Abstract
Pseudotumors are not uncommon complications after total hip arthroplasty (THA) and may occur due to differences in bearing surfaces of the head and the liner ranging from soft to hard articulation. The most common causes of pseudotumors are foreign-body reaction, hypersensitivity and wear debris. The spectrum of pseudotumor presentation following THA varies greatly-from completely asymptomatic to clear implant failure. We report a case of pseudo-tumor formation with acetabular cup aseptic loosening after revision ceramic-on-metal hip arthroplasty. The patient described herein underwent pseudotumor excision and re-revision complex arthroplasty using a trabecular metal shell and buttress with ceramic-on-polyethylene THA. Surgeons should be aware of the possibility of a pseudotumor when dealing with revisions to help prevent rapid progression of cup loosening and implant failure, and should intervene early to avoid complex arthroplasty procedures.
Pseudotumors are not a single entity, but rather a spectrum of abnormal periprosthetic soft tissue reactions causing a granulomatous mass or destructive cystic lesion1). These complications may developed in following surgeries involving metal-on-polyethylene (MoP) total hip arthroplasty (THA) due to polyethylene debris2) and metal-on metal (MoM) THA due to metal debris34). These lesions are non-neoplastic and believed to worsen progressively, resulting in extensive bone and soft tissue destruction1). Pseudotumors are increasingly associated with THA; recent studies report incidences ranging from 0.27%5) to 5%6). To overcome the adverse effect of metal ion release in MoM arthroplasties, other hard bearings with improved quality were introduced (e.g., ceramic-on-ceramic [CoC] and ceramic-on-metal [CoM]) couples which are associated with minimal bearing surface wear. Importantly, there are limited clinical data relating to the use of CoM, with short duration of follow-up and high variation in the wear performance789). Here, we report a case of pseudotumor formation one year after CoM revision THA.
The patient's informed consent was taken for the purpose of publication of the case along with institutional review board clearance.
A 50-year-old female department store salesperson, who presented with idiopathic bilateral avascular necrosis of the femoral head underwent primary left-hip THA in 2003 at an outside institution 3 years prior to evaluation at our hospital. This patient presented with worsening right hip pain for the previous 4 months. Radiographs demonstrated secondary osteoarthritis of the right hip joint for which CoP THA was performed. On the left side, the patient had an apparent well-functioning THA (i.e., without evidence of loosening). A review of operative records identified the left-side THA components as cementless MoP. The surgical incision at the left hip was well healed with no evidence of any infection.
In 2011, the patient started to complain of gradual onset of pain in the left hip. Radiographs and computed tomography (CT) scans demonstrated polyethylene wear with aseptic loosening of both acetabular and femoral components. This patient underwent revision THA with cementless CoM of her left hip in 2011 using: i) a 54 mm pinnacle acetabular shell, ii) a cobalt chromium (CoCr) metal liner, iii) a 36 mm Biolox delta ceramic head, and iv) a S-ROM titanium alloy femoral stem with titanium sintered proximal sleeve (Depuy, Johnson and Johnson Corp., Warsaw, IN, USA). On the acetabular side, an allo chip bone graft was used for osteolytic lesions, and encirclage wiring was done for greater trochanter. Intraoperative findings were loosening of the femoral stem and acetabular cup along with mild metallosis of the acetabulum and the femoral side. The postoperative period was uneventful with substantial functional improvement. As estimated from plain radiographs, acetabular cup inclination and anteversion angles were 45° and 20°, respectively. Femoral anteversion was 15° with normal stem alignment. At 6-week follow-up, the patient was able to begin partial weight-bear, increasing to full weight-bearing with an assistive device and active abduction over a 6-week period.
After 1 year of follow-up in 2012, the patient complained of mild discomfort in the left inguinal region. On examination, a soft non-tender swelling (roughly 2×3 cm), with no signs of inflammation, was noted in the left inguinal region. Radiographs revealed normal alignment and position of the hip prosthesis with no signs of loosening (Fig. 1A). Ultrasonography of the swelling suggested a cystic lesion in the iliopsoas area (3.76×3.12×2.95 cm; Fig. 1B) and was suspected to be iliopsoas bursitis. Serum inflammatory markers and complete blood counts were within normal limits. Clinical examination revealed painless normal range of motion of the left hip. The patient was kept under observation after refusal for ultrasound-guided aspiration.
After one month, the patient complained of pain in the left hip joint region and started to limp in a few days. This patient also experienced an increase in the size of the previously noted swelling. Follow-up radiographs revealed signs of superior and lateral migration of the acetabular cup, increased inclination angle with evidence of loosening of cup but a well-fixed femoral stem (Fig. 1A). CT scan revealed a well-circumscribed lesion around the left hip with extension into the iliopsoas region (Fig. 2). CT scans revealing lysis of the left hip with normal right hip joint. CT scans also revealed the superior segmental defect in the acetabulum along with loosening of the acetabular cup. A positive radioisotope bone scan indicated acetabular loosening. The patient's serum C-reactive protein value was 0.6 mg/dL (normal) and erythrocyte sedimentation rate was 28 mm/hour (slightly elevated; normal, 2–20 mm/hour). Her complete blood cell count was normal. Serum cobalt and chromium levels were significantly elevated (serum Co=2.4µg/L [reference, <0.9µg/L], serum cr=22.5µg/L [reference, <0.4µg/L]).
Given the clinical and imaging findings, combined with a history of CoM THA, her care team deemed that this patient's symptoms were likely due to aseptic loosening of the acetabular cup with local soft tissue response due to elevated serum metal ions. Surgical exploration with revision THA for loosened implant was discussed with the patient and she underwent a revision THA using a posterior approach. The pseudotumor and surrounding inflamed synovial sac (Fig. 3A) was excised. The cystic soft tissue swelling extended into the hip joint and was stained black with features suggestive of metallosis (Fig. 3B). The patient's hip was dislocated and the loosened acetabular cup along with CoCr liner was removed. There was corrosive wear of the metal liner with a large “black stripe” across the top of the retrieved ceramic femoral head (Fig. 4). The proximal femoral sleeve and the femoral taper showed no corrosion or wear and were well-fixed with no signs of loosening.
The intraoperative frozen section of the excised mass revealed less than 5 polymorphonuclear leukocytes per high-power field in all the three specimens. Intraoperative dark gray colored fluid analysis was done, revealing 58% polymorphonuclear cells, 39% lymphocytes and 3% mononuclear cells. After aggressive debridement of the metallic and necrotic tissue and thorough lavage, the acetabular cavitary defects were filled with mixed autogenous bone graft and allograft bone chips. On the acetabular side, the patient was revised with a 52 mm trabecular metal shell with metal buttress which can be seen on final post-operative X–ray (Fig. 5) to address the superior bone defect (Zimmer, Warsaw, IN, USA). A highly cross-linked polyethylene liner was applied with 32 mm Biolox delta ceramic femoral head (Depuy, Johnson and Johnson Corp.).
Operative cultures of soft tissues and fluid were both negative for infection. Histopathology was consistent with metallosis. For each tissue fragment, sections were routinely stained with hematoxylin and eosin and were examined with light microscopy. On microscopic examination, the inner surface was covered with the eosinophilic fibrinoid material with local fibrotic tissue. The histopathology analysis supported morphology consistent with metallosis as an inflammatory response to metal particles. It revealed abundant lymphocytes, histiocytes, occasional plasma cells, foreign body type giant cells and black metal particles (Fig. 6).
After 6 weeks of partial weight bearing, the patient was mobilized to full weight-bearing over a period of 6 weeks. At 6 months, a repeat serum metal ion analysis revealed a decrease in cobalt and chromium ions levels with their values being 1.3 and 2.54 µg/L, respectively. The most recent serum cobalt and chromium ions values were 0.66 and 0.42 µg/L, respectively. Functionally, the patient continued to improve and had a Harris hip score of 87 at the latest follow-up which was significantly higher than the pre-operative score of 58.
The use of a MoM bearing is associated with elevated levels of serum metal ions3) with local effects (metallosis and local soft tissue reaction)6). The use of MoM articulations have decreased, while other hard bearings (e.g., CoC and CoM) have been increasingly used. Although CoC bearings are associated with low wear rates, breakage and squeaking are still a concern. In vitro studies have shown reduced wear rate in CoM bearing surface7). At the same time, there is a difference in the literature between wear and metal ion release in CoM with limited clinical data89). Few reports reveal a relationship between head-neck, modular neck and stem-sleeve corrosion with the increased incidence of metal hypersensitivity reactions10). Patient-related factors (e.g., sex [female]11); surgeon-related factors [e.g., suboptimal component positioning12)]) are more often involved in the formation of a pseudotumor. However, all the three hard bearings (i.e., CoC, CoM, MoM) are associated with increased wear with edge loading; CoM bearings are associated with a lower wear rate compared with MoM13).
Two case reports describe pseudotumor formation around the CoM bearing after primary arthroplasty with abnormal acetabular cup positioning; in these cases, the pseudotumors resulted from cup malposition14). To the best of our knowledge, this case report is the first to describe pseudotumor formation with rapid loosening, and large pelvic osteolysis after a well-aligned and positioned revision CoM THA managed with complex re-revision arthroplasty. No definitive reason for pseudtumor was ascertained; however, we believe that impingement, third-body or backside wear, or spinopelvic problem might be at least partially responsible. The initial presentation of symptoms in our case occurred one year after the revision surgery-a short duration when compared with soft tissue reactions involving a MoP bearing (range from 3 to 26 years15)).
In the management of a pseudotumour, non-metal bearing is indicated during revision surgery5), and we revised our case with ceramic on polyethylene. However, since a modular titanium alloy stem with the sleeve, porous trabecular metal shell and a metal buttress was still present, the patient requires close follow-up with regular serum metal ion analysis.
Even mild signs and symptoms of soft tissue reaction should be aggressively investigated for metallosis, even in the absence of any radiographic loosening. Treating physicians should be aware of this condition so that prompt diagnosis and treatment can occur. Patients with index revision surgery due to aseptic loosening may require subsequent re-revision due to loosening. Loosening in such cases will increase edge loading, hence more severe metallosis and rapid loosening requiring a complex arthroplasty procedure.
Figures and Tables
Fig. 1
(A, B) Anteroposterior radiograph of left hip. (A) One year after revision cementless ceramic-on-metal hip arthroplasty with well-aligned and fixed implants. (B) One month after the initial presentation of mild discomfort, radiograph revealed acetabular cup superior and lateral migration with a well-fixed femoral stem. (C) Ultrasonography of left hip revealing a cystic lesion in the iliopsoas area (3.76×3.12×2.95 cm).

Fig. 2
(A–C) Computed tomography scans of both hips revealing a space-occupying lesion in the iliopsoas region which is in communication with the left hip joint (arrow).

Fig. 3
(A, B) Intraoperative photograph demonstrating ceramic head and metal liner with metal staining and metallosis of soft tissue. (C) Photograph demonstrating cup and metal liner with metal staining and metallosis of soft tissue.

Fig. 5
Postoperative anteroposterior radiograph after second-stage revision with trabecular metal cup and buttress with head and liner exchanged.

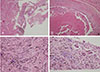
Fig. 6
Histological sections (H&E stain). (A) Chronic inflammation indicated by the presence of black pigment and pseudotumor perivascular lymphocytes (×40). (B) Necrotic debris with fibrosis, fibrin material and lymphocytes (×100). (C) Photomicrograph demonstrating histiocyte infiltration with gray and black metal particles in the tissue surrounding the granuloma (×400). (D) High-power magnification demonstrating the presence of histiocytes and foreign body type giant cells containing black metallic particles (×400).
References
1. Daniel J, Holland J, Quigley L, Sprague S, Bhandari M. Pseudotumors associated with total hip arthroplasty. J Bone Joint Surg Am. 2012; 94:86–93.

2. Griffiths HJ, Burke J, Bonfiglio TA. Granulomatous pseudotumors in total joint replacement. Skeletal Radiol. 1987; 16:146–152.

3. Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008; 90:847–851.

4. Madan S, Jowett RL, Goodwin MI. Recurrent intrapelvic cyst complicating metal-on-metal cemented total hip arthroplasty. Arch Orthop Trauma Surg. 2000; 120:508–510.

5. Campbell P, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J Arthroplasty. 2008; 23:1080–1085.

6. Kwon YM, Ostlere SJ, McLardy-Smith P, Athanasou NA, Gill HS, Murray DW. “Asymptomatic” pseudotumors after metal-on-metal hip resurfacing arthroplasty: prevalence and metal ion study. J Arthroplasty. 2011; 26:511–518.

7. Williams S, Schepers A, Isaac G, et al. The 2007 Otto Aufranc Award. Ceramic-on-metal hip arthroplasties: a comparative in vitro and in vivo study. Clin Orthop Relat Res. 2007; 465:23–32.
8. Isaac GH, Brockett C, Breckon A, et al. Ceramic-on-metal bearings in total hip replacement: whole blood metal ion levels and analysis of retrieved components. J Bone Joint Surg Br. 2009; 91:1134–1141.
9. Reinders J, Sonntag R, Heisel C, Reiner T, Vot L, Kretzer JP. Wear performance of ceramic-on-metal hip bearings. PLoS One. 2013; 8:e73252.

10. Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2012; 41:422–426.
11. Mont MA, Schmalzried TP. Modern metal-on-metal hip resurfacing: important observations from the first ten years. J Bone Joint Surg Am. 2008; 90:Suppl 3. 3–11.

12. Harper GD, Bull T, Cobb AG, Bentley G. Failure of the Ring polyethylene uncemented acetabular cup. J Bone Joint Surg Br. 1995; 77:557–561.

13. Williams S, Isaac G, Porter N, Fisher J, Older J. Long-term radiographic assessment of cemented polyethylene acetabular cups. Clin Orthop Relat Res. 2008; 466:366–372.

14. Deshmukh AJ, Rathod PA, Rodgers WH, Rodriguez JA. Early failure of a ceramic-on-metal total hip arthroplasty: a case report. JBJS Case Connect. 2012; 2:e25.
15. Carli A, Reuven A, Zukor DJ, Antoniou J. Adverse soft-tissue reactions around non-metal-on-metal total hip arthroplasty - a systematic review of the literature. Bull NYU Hosp Jt Dis. 2011; 69:Suppl 1. S47–S51.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download