Abstract
Purpose
This study was performed to assess the radiologic and clinical results of U-blade Gamma3 nail use for the treatment of trochanteric fractures.
Materials and Methods
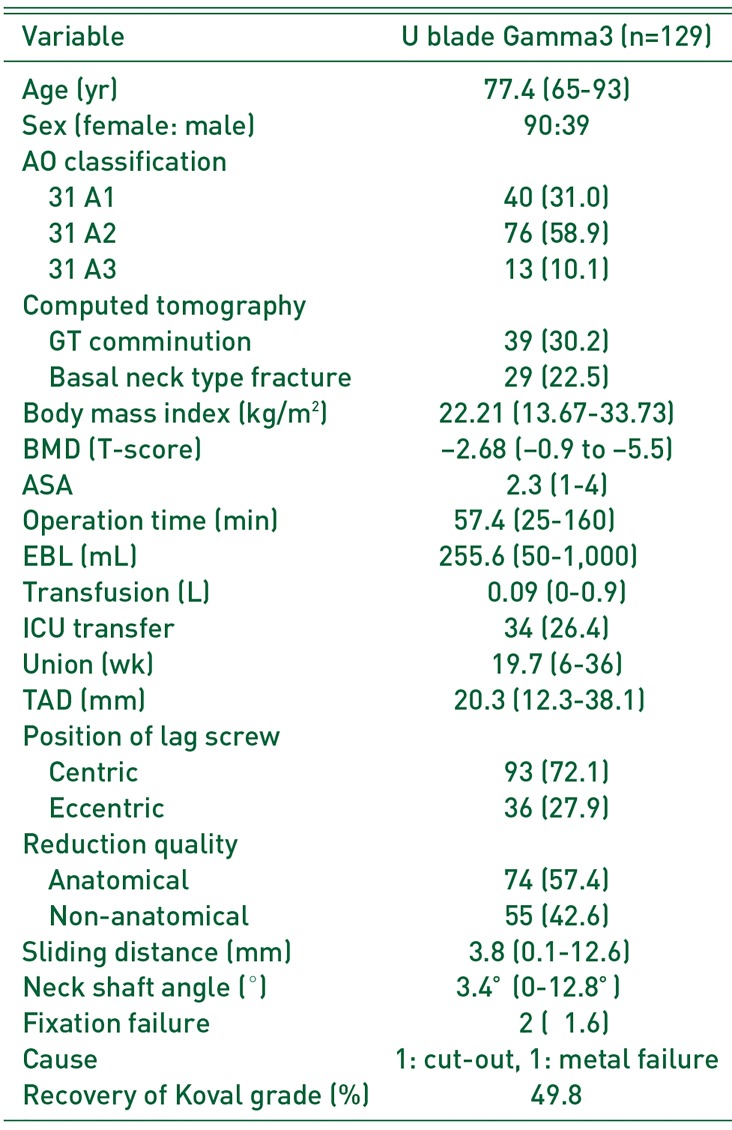
Between September 2015 and May 2018, all patients aged 65 years and older who underwent surgery with U-blade Gamma3 nails were analyzed. A total of 129 patients were selected based on having at least six months of follow-up. Image evaluations included bone quality (T-score), fracture classification on plain radiograph (AO/OTA), computed tomography configuration, union period, position of lag screw, anatomical reduction, tip apex distance (TAD), sliding extent of lag screw, change of neck shaft angle, and complications leading to reoperations were analyzed. Functional outcome were assessed using the Koval grade (ambulatory ability) at the final follow-up.
Results
The mean time to union was 19.7 (range, 6–36) weeks. The screw position was centric (93 cases; 72.1%) and anatomical reduction was achieved in 74 cases (57.4%). The mean TAD was 20.3 (range, 12.3–38.1) mm. The mean sliding length of the lag screws was 3.8 (range, 0.1–12.6) mm. The mean change of neck shaft angle was 3.4° (range, 0–12.8°). Reoperations were required in two cases (1.6%) due to the cutting out of the lag screw (n=1) and metal failure with U-blade bending (n=1). Finally, Koval grades for 49.8% of patients reached preoperative status.
Trochanteric fractures are generally associated with osteoporosis and old age, therefore early treatment, accurate reduction, and internal fixation are crucial to maximize clinical results. In particular, functional recovery through early weight-bearing is an important prognostic indicator of a favorable prognosis. Compression hip screws have less favorable results compared with intramedullary nail fixation and are known to have fewer biomechanical advantages than intramedullary nail, particularly as noted with instability and the risk of severe osteoporotic fractures1). The fourth-generation Gamma nail (Asia-Pacific and Japanese versions, 170 mm) is an innovative design that makes it particularly appropriate for Asian patients who may be smaller in stature. The newest model in the Gamma series (i.e., Gamma3 nail designed with a U-blade lag screw) was designed to provide improved outcomes when treating unstable proximal femur fractures (Fig. 1). Reported herein are a summary of radiological and clinical outcomes for patients treated with Gamma3 nails (Gamm3 U-Blade Lag Screw; Stryker Trauma GmbH, Schoenkirchen, Germany).
This study was approved by local institutional review boards (IRB No. 2018-02-009). The radiological and functional result of the trochanteric fracture patients who underwent internal fixation using the U-Blade Gamma3 lag screw in the orthopedic departments of the three different hospitals between September 2015 and May 2018 were investigated. In total, data from 129 patients (61, 48, and 20 patients at each hospital) were retrospectively collected. The inclusion criteria were: 1) patient greater than 65 years of age, 2) patients had at least six months of follow-up periods, 3) non-pathologic fractures except osteoporosis, 4) low energy fractures (e.g., fall from a standing height), and 5) preinjury independent walker (Koval grade, <6). Patients who were unable to walk on their own prior to the injury (Koval grade, 7) were excluded. The 170 mm nail length was investigated in the current study and most implants were 125° among the three different angles (120°, 125°, 130°); nails of different lengths were excluded to reduce potential bias of lag screw motion (e.g., sliding distance, neck shortening). All operations were conducted by three surgeons who each had five or more years of experience in this field. In all cases, preoperative plain radiographs and three-dimensional (3D) computed tomography (CT) were evaluated to identify: 1) fracture configuration, 2) the presence of greater trochanter (GT) comminution, and 3) basal neck type fractures. Radiological outcomes assessed were: 1) union, 2) lag screw position and change, and 3) basal neck type fracture (Fig. 2). For functional outcome, the recovery rate of functional ability (using Koval grade) was analyzed. The lag screw position in the femoral head was measured using the tip apex distance (TAD) and described as centric and eccentric. Centric position was defined as a lag screw that was simultaneously positioned in the center in the anteroposterior and lateral views. TAD value, position, and reduction quality were evaluated from the anteroposterior and lateral images taken immediately after the surgery. The sliding distance and neck shaft angle, which can represent shortening and varus changes of the fracture site, were calculated as a difference between the initial and final plain radiographs. All parameters which were obtained in the plain radiographs were adjusted by the calibration of magnification of real size and angle of the inserted implants. For fracture union, a clinical union was determined to be achieved when the pain scale improved during the follow-up period and the absence of pain or tenderness during weight-bearing. Radiological union was determined to be achieved when the fracture line was lost and three or more external or internal calluses were formed in the anteroposterior and lateral radiological images taken during the follow-up period2). For functional outcome, ability status was evaluated using the Koval grade34) (Table 1). The preinjury walking ability before surgery was compared to the postinjury walking ability at the final visit. The recovery rates were calculated.
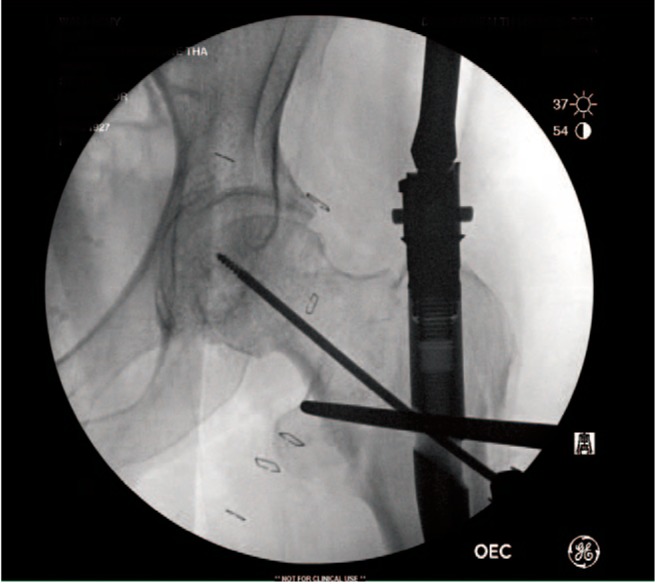
Operations were carried out in a general manner. When the manual reduction was unsatisfactory, a long Kelly, bone hook or Hohmann retractor was used to compress the lateral cortex or the anterior cortex or pulling the medial cortex for the reduction (Fig. 3). No invasive reductions were required. Manual reduction was used to maintain continuity of the medial cortex and the anterior cortex. When anatomical reduction was not maintained, positive medial cortex5) and valgus alignment in anteroposterior fluoroscopic and posteriorly angulation than anterior angulation in lateral C-arm were accepted. When the fracture gap or step displacement remained, or when the medial cortex gap was expanded during the insertion of the lag screw, the lag screw driver thumbwheel was gently tightened to compress the gap, and consequently, apposition was achieved. After the surgery, when the subjects could already bear the pain in a sitting position, they were asked to try to stand using a tilt table mostly one to three days after the surgery. Walking was allowed when the pain became tolerable. Various weight-bearing training exercises were accomplished according to the subject's pain level and fracture type. Follow-up occurred at 1, 3, 6, and 12 months postoperatively and yearly thereafter.
The mean follow-up period was 12.8 months (range, 6–34 months). Of the 129 patients included, 90 (69.8%) were females and their mean age was 77.4 years (range, 65–93 years). The mean time lapse between admission and surgery was 2.9 days (range, 0–32 days); however, 40 patients (31.0%) underwent operations within one day. Fractures were classified according to the AO/OTA fracture classification scale revealing the following ratio: A1 (n=40), A2 (n=76), and A3 (n=13). A stable fracture (A11–21) was observed in 59 cases (45.7%), and an unstable fracture (A22–33) in 70 cases (54.3%). Upon CT evaluation, GT comminution was noted in 39 cases (30.2%) and basal neck type fractures were noted in 29 cases (22.5%). For osteoporosis assessments, quantitative CT and dual-energy X-ray absorptiometry (DEXA) were used. The mean body mass index was 22.21 kg/m2 (range, 13.67–33.73 kg/m2). The mean T-score was −2.68 (range, −0.9 to −5.5). The pre-operative American Society of Anesthesiologists (ASA) status was 2.3 (range, 1–4). The mean operative time from the skin incision to the nail insertion and the skin suture was 57.4 minutes (range, 25–160 minutes); the mean estimated blood loss was 255.6 mL (range, 50–1,000 mL), and the mean blood transfusion amount was 0.09 L (range, 0–0.94 L). In total, 95 patients were moved to general wards after their surgeries and 34 (26.4%) patients were transferred to the surgical intensive care unit. All of the ASA 3 and 4 patients and some of ASA 2 patients were transferred to ICU. No subjects died during the hospital course (or admission periods). Bone union was achieved in 127 subjects (98.4%). One patient experienced a delay in union; however, healing was accomplished without any additional medication or procedures. The mean fracture union period was 19.7 weeks (range, 6–36 weeks). The mean TAD was 20.3 mm (range, 12.3–38.1 mm) and 64 (49.6%) had TAD of 10 to 20 mm. The screws were coded as being in the centric position in 93 cases (72.1%); the remaining 36 were in eccentric positions. Anatomical reductions were achieved in 74 (57.4%) cases; the remaining achieved non-anatomical reductions. The mean sliding distance was 3.8 mm (range, 0.1–12.6 mm), and only six (4.7%) patients were over 10 mm; there were no additional operations required due to over sliding. The mean change of neck shaft angle was 3.4°(range, 0–12.8°). All subjects have varus changes. A significant change was defined as a change of 10°or more, but no complications (significant shortening, nail breakage, non-union) were observed, so even a 10°or greater varus deformity was not included as a complication. Resurgery was required in two subjects (1.6%). One presented with cut out of the femoral head at three months after operation (Fig. 4) and the other was a metal failure due to secondary injury at one month after surgery (Fig. 5); both were converted to hemiarthroplasties. According to the pre-operative fracture classification, there was one case of a stable fracture (A11), basal neck fracture type with T score of −3.5; and the other one case was unstable (A32) with T score of −1.9. The functional ability for walking was compared to the preoperative status to the status of final visits. The mean Koval grade at final visits was 2.7 (range, 1–7). The overall recovery rate of ambulatory status was 49.8% (Table 2).
The initial Gamma nail model, a screw-type intramedullary nail, has a minimal bending stress applied to the internal fixator, allowing for rigid stability without anatomical reduction of the posteromedial cortex, and subsequent early weight-bearing67). Although the Gamma nail has been used for almost 30 years and has thus garnered accumulated clinical experience, its initial model is associated with complications such as femoral shaft fracture, cut out of the lag screw from the femoral head, and femoral pain189). Kim et al.10) reported that the conventional Gamma3 nail was not significantly better at treating intertrochanteric fractures than other available options (e.g., DLT [Dyna Locking Trochanteric Nail] or PFNA [Proximal Femoral Nail Antirotation]). The recent U-blade Gamma3 nail is one of the most innovative nails among the nail systems, including the Asia-Pacific-type nails which were introduced in 2010 in South Korea. The U-blade Gamma3 nail was introduced in 2015, and was designed to prevent rotation; however, no clinical trials describing the risk-benefit profile have been published11). While the current study is not a comparison study, the clinical outcomes appear favorable.
Various implants have been designed to improve rotational stability in unstable femur fractures1213). For the effort of reducing the implant related complications such as lag screw cutout, cut thorough and pull out, many different companies have developed novel lag screw designs. The U-blade Gamma3 nail is the most evolved option and has the most clinical experience. Although though there is no objective comparative data in this study to support its superiority to other options, only two cases (1.6%) of fixation failure suggest that the new U-blade Gamma3 design is associated with favorable results and that it may successfully replace the previous Gamma3 nail design.
In particular, the femoral shaft fracture is the most serious peri- and post-operative complication associated with wrong procedures and poorly designed nails14). The incidence of post-operative shaft fractures has been reported to range from 0% to 12%9151617); however, in this study, no shaft fractures developed during or after the surgery. In the case of the distal locking screw, the short metal nail caused less discrepancy with the jig, and wrong or difficult insertion of the distal locking screw did not occur. Accordingly, complications such as stress concentration fractures around the tips of the nails or the interlocking screws can be avoided. Compared with the typical 240-, 200-, and 180-mm nails, the surgical procedure is more convenient and has fewer complications. In a study by Rosenblum et al.7), a decrease in the stability of the fracture site reduces the calcar femoral load and thus increases the concentration of the distal portion of Gamma nail. Furthermore, the excessive reaming required for larger nails weakens the femoral shaft, which is vulnerable to fracture during the operation or postoperative period. According to Halder6), when reaming is excessively conducted for Gamma nail insertion, stress shielding occurs to cause a fatigue fracture in distal portion of nail, and it takes long period for surgeons to be skillful with this method. The Gamma nail is prone to be implant-related femur fractures18). In our study, there were no reports of peri-implant fracture or thigh pain. The short length (170 mm) of the Gamma3 nail is advantageous relative to this potential complication.
In a biomechanical study, Wang et al.19) demonstrated the superiority of one lag screw design over the two lag screws design regarding cut out and antirotation. Recently, Chinzei et al.13) reported that the gliding nail, with its specific non cylindric blade design, provides the most favorable antirotation results compared to cylindric helical blade or lag screws. According to the clinical experience of the authors, it has been a recognized disadvantage of the U-blade Gamma3. This system may be more time consuming due to the management of additional U-blade. The metal failure related to the U-blade was reported as a case report by Choi et al20). In this case, the reduction quality was poor, the TAD was outside of the normal range, and the lag screw was too low in the anteroposterior view of plain radiograph and anterior in the lateral plain radiograph, so these factors may contribute the lag screw failure. Unlike the typical metal nails, the modified nails were made of titanium and were 170 mm long (down from 180 mm), and the distal diameter decreased from 11 to 10 mm. As a result, a less invasive surgical procedure could be achieved, the levels of the post-operative thigh pain and the stress riser fracture, which were caused by the abutment between the metal nails and the femoral internal bone, decreased21). However, when used for fractures extended to the subtrochanteric area, it may be unstable after the surgery due to the shortened length of 170 mm, due to which a refracture may develop. In these cases, long Gamma nails must be used, another potential disadvantage of this system.
We acknowledge major limitations in this study. First, the number of patients was limited and it was difficult to follow-up because the patients were geriatric. If a patient died or could not be followed properly, treatment outcomes could not be fully evaluated. Therefore, the results of this analysis might not be sufficiently suitable for the interpretation of clinical results. Second, surgeons were in different hospitals, so any bias may remain and interfere with an accurate interpretation of results. Lastly, the data from the plain radiographs (e.g., neck shaft angle, sliding distance, TAD, reduction quality, or screw position) are continuous variables which may be associated with interobserver variability.
The U-blade Gamma3 nail can be used to treat proximal femoral trochanteric fracture with favorable results. When using this nail, accurate reduction, an appropriate lag screw length, and accurate positioning of the lag screw in the femoral head can be achieved. A 1.6% cut out rate is very encouraging despite the metal failure by secondary trauma. Analysis of additional cases with longer follow-up will help provide a more comprehensive evaluation of this newly designed U-blade Gamma3 nail.
References
1. Stapert JW, Geesing CL, Jacobs PB, de Wit RJ, Vierhout PA. First experience and complications with the long Gamma nail. J Trauma. 1993; 34:394–400. PMID: 8483181.

2. Corrales LA, Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008; 90:1862–1868. PMID: 18762645.

3. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995; (310):150–159.
4. Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD. Functional outcome after hip fracture. Effect of general versus regional anesthesia. Clin Orthop Relat Res. 1998; (348):37–41. PMID: 9553531.
5. Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015; 135:811–818. PMID: 25840887.

6. Halder SC. The Gamma nail for peritrochanteric fractures. J Bone Joint Surg Br. 1992; 74:340–344. PMID: 1587873.

7. Rosenblum SF, Zuckerman JD, Kummer FJ, Tam BS. A biomechanical evaluation of the Gamma nail. J Bone Joint Surg Br. 1992; 74:352–357. PMID: 1587875.

8. Williams WW, Parker BC. Complications associated with the use of the gamma nail. Injury. 1992; 23:291–292. PMID: 1644453.

9. Hesse B, Gachter A. Complications following the treatment of trochanteric fractures with the gamma nail. Arch Orthop Trauma Surg. 2004; 124:692–698. PMID: 15517321.

10. Kim SS, Lee KY, Kim CH, et al. Comparison of the Dyna locking trochanteric nail, proximal femoral nail antirotation and gamma 3 nail in treatment of intertrochanteric fracture of the femur. Hip Pelvis. 2013; 25:211–219.

11. Lang NW, Arthold C, Joestl J, et al. Does an additional antirotation U-Blade (RC) lag screw improve treatment of AO/OTA 31 A1-3 fractures with gamma 3 nail? Injury. 2016; 47:2733–2738. PMID: 27832831.

12. Mereddy P, Kamath S, Ramakrishnan M, Malik H, Donnachie N. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury. 2009; 40:428–432. PMID: 19230885.

13. Chinzei N, Hiranaka T, Niikura T, et al. Comparison of the sliding and femoral head rotation among three different femoral head fixation devices for trochanteric fractures. Clin Orthop Surg. 2015; 7:291–297. PMID: 26330949.

14. Chevalley F, Gamba D. Gamma nailing of pertrochanteric and subtrochanteric fractures: clinical results of a series of 63 consecutive cases. J Orthop Trauma. 1997; 11:412–415. PMID: 9314147.

15. Goldhagen PR, O'Connor DR, Schwarze D, Schwartz E. A prospective comparative study of the compression hip screw and the gamma nail. J Orthop Trauma. 1994; 8:367–372. PMID: 7996318.

16. Friedl W, Colombo-Benkmann M, Dockter S, Machens HG, Mieck U. [Gamma nail osteosynthesis of per- and subtrochanteric femoral fractures. 4 years experiences and their consequences for further implant development]. Chirurg. 1994; 65:953–963. German. PMID: 7821076.
17. Forthomme JP, Costenoble V, Soete P, Docquier J. [Treatment of trochanteric fractures of the femur using the gamma nail (apropos of a series of 92 cases)]. Acta Orthop Belg. 1993; 59:22–29. French. PMID: 8484318.
18. Robinson CM, Adams CI, Craig M, Doward W, Clarke MC, Auld J. Implant-related fractures of the femur following hip fracture surgery. J Bone Joint Surg Am. 2002; 84:1116–1122. PMID: 12107309.

19. Wang CJ, Brown CJ, Yettram AL, Procter P. Intramedullary femoral nails: one or two lag screws? A preliminary study. Med Eng Phys. 2000; 22:613–624. PMID: 11259930.

20. Choi K, Kim Y, Zhou S, Hwang J. Failure of a rotation control Gamma 3 lag screw used to treat a trochanteric fracture. Hip Pelvis. 2018; 30:129–133. PMID: 29896464.

21. Loch DA, Kyle RF, Bechtold JE, Kane M, Anderson K, Sherman RE. Forces required to initiate sliding in second-generation intramedullary nails. J Bone Joint Surg Am. 1998; 80:1626–1631. PMID: 9840631.

Fig. 2
Basal neck type fracture was defined as a fracture with the main fracture line between the base of the neck and the upper margin of the medial lesser trochanter, between the base of the neck base and one cm lateral to greater trochanter tip on three-dimensional computed tomography (CT) image. The blue zone is the trochanteric fracture zone. The red lines are suggestive of a basal neck fracture type upon CT scan.
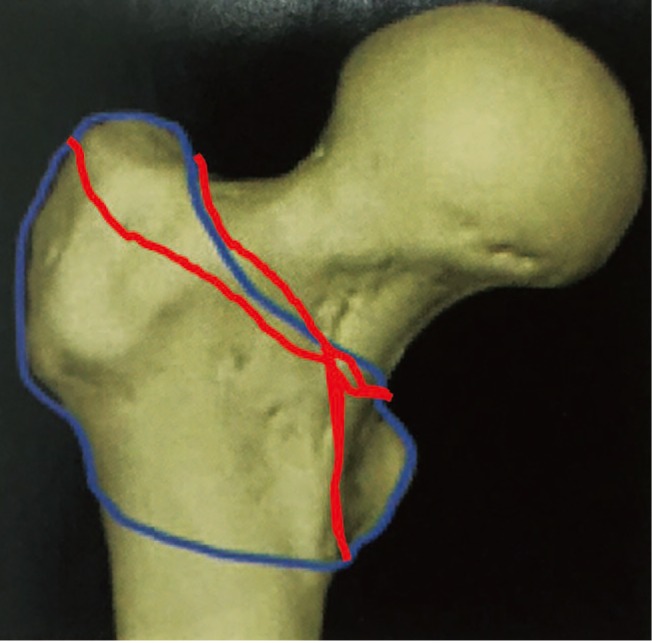
Fig. 4
(A) An 83-year-old woman suffered from a fall from height at home; the fracture type was reverse oblique (A32). (B) The fragment was reduced using a U-blade Gamma3 nail. (C) The lag screw was cut out of the head three months postoperatively. (D) The reoperation was converted to hemiarthroplasty.
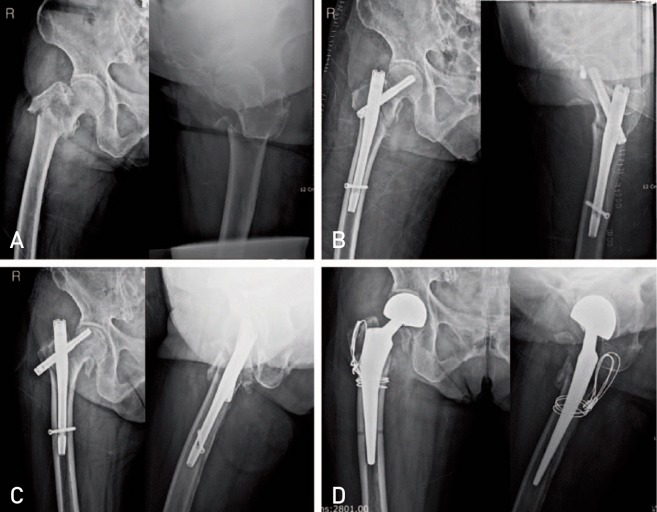
Fig. 5
(A) A 93-year-old woman presented with a stable fracture (A11). (B) The three dimensional computed tomography scan revealed basilar neck fracture type. (C) The reduction was controlled using a U-blade Gamma3 nail (170 mm, 125°). (D) The lag screw was cut out and failure of U-blade occurred at one month postoperatively.
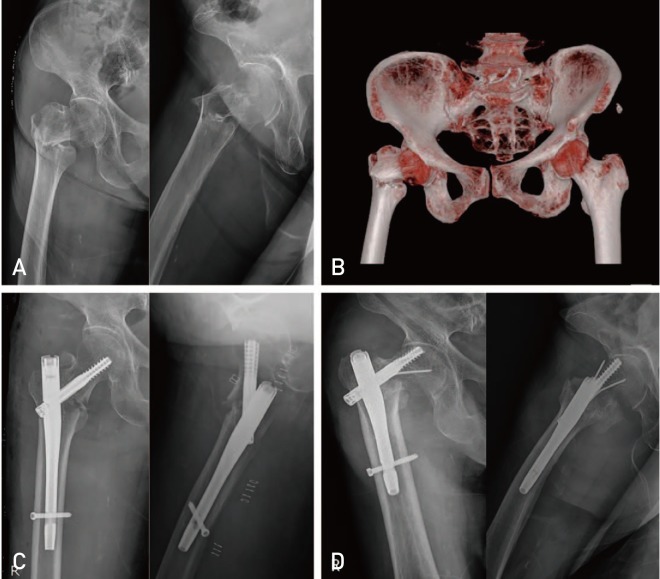
Table 1
Categories of Ambulatory Ability
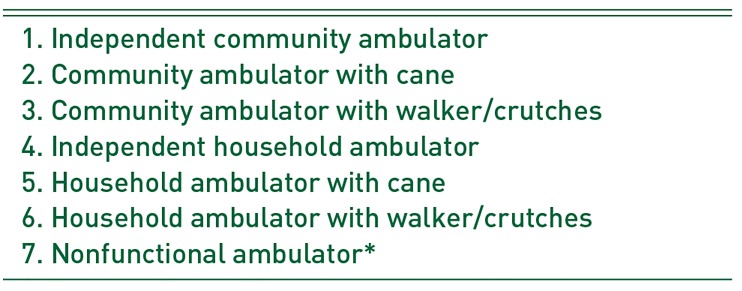
Table 2
Clinical Outcomes Associated with Use of U-blade Gamma3 Nails




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download