Abstract
Objective
Placental growth factor (PlGF) is one of the many angiogenic factors, which is decreased in placenta and serum during preeclampsia (PE) and also associated with pregnancies complicated by small for gestational age. In this study, we compared serum PlGF levels with different groups (controls, PE patients, pregnant women with small for gestational age [SGA]) and evaluated the usefulness of PlGF for diagnosis.
Methods
Serum samples were collected at the time of delivery from 40 women with uncomplicated pregnancies, 30 women with PE, 30 women with pregnancies complicated by SGA fetuses. Serum PlGF level was measured in all the samples using Triage PlGF test. We used the Kruskal-Wallis test and receiver operator characteristic curve analysis.
Results
Maternal serum PlGF concentrations in pregnancies complicated by PE (21.17 ± 15.27 pg/mL) were significantly lower than those in uncomplicated pregnancies (133.70 ± 158.80 pg/mL, P<0.01) and PlGF concentrations were decreased in pregnancies complicated by SGA fetuses (95.65 ± 210.36 pg/mL) compared with control group, but there was no statistically significant difference.
Conclusion
Decreased PlGF concentrations were observed in pregnancies complicated by PE and SGA. PlGF concentrations in pregnancies complicated by PE was significantly lower than those in uncomplicated pregnancies. By further prospective investigation, we may expect that the PlGF levels during pregnancy will be a marker to identify women at risk for the development of PE and SGA.
Figures and Tables
Fig. 1
Log 10 PlGF concentrations with gestational age in control women, pregnancies with SGA and PE. PlGF, placental growth factor; PE, preeclampsia; SGA, small for gestational age.

Fig. 2
Receiver operator characteristic curves for PlGF discrimination of control vs. PE (area under curve, 0.837; 95% CI, 0.724 to 0.951). Cutoff values of 65.1 pg/mL had 93.3% sensitivity and 68% specificity. PlGF, placental growth factor; PE, preeclampsia; SGA, small for gestational age; CI, confidence interval.

Fig. 3
Receiver operator characteristic curves for PlGF discrimination of control vs. SGA (area under curve, 0.771; 95% CI, 0.622 to 0.919). Cutoff values of 59.25 pg/mL had 81.8% sensitivity and 68% specificity. PlGF, placental growth factor; PE, preeclampsia; SGA, small for gestational age; CI, confidence interval.
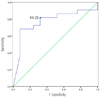
Table 1
Clinical characteristics of study population
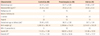
Values are given as mean ± standard deviation and statistical significance was assessed by the Kruskal-Wallis test.
SGA, small for gestational age; BMI, body mass index; BW, birth weight; BP, blood pressure.
aP <0.05, Preeclampsia vs. SGA; bP <0.05, Control vs. Preeclampsia, Control vs. SGA; cP <0.05, Control vs. Preeclampsia, Control vs. SGA, Preeclampsia vs. SGA; dP <0.05, Control vs. Preeclampsia, Preeclampsia vs. SGA.
References
1. Redman CW, Sargent IL. Latest advances in understanding preeclampsia. Science. 2005. 308:1592–1594.
2. Roberts JM, Lain KY. Recent Insights into the pathogenesis of pre-eclampsia. Placenta. 2002. 23:359–372.
3. Torry DS, Torry RJ. Angiogenesis and the expression of vascular endothelial growth factor in endometrium and placenta. Am J Reprod Immunol. 1997. 37:21–29.
4. Villee CA, Grigorescu A, Reddy PR. Androgen regulation of RNA synthesis in target tissues. J Steroid Biochem. 1975. 6:561–565.
5. Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004. 350:672–683.
6. Knudsen UB, Kronborg CS, Dadelszen P, Kupfer K, Lee SW, Vittinghus E, et al. A single rapid point-of-care placental growth factor determination as an aid in the diagnosis of preeclampsia. Pregnancy Hypertens. 2012. 2:8–15.
7. Romero R, Nien JK, Espinoza J, Todem D, Fu W, Chung H, et al. A longitudinal study of angiogenic (placental growth factor) and anti-angiogenic (soluble endoglin and soluble vascular endothelial growth factor receptor-1) factors in normal pregnancy and patients destined to develop preeclampsia and deliver a small for gestational age neonate. J Matern Fetal Neonatal Med. 2008. 21:9–23.
8. Benton SJ, Hu Y, Xie F, Kupfer K, Lee SW, Magee LA, et al. Can placental growth factor in maternal circulation identify fetuses with placental intrauterine growth restriction? Am J Obstet Gynecol. 2012. 206:163.e1–163.e7.
9. Report of the National High Blood Pressure Education Program Working Group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000. 183:S1–S22.
10. Verlohren S, Galindo A, Schlembach D, Zeisler H, Herraiz I, Moertl MG, et al. An automated method for the determination of the sFlt-1/PIGF ratio in the assessment of preeclampsia. Am J Obstet Gynecol. 2010. 202:161.e1–161.e11.
11. Verlohren S, Herraiz I, Lapaire O, Schlembach D, Moertl M, Zeisler H, et al. The sFlt-1/PlGF ratio in different types of hypertensive pregnancy disorders and its prognostic potential in preeclamptic patients. Am J Obstet Gynecol. 2012. 206:58.e1–58.e8.
12. Benton SJ, Hu Y, Xie F, Kupfer K, Lee SW, Magee LA, et al. Angiogenic factors as diagnostic tests for preeclampsia: a performance comparison between two commercial immunoassays. Am J Obstet Gynecol. 2011. 205:469.e1–469.e8.
13. Sunderji S, Gaziano E, Wothe D, Rogers LC, Sibai B, Karumanchi SA, et al. Automated assays for sVEGF R1 and PlGF as an aid in the diagnosis of preterm preeclampsia: a prospective clinical study. Am J Obstet Gynecol. 2010. 202:40.e1–40.e7.
14. Lee HB, Kil KC, Nam SY, Shin JE, Cheon JY, Lee Y. Clinical usefulness of soluble fms-like tyrosine kinase 1, soluble endoglin and placental growth factor in Korean women with preeclampsia. Korean J Obstet Gynecol. 2011. 54:229–235.
15. Harrington KF, Campbell S, Bewley S, Bower S. Doppler velocimetry studies of the uterine artery in the early prediction of pre-eclampsia and intra-uterine growth retardation. Eur J Obstet Gynecol Reprod Biol. 1991. 42:Suppl. S14–S20.
16. Harrington K, Cooper D, Lees C, Hecher K, Campbell S. Doppler ultrasound of the uterine arteries: the importance of bilateral notching in the prediction of pre-eclampsia, placental abruption or delivery of a small-for-gestational-age baby. Ultrasound Obstet Gynecol. 1996. 7:182–188.
17. Papageorghiou AT, Yu CK, Nicolaides KH. The role of uterine artery Doppler in predicting adverse pregnancy outcome. Best Pract Res Clin Obstet Gynaecol. 2004. 18:383–396.
18. Ness RB, Sibai BM. Shared and disparate components of the pathophysiologies of fetal growth restriction and preeclampsia. Am J Obstet Gynecol. 2006. 195:40–49.
19. Redman CW, Sacks GP, Sargent IL. Preeclampsia: an excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol. 1999. 180:499–506.
20. Johnson MR, Anim-Nyame N, Johnson P, Sooranna SR, Steer PJ. Does endothelial cell activation occur with intrauterine growth restriction? BJOG. 2002. 109:836–839.
21. Nagamatsu T, Fujii T, Kusumi M, Zou L, Yamashita T, Osuga Y, et al. Cytotrophoblasts up-regulate soluble fms-like tyrosine kinase-1 expression under reduced oxygen: an implication for the placental vascular development and the pathophysiology of preeclampsia. Endocrinology. 2004. 145:4838–4845.
22. Shokry M, Bedaiwy MA, Fathalla MM, Alsemary A, Elwakil S, Murphy A. Maternal serum placental growth factor and soluble fms-like tyrosine kinase 1 as early predictors of preeclampsia. Acta Obstet Gynecol Scand. 2010. 89:143–146.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download