Abstract
Epinephrine is one of the most widely-used vasoconstrictors in dental treatment including endodontic microsurgery. However, the systemic safety of epinephrine has been in debate for many years because of its potential risk to cause cardiovascular complications. The purpose of this review was to assess the cardiovascular effect of epinephrine use in endodontic microsurgery. Endodontic microsurgery directly applies epinephrine into the bone cavity, and the amount is reported to be much larger than other dental surgeries. Moreover, when considering that systemic potency of intraosseous application is reported to be comparable to intravenous application, the systemic influence of epinephrine could be increased in endodontic microsurgery. Besides, pre-existing cardiovascular complications or drug interactions can enhance its systemic influence, resulting in increased susceptibility to cardiovascular complications. Although clinical studies have not reported significant complications for patients without severe systemic complications, many epinephrine-induced emergency cases are warning the cardiovascular risk related with pre-existing systemic disease or drug interactions. Epinephrine is a dose-sensitive drug, and its hypersensitivity reaction can be fatal to patients when it is related to cardiovascular complications. Therefore, clinicians should recognize the risk, and the usage of pre-operative patient evaluation, dose control and patient monitoring are required to ensure patient's safety during endodontic microsurgery.
Epinephrine is one of the most widely-used vasoconstrictors in dentistry. However, because of the characteristics as a hormone that influences main organs simultaneously, it has been argued as a potential risk factor that can cause cardiovascular complications. For this reason, many studies have been published to evaluate the safety of epinephrine in dental treatment.1-16 However most of them were conducted with tooth extraction2-13 and periodontal surgery,14 and there have been only few studies for endodontic microsurgery to this date.15,16
Endodontic microsurgery has a unique feature in regard of epinephrine application, especially in intra-operative hemostasis. Almost perfect bleeding control is needed for proper inspection of the resected root surface and retro-filling of the root-end cavity, which are the most important components of endodontic microsurgery.17-19 For this reason, direct application of epinephrine into the bone cavity has been commonly selected by many clinicians, which has been confirmed as an effective way to ensure hemostasis during surgery.17 However, due to additional doses of epinephrine and the administration route (intraosseous route) that affects the systemic circulation more directly than other routes, the systemic influence of epinephrine could be increased in endodontic microsurgery, resulting in increased susceptibility to the cardiovascular complications.15,16,20,21
As the success rate and long-term prognosis of endodontic microsurgery is validated, it is becoming a standard treatment option in the endodontic field.22-24 It is the time to focus on not only the long-term prognosis of endodontic microsurgery, but also the systemic safety during treatments.
Therefore, the purposes of this review were to assess the cardiovascular effect of epinephrine use in endodontic microsurgery, and to make clinical suggestions that can reduce the risk of epinephrine.
Epinephrine is one of the principal hormones that affect adrenergic receptors of autonomic nervous system.25 It modulates various functions of the body simultaneously by affecting different subtypes of the adrenergic receptor. Epinephrine induces vasoconstriction of the mucosa, skin, and internal organs by affecting α1 adrenergic receptor, and increases blood glucose level by affecting α2 adrenergic receptor. It also influences β1 adrenergic receptor to increase cardiac output by changing heart rate and contraction force, and it induces vasodilatation of the skeletal muscles, liver and relaxation of bronchial smooth muscle by affecting β2 receptor.
In the dental field, epinephrine serves as a local vasoconstrictor in local anesthetics or gingival retraction cords.26,27 And it is also used in endodontic microsurgery as a hemostatic agent to control the bleeding in the bone cavity.17 In this way, most dentists only use the effect of epinephrine to α1 receptor.
On the other hand, epinephrine is being used for various purposes in the medical field. It is injected in case of acute hypotensive crisis to elevate the blood pressure immediately, and it is also administered to induce defibrillation in case of cardiac arrest. In acute asthma attack, it is inhaled to induce bronchodilation. Epinephrine is not just a simple hemostatic agent but a hormone that modulates main organs of the body. In this regard, its action on β1 adrenergic receptor can cause unsuspected cardiovascular complications during dental surgery if we are not aware of its nature.
Patients with cardiovascular diseases are increasing in dental practices in recent years. Such patients are vulnerable to the stress induced by dental treatment, and more susceptible to drug side effects compared to healthy patients. Therefore, the possibility of medical emergency during dental treatment is more likely in these patients.
Cardiovascular complications of epinephrine on patients with hypertension have been a concern in dental practice. Bader et al. conducted systematic review to identify cardiovascular complications in hypertensive patients caused by epinephrine contained in anesthetic solutions.1 373 studies were initially searched, and finally six studies of them were analyzed. This revealed that the effect of epinephrine was not significant during dental surgery in hypertensive patients compared with normotensive patients. However, as the author commented, the number of subjects was too small and the information about predisposing medical diagnoses and medication status was restricted. Moreover, analyzed studies were associated with tooth extraction and minor dental surgery, not endodontic microsurgery.
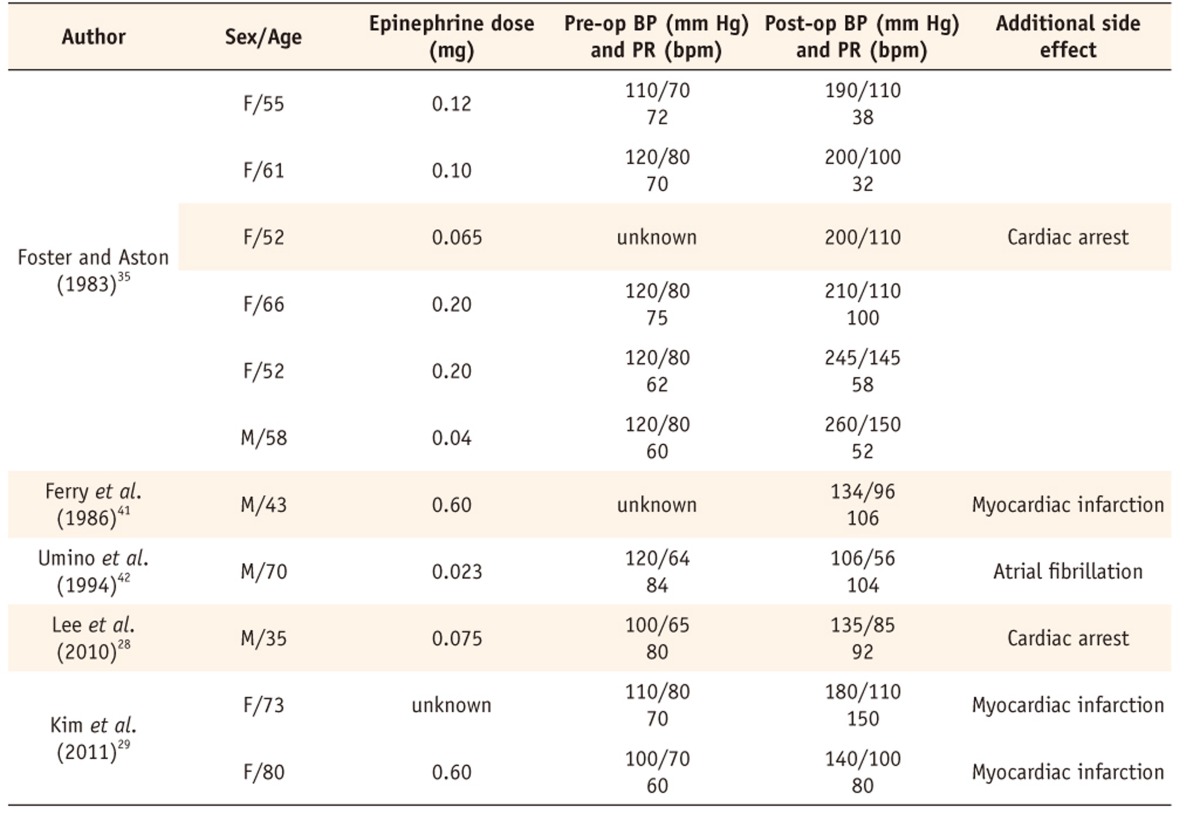
Meanwhile, it is not difficult to find epinephrine emergency cases in patient with pre-existing cardiovascular disease. Lee et al. reported occurrence of cardiac arrest induced by submucosal injection of epinephrine in a patient with variant angina.28 When 1.5% lidocaine with 1 : 100,000 epinephrine was injected (about 7.5 mL) in the nasal mucosa for septoplasty, sudden ventricular tachycardia was observed, followed by cardiac arrest. Kim et al. also reported two cases that showed acute elevation of blood pressure with severe chest tightness during endoscopic submucosal dissection after submucosal injection of 1 : 100,000 epinephrine.29 One of the cases was diagnosed as myocardiac infarction.
Epinephrine induces vasoconstriction on mucosa, skin, and internal organs by affecting α1 adrenergic receptor. It also induces vasodilatation of skeletal muscle by affecting β2 adrenergic receptor at the same time so that rapid increase of blood pressure can be prevented. However such mechanism can be disturbed by non-selective β blocker because it blocks the action of β1 and β2 adrenergic receptor.30-34 Therefore epinephrine behaves as a pure agonist of α adrenergic receptor inducing acute hypertensive crisis, followed by reflex bradycardia, and cardiac arrest in the worst case when it is administered with non-selective β blocker.35
Foster and Aston reported case series of drug interaction between epinephrine and non-selective β blocker.35 When 0.5 - 1.0% lidocaine or xylocaine with 1 : 100,000 - 1 : 200,000 epinephrine was subcutaneously injected to patients in medication with propranolol for eyelid-plasty and facial plasty, there was acute elevation of systolic and diastolic blood pressure, and one of the patient experienced cardiac arrest.
MAO inhibitor and tricyclic antidepressant acts on axon terminal and synaptic space where epinephrine is secreted. MAO inhibitor blocks MAO from breaking up transmitter molecules that epinephrine concentration is increased at axon terminal. Tricyclic antidepressant inhibits the reuptake of neurotransmitters from synaptic space to axon terminal, and also increases epinephrine concentration at synaptic space. Therefore, both MAO inhibitor and tricyclic antidepressants induce the effect of overdose administration of epinephrine.32-34,36,37
Boakes et al. conducted clinical study to evaluate drug interaction between epinephrine and tricyclic antidepressant in patients taking imipramine 25 mg t.i.d, and observed significant elevation of blood pressure in experimental group compared to control group.37 In this way, he reported clinical synergistic interaction between the two drugs.
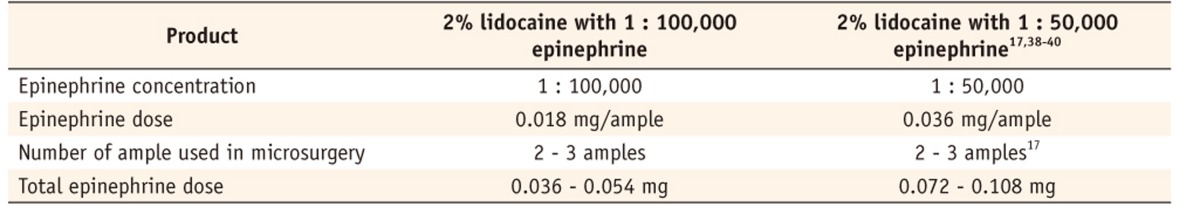
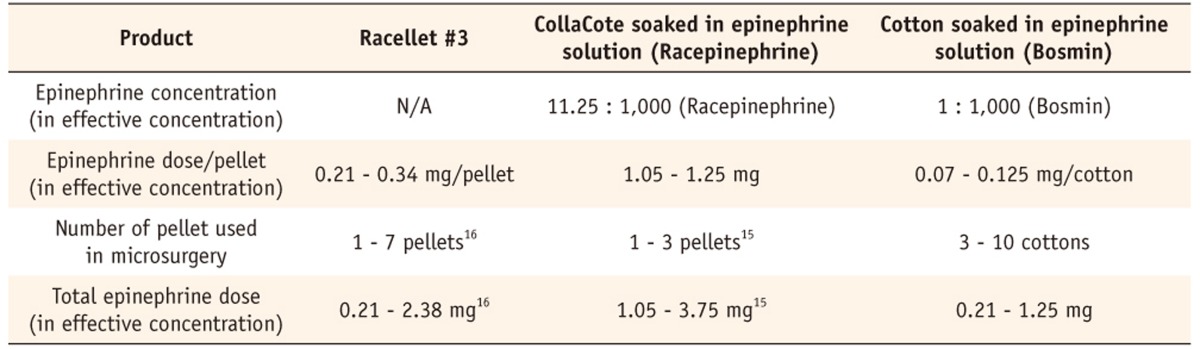
A small amount of epinephrine is routinely injected as a vasoconstrictor with local anesthetic solution for conventional dental surgery and the quantity is about 0.036 - 0.054 mg (Table 1). However, additional amount of epinephrine is applicated in endodontic microsurgery for hemostasis of access bone cavity.17 Epinephrine contained in one Racellet #3 pellet is equivalent to 15.3 amples of 2% lidocaine with 1 : 100,000 epinephrine, and total epinephrine dose used in endodontic microsurgery for hemostasis is reported to 0.21 - 3.75 mg (Table 2).15,16 Therefore, approximately 3.9 - 104 times larger amount of epinephrine is used in endodontic microsurgery compared with other dental surgery or plastic surgery.
In case of systemic emergencies like anaphylaxis or cardiac arrest, generally 0.5 - 1.0 mg of epinephrine is injected intravenously to induce immediate cardiac excitation or assist cardiac defibrillation. Therefore, the amount of epinephrine we are using in endodontic microsurgery might be too large and its safety should be confirmed before application.
Most of epinephrine is applicated through intraosseous route in endodontic microsurgery. Therefore the systemic potency of intraosseous route should be compared with other pathways like subcutaneous, submucous, or intravenous routes to estimate the amount of risk.
Cancellous bone is known to be highly vascularized with much of capillary distribution. Wood et al. observed heart rate after local anesthetic injection, and compared intraosseous injection with infiltration injection in terms of heart rate change.20 Significant increase in heart rate was indentified in intraosseous injection compared with infiltration injection during injection and after 2 minutes.
Hoskins et al. used swine model to compare intraosseous injection with IV injection in terms of inflow capacity to systemic circulation as he measured aortic concentration of epinephrine 480 seconds after injection.21 Intraosseous injection through sternum resulted 86% of epinephrine concentration in relative dose compared with IV injection, and intraosseous injection via tibia showed 65% of epinephrine concentration compared with IV injection. According to this result, he suggested intraosseous injection of epinephrine as a second choice when IV injection is difficult in cardiovascular emergencies.
On the basis of these studies, we can expect that cardiovascular effect of intraosseous route is comparable to intravenous route, and stronger than subcutaneous or submucosal route.
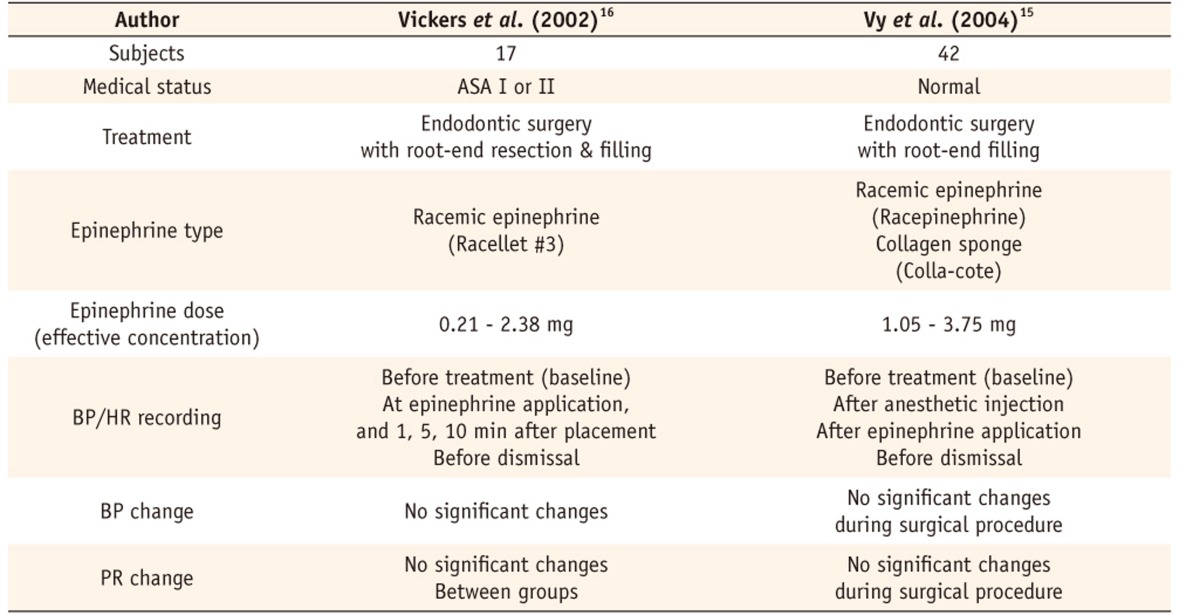
Two clinical studies were found, which examined cardiovascular effects of epinephrine during endodontic surgery (Table 3).15,16
Vickers et al. evaluated 17 ASA I or II patients who underwent endodontic surgery with the use of topical epinephrine for hemostasis.16 Racemic epinephrine pellets (Racellet #3) were applied into bone cavity to achieve hemostasis during surgery, and blood pressure and pulse rate was measured pre- and postoperatively and during the surgery. Results indicated that there was no significant change in blood pressure and pulse rate.
Vy et al. evaluated 42 patients who received topical epinephrine placement during endodontic surgery.15 Racemic epinephrine was delivered with collagen sponge into bony crypt for hemostasis, and blood pressure and pulse rate was measured pre- and postoperatively and during the surgery. Other than slight increase of pulse rate on anesthetic injection, results showed no evident changes in blood pressure or pulse rate during surgical procedure. Vy et al. pointed out that epinephrine is not applied by injection mode, but applied topically. As topically applied epinephrine causes immediate local vasoconstriction of capillaries in bone cavity surface, there is little chance of large amount of epinephrine to be absorbed into the systemic circulation. This can be one of the reasons why there are rare emergency situations in the routine endodontic microsurgery.
These clinical studies indicate that epinephrine can be considered as a stable hemostatic agent if it is applied in controlled volume, and for normal patients without severe systemic complications. Although existing clinical studies are not warning about potential systemic complication of epinephrine use in endodontic microsurgery, they still cannot guarantee that epinephrine can be used safely in all endodontic microsurgery cases. Only 59 patients without significant systemic disease were evaluated, and there is no data for patients with predisposing systemic diseases such as cardiovascular disease.
Many emergency cases during surgery induced by epinephrine administration have been reported in various fields of medical society, and most of them are related with predisposing cardiovascular complications or drug interactions (Table 4).28,29,35,41,42 Therefore epinephrine application should be carefully considered in such cases.
Epinephrine is a dose-sensitive drug and has narrow safety margin.25 It should be noticed that there are always hyper-responders in each drug, and such hypersensitivity reaction can lead to fatal result when it is related to cardiovascular complication like these cases.
Dose control of epinephrine is the first thing to do for risk management. It is recommended to use quantifiable products, and there are commercial products like Racellet pellets (Pascal International, Bellevue, WA, USA). One Racellet #3 pellet contains 0.55 mg of racemic epinephrine (0.275 mg in effective concentration), therefore clinician can easily estimate the whole epinephrine amount administered. To use cotton soaked in epinephrine solution is not an effective way in measuring epinephrine dose, because the solution volume absorbed to the cotton is not uniform, ranging 0.07 - 0.125 mg/pellet.
Excess application should be avoided. As Kim and Rethnam recommended, to use only one epinephrine cotton followed by sterile dry cottons might be an alternative way in case bleeding is not severe.17
Electrocardiogram should be measured during endodontic microsurgery as well as blood pressure and pulse rate, because there is possibility of cardiac arrhythmia and it is impossible to detect it without electrocardiogram. All parameters must be checked in real-time to deal with emergency immediately.
The effect of epinephrine administration during endodontic microsurgery has not been fully investigated. Clinical studies to date do not provide sufficient information about potential systemic complications of epinephrine use in endodontic microsurgery, meanwhile case reports and case series are warning about the risk. Clinicians should be aware of the nature of epinephrine, and should pay attention to its potential risk when treating patient with endodontic microsurgery, especially for medically compromised patients.
Further research is strongly recommended to evaluate the cardiovascular effect of epinephrine application during endodontic microsurgery, and to establish standard guidelines that can guarantee safety of patients with various systemic conditions during endodontic microsurgery.
References
1. Bader JD, Bonito AJ, Shugars DA. A systematic review of cardiovascular effects of epinephrine on hypertensive dental patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:647–653. PMID: 12142870.

2. Silvestre FJ, Salvador-Martínez I, Bautista D, Silvestre-Rangil J. Clinical study of hemodynamic changes during extraction in controlled hypertensive patients. Med Oral Patol Oral Cir Bucal. 2011; 16:e354–e358. PMID: 21196862.

3. Ogunlewe MO, James O, Ajuluchukwu JN, Ladeinde AL, Adeyemo WL, Gbotolorun OM. Evaluation of haemodynamic changes in hypertensive patients during tooth extraction under local anaesthesia. West Indian Med J. 2011; 60:91–95. PMID: 21809720.
4. Conrado VC, de Andrade J, de Angelis GA, de Andrade AC, Timerman L, Andrade MM, Moreira DR, Sousa AG, Sousa JE, Piegas LS. Cardiovascular effects of local anesthesia with vasoconstrictor during dental extraction in coronary patients. Arq Bras Cardiol. 2007; 88:507–513. PMID: 17589623.
5. Meral G, Tasar F, Sayin F, Saysel M, Kir S, Karabulut E. Effects of lidocaine with and without epinephrine on plasma epinephrine and lidocaine concentrations and hemodynamic values during third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:e25–e30. PMID: 16037765.

6. Miura K, Matsumura K, Nakamura Y, Kurokawa H, Kajiyama M, Takata Y. Suppression of cardiac sympathetic nervous system during dental surgery in hypertensive patients. Hypertens Res. 2000; 23:207–212. PMID: 10821128.

7. Blinder D, Manor Y, Shemesh J, Taicher S. Electrocardiographic changes in cardiac patients having dental extractions under a local anesthetic containing a vasopressor. J Oral Maxillofac Surg. 1998; 56:1399–1402. PMID: 9846537.

8. Meechan JG. Plasma potassium changes in hypertensive patients undergoing oral surgery with local anesthetics containing epinephrine. Anesth Prog. 1997; 44:106–109. PMID: 9481971.
9. Blinder D, Shemesh J, Taicher S. Electrocardiographic changes in cardiac patients undergoing dental extractions under local anesthesia. J Oral Maxillofac Surg. 1996; 54:162–165. PMID: 8604063.

10. Abraham-Inpijn L, Borgmeijer-Hoelen A, Gortzak RA. Changes in blood pressure, heart rate, and electrocardiogram during dental treatment with use of local anesthesia. J Am Dent Assoc. 1988; 116:531–536. PMID: 3164019.

11. Meyer FU. Hemodynamic changes of local dental anesthesia in normotensive and hypertensive subjects. Int J Clin Pharmacol Ther Toxicol. 1986; 24:477–481. PMID: 3781681.
12. Vernale CA. Cardiovascular responses to local dental anesthesia with epinephrine in normotensive and hypertensive subjects. Oral Surg Oral Med Oral Pathol. 1960; 13:942–952. PMID: 13841864.

13. Cheraskin E. Use of epinephrine with local anesthesia in hypertensive patients. III. Effect of epinephrine on blood pressure and pulse rate. J Am Dent Assoc. 1958; 57:507–519. PMID: 13575081.

14. Davenport RE, Porcelli RJ, Iacono VJ, Bonura CF, Mallis GI, Baer PN. Effects of anesthetics containing epinephrine on catecholamine levels during periodontal surgery. J Periodontol. 1990; 61:553–558. PMID: 2213464.

15. Vy CH, Baumgartner JC, Marshall JG. Cardiovascular effects and efficacy of a hemostatic agent in periradicular surgery. J Endod. 2004; 30:379–383. PMID: 15167461.

16. Vickers FJ, Baumgartner JC, Marshall G. Hemostatic efficacy and cardiovascular effects of agents used during endodontic surgery. J Endod. 2002; 28:322–323. PMID: 12043873.

17. Kim S, Rethnam S. Hemostasis in endodontic microsurgery. Dent Clin North Am. 1997; 41:499–511. PMID: 9248687.
18. Song M, Shin SJ, Kim E. Outcomes of endodontic micro-resurgery: a prospective clinical study. J Endod. 2011; 37:316–320. PMID: 21329814.

19. Cho YW, Kim E. Is stopping of anticoagulant therapy really required in a minor dental surgery? How about in an endodontic microsurgery? Restor Dent Endod. 2013; 38:113–118. PMID: 24010076.
20. Wood M, Reader A, Nusstein J, Beck M, Padgett D, Weaver J. Comparison of intraosseous and infiltration injections for venous lidocaine blood concentrations and heart rate changes after injection of 2% lidocaine with 1 : 100,000 epinephrine. J Endod. 2005; 31:435–438. PMID: 15917682.
21. Hoskins SL, do Nascimento P Jr, Lima RM, Espana-Tenorio JM, Kramer GC. Pharmacokinetics of intraosseous and central venous drug delivery during cardiopulmonary resuscitation. Resuscitation. 2012; 83:107–112. PMID: 21871857.

22. Kim E, Song JS, Jung IY, Lee SJ, Kim S. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod. 2008; 34:546–551. PMID: 18436032.

23. Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature-part 1: Comparison of traditional rootend surgery and endodontic microsurgery. J Endod. 2010; 36:1757–1765. PMID: 20951283.

24. Song M, Chung W, Lee SJ, Kim E. Long-term outcome of the cases classified as successes based on short-term follow-up in endodontic microsurgery. J Endod. 2012; 38:1192–1196. PMID: 22892734.

25. Katzung B, Masters S, Trevor A. Basic and Clinical Pharmacology. 12th ed. Columbus: McGraw-Hill;2011. p. 129–149.
26. Chu WS, Park SH, Ahn DK, Kim SK. Effect of local anesthesia on pulpal blood flow in mechanically stimulated teeth. J Korean Acad Conserv Dent. 2006; 31:257–262.

27. Lee JS, Kim SK. The influence of epinephrine concentration in local anesthetics on pulpal and gingival blood flows. J Korean Acad Conserv Dent. 2003; 28:475–484.

28. Lee JY, Hong SJ, Chon JY, Kwon SY. Cardiac arrest induced by submucosal injection of epinephrine in a patient with variant angina. Rhinology. 2010; 48:251–253. PMID: 20502771.

29. Kim HH, Park MI, Park SJ, Moon W. Myocardial infarction thought to be provoked by local epinephrine injection during endoscopic submucosal dissection. J Clin Med Res. 2011; 3:143–146. PMID: 21811546.

30. Hersh EV, Giannakopoulos H. Beta-adrenergic blocking agents and dental vasoconstrictors. Dent Clin North Am. 2010; 54:687–696. PMID: 20831932.

31. Sugimura M, Hirota Y, Shibutani T, Niwa H, Hori T, Kim Y, Matsuura H. An echocardiographic study of interactions between pindolol and epinephrine contained in a local anesthetic solution. Anesth Prog. 1995; 42:29–35. PMID: 8934951.
32. Yagiela JA. Adverse drug interactions in dental practice: interactions associated with vasoconstrictors. Part V of a series. J Am Dent Assoc. 1999; 130:701–709. PMID: 10332135.
33. Pallasch TJ. Vasoconstrictors and the heart. J Calif Dent Assoc. 1998; 26:668–673. 676PMID: 9879236.
34. Ferguson-Myrthil N. Vasopressor use in adult patients. Cardiol Rev. 2012; 20:153–158. PMID: 22318007.

35. Foster CA, Aston SJ. Propranolol-epinephrine interaction: a potential disaster. Plast Reconstr Surg. 1983; 72:74–78. PMID: 6867180.
36. Gómez-Moreno G, Guardia J, Cutando A, Calvo-Guirado JL. Pharmacological interactions of vasoconstrictors. Med Oral Patol Oral Cir Bucal. 2009; 14:e20–e27. PMID: 19114951.
37. Boakes AJ, Laurence DR, Teoh PC, Barar FS, Benedikter LT, Prichard BN. Interactions between sympathomimetic amines and antidepressant agents in man. Br Med J. 1973; 1:311–315. PMID: 4685619.

38. Gutmann JL, Frazier LW Jr, Baron B. Plasma catecholamine and haemodynamic responses to surgical endodontic anaesthetic protocols. Int Endod J. 1996; 29:37–42. PMID: 9206410.

39. Buckley JA, Ciancio SG, McMullen JA. Efficacy of epinephrine concentration in local anesthesia during periodontal surgery. J Periodontol. 1984; 55:653–657. PMID: 6594502.

40. Witherspoon DE, Gutmann JL. Haemostasis in periradicular surgery. Int Endod J. 1996; 29:135–149. PMID: 9206418.

41. Ferry DR, Henry RL, Kern MJ. Epinephrine-induced myocardial infarction in a patient with angiographically normal coronary arteries. Am Heart J. 1986; 111:1193–1195. PMID: 2940853.

42. Umino M, Ohwatari T, Shimoyama K, Nagao M. Unexpected atrial fibrillation during tooth extraction in a sedated elderly patient. Anesth Prog. 1994; 41:77–80. PMID: 8934964.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download