 weeks, whilst cumulative CPR and OPR increased steadily until the end of the follow-up period in the surplus group. The estimated cumulative CPR was 46.7% and 100%, in the freeze-all and surplus groups, respectively (
P=0.50,
Fig. 2A), and the estimated cumulative OPR was 46.7% and 74.8%, in the freeze-all and surplus groups, respectively (
P=0.37,
Fig. 2B).
Fig. 2
Kaplan-Meier estimates of (A) cumulative clinical pregnancy rate and (B) cumulative ongoing pregnancy rate based on the interval between embryo freezing at day 5 and frozen embryo transfer.

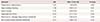
Cox regression analysis showed that the cryopreservation duration in cycles with pregnancy was significantly shorter in parous women (HR, 0.18; 95% CI, 0.05–0.65;
P=0.01,
Table 2). No other variables consistently predicted shorter cryopreservation duration in cycles with pregnancy.
Table 2
Cox regression analysis of factors predicting the cryopreservation duration in cycles with pregnancy
|
Variable |
HR |
95% CI for HR |
P
|
|
Freeze-all (vs. surplus) group |
2.62 |
1.00–6.89 |
0.05 |
|
Age at embryo freezing |
1.06 |
0.93–1.21 |
0.41 |
|
Parous women |
0.18 |
0.05–0.65 |
0.01 |
|
Diagnosed with PCOS |
0.33 |
0.11–1.02 |
0.05 |
|
Blastocyst (vs. cleavage) stage embryo transferred |
2.65 |
0.85–8.24 |
0.09 |
|
No. of good-quality-embryos transferred |
0.75 |
0.46–1.20 |
0.23 |
Discussion
In the present retrospective study, we demonstrated that the pregnancy rate for FET cycles using embryos from freeze-all policy to prevent OHSS was comparable to the pregnancy rate for FET cycles using surplus embryos. This is in agreement with the results from a retrospective study by Horwath et al. [
16]. They showed similar pregnancy rates between a freeze-all group and 4 other groups of different indications.
In the present work, we demonstrated for the first time that the estimated cumulative CPR and OPR based on the duration of embryo cryopreservation is similar between the freeze-all group and the surplus group, regardless of the day of ET. Based on our findings, PR for FET cycles using embryos from freeze-all policy to prevent OHSS reached a plateau at around 23 weeks in day 2–4 transfer cycles and at around 16 weeks in day 5 transfer cycles. Thus, we recommend these time intervals to maximize the PR for FET cycles using embryos from freeze-all policy. The optimal time interval between embryo freezing and FET has been unknown, but our findings may help clinicians to determine when FET should be performed.
The median duration of cryopreservation was significantly shorter in the freeze-all group than in the surplus group. This phenomenon might be associated with a tendency to transfer embryos earlier in the freeze-all group. As women in the freeze-all group did not receive fresh ET, they might wish subsequent FET immediately or earlier time after embryo cryopreservation. In a recent study, there was no difference in PR of FET cycles using embryos from freeze-all policy to prevent OHSS, whether it was performed immediately after embryo freezing or after 2 menstrual cycles [
21]. In the surplus group, FET might be delayed for several reasons. Some patients may want a rest period to recover after failed fresh ET. Some patients may visit infertility clinics because they want a second baby after a successful delivery following fresh ET.
The most prominent feature of our study is that we derived the estimates for cumulative PR according to the duration of cryopreservation by the Kaplan-Meier method. However, more studies would be needed to verify similar cumulative PR according to the duration of cryopreservation in the 2 groups because the period of observation was not similar between the groups in our study.
Here, we demonstrated that freeze-all embryo policy for prevention of OHSS and later transfer of frozen embryos might guarantee an acceptable PR, which is similar to the FET utilizing surplus embryos. The PR was similar between the 2 groups in either day 2–4 or day 5 transfers. Nonetheless, the proportion of day 5 transfers was significantly lower in the freeze-all group; thus, more studies would be needed to verify our finding.
The reason for the lower proportion of day 5 transfer in the freeze-all group is largely unknown. In general, many embryos transferred at day 2–4 do not survive until the blastocyst stage. The fear of “no blastocysts available” after further culture might lead to a tendency of early freezing. In contrast, the clinicians may choose to culture surplus embryos up to the blastocyst stage for later use in the surplus group, since a fresh ET has already been performed, and the cryopreserved embryos are for backup in case the women fails to get pregnant.
Unless other adjuvant agents are used before or during endometrium preparation, the EMT and the embryo quality are the 2 most crucial factors affecting pregnancy. However, there was no difference in EMT before FET as shown in
Table 1. It is a common belief that the best quality embryos are used in the fresh ET cycles, and the remaining (surplus) are lower quality embryos. However, there was no difference in embryo quality between surplus embryos and embryos in the freeze-all group when we compared the number of good-quality-embryos in our study.
The proportion of patients with PCOS was obviously higher in the all-freezing group, since the group represent the high-responders. The uneven distribution of PCOS patients in the 2 groups was an important confounder since PCOS patients generally have a lower chance of pregnancy. Poor endometrial function and poor embryo quality have been suggested as possible explanations for the low pregnancy rate in patients with PCOS [
1722]. In our study, when adjusted for other variables in the Cox regression analysis, the diagnosis of PCOS did not show a significant association with the cryopreservation duration in cycles with pregnancy. There were also known differences between lean or obese PCOS patients, we were not able to describe characteristics of obese PCOS and lean PCOS separately since not all medical records had weight and height information. In the multivariate Cox regression analysis, there was no difference in cryopreservation duration in cycles with pregnancy between freeze-all group and surplus group. Parous condition was the only significant factor associated with shorter cryopreservation duration in cycles with pregnancy possibly reflecting the less severe conditions associated with infertility.
In conclusion, we demonstrated that freeze-all policy for prevention of OHSS and a later transfer of frozen embryos might guarantee an acceptable PR. We proposed that FET should be performed within 23 weeks in day 2–4 transfer cycles and within 16 weeks in day 5 transfer cycles in case of freezing all embryos to prevent OHSS.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download