Abstract
Purpose
This study was performed to assess the clinical and radiological outcomes following one-stage hip reconstruction, consisting of open reduction femoral shortening and pelvic osteotomy, for neglected developmental dislocation of the hip (DDH).
Materials and Methods
This is a retrospective analysis of 77 hips in 65 patients (46 females and 19 males; 12 had bilateral dislocations), operated at a Ghurki Trust Teaching Hospital in Pakistan between 2013 and 2015. The average age at surgery was 11.02±3.43 years. According to the Tönnis classification, there were 10, 14, 22, and 31 patients in grades 1, 2, 3, and 4, respectively. The pelvic procedure utilized in this study was triple osteotomy (47 hips) followed by double and Salter osteotomy (18 and 12 hips, respectively). Postoperative evaluations were conducted using the modified MacKay's scoring system (functional outcomes) and Severin's scoring method (radiological assessment).
Results
Postoperatively, there were 38 (49.4%), 19 (24.7%), 14 (18.2%), and 6 (7.8%) hips in Severin grade I, II, III and IV, respectively. According to the modified McKay criteria, there were 22 hips (28.6%) in excellent condition, 44 (57.1%) in good condition, 9 (11.7%) in fair condition and 2 (2.6%) in poor condition. Both patients with poor outcomes had an unstable, painful hip with evidence of avascular necrosis of the femoral head.
Late-presenting developmental dislocation of the hip (DDH) is still a common problem in developing countries and among low socioeconomic groups. Left untreated, these dysplastic changes initially lead to abnormal gait followed by osteoarthritis in early adulthood1). The principal problems in the management of late-diagnosed dislocations are a high femoral head, adaptive shortening of the extra-articular soft tissues and a dysplastic acetabulum2).
The principles of treating a dislocated hip joint in an older child are quite different from that of a neonate. Reduction of DDH is challenging and complications are frequent. A good result after open reduction for DDH depends on the remodeling of the acetabulum in response to the reduced femoral head. As the remodeling potential diminishes with age, chances of successful outcomes decrease significantly and subsequently may cause more disability than the dislocated hip, particularly in children with bilateral DDH3). Some authors suggest that reduction of the hip after the age of 10 years is not advisable and that the condition should be treated with skilled neglect until the hip is painful and the patient old enough to undergo total hip replacement4). After surveying the relevant literature, a handful of studies supporting surgical treatment were identified3456).
A combination of open reduction with femoral shortening is popular to correct the deformities in one stage. Femoral shortening helps prevent excessive pressure on the femoral head when it is relocated in the acetabulum, which may predispose the affected to avascular necrosis (AVN). Pelvic osteotomy is often required owing to dysplastic and shallow acetabulum27). We report a retrospective analysis designed to evaluate the radiographic and functional results of a one-stage triple operative procedure of open reduction, femoral shortening, and pelvic osteotomy in children older than 8 years of age.
This was a retrospective case series of 65 patients (77 hip joints) with DDH in patients older than 8 years of age (with open tri-radiated cartilage) operated between 2013 and 2015 at a Ghurki Trust Teaching Hospital in Lahore, Pakistan. Indication for surgery was limping gait in all patients. Patients with known neuromuscular and chromosomal disorders and those with prior surgical procedures of a pelvic or a femoral osteotomy were excluded. All patients had a minimum of two year of follow-up.
As our study was retrospective in nature and did not influence patient care, the need for ethical approval was waived by the institutional review board. Clinical data (i.e., pain symptoms, gait pattern, range of hip joint motion and presence of Trendelenburg sign) were recorded for each patient preoperatively and at the latest follow-up using the modified McKay's criteria8). The Tönnis classification system9) was used to assess the degree of dislocation of the femoral head. Radiographic evaluations (i.e., examination of preoperative and follow-up plain radiographs) were used to classify patients according to the Severin's grading system10).
A standardized pre-coded questionnaire was designed to collect the aforementioned clinical and radiological data. The data was then entered into IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA). Frequencies, percentages, means and standard deviations were computed where appropriate.
The operative procedure started with adductor tenotomy–performed through a small incision given directly over the tight adductors in the inguinal region. The Smith Petterson approach was used to expose the hip joint. Skin incision was initiated over the lateral iliac crest down to the anterior superior iliac spine, turning distally to follow the lateral side of the sartorius muscle. The interval between the sartorius and tensor fascia lata is developed. Exposing and severing the underlying tendon of the rectus femoris reveals the capsule covering the dislocated femoral head. Next, the glutei were peeled off from the outer table of the iliac bone and the iliacus from the inner table, enabling clear exposure of the iliac bone for any pelvic procedure. The capsule was then incised in a T-shaped manner to reveal the underlying femoral head and the deeply seated acetabular fossa. The ligamentum teres and transverse acetabular ligament were then divided to ensure a stable seating of the femoral head after clearing the acetabular fossa from soft tissues.
Next, the proximal femur was exposed through separate mid lateral incision and femoral osteotomy was conducted at the intertrochanteric region. The first cut in the femur was followed by open reduction. The amount of overlap in the femur was evaluated to determine the amount of femoral shaft to be resected. We noted that shortening of 2 to 3 cm was necessary to allow easy reduction of the femoral head while maintaining normal soft tissue tension across the hip. The osteotomy was then fixed with a four-hole plate and a varus fixation of roughly 10° to 15° was conducted. A derotation component was added in patients with femoral anteversion less than 30° by fixing the plate to the proximal femoral fragment and rotating distal fragment externally to bring patella to face the ceiling.
The pelvic procedure utilized in this study was triple osteotomy (47 hips) followed by double and Salter osteotomy in 18 and 12 hips, respectively. Triple pelvic osteotomy (i.e., iliac, pubic, and ischial osteotomy) was performed in the majority of cases because adequate displacement of the acetabular fragment was difficult without additional pubic and ischial osteotomies performed through the adductor incision. A full thickness bone graft was removed from the middle part of the iliac crest and trimmed to the shape of a wedge; the base should correspond approximately to the distance between the anterior superior and inferior spines. After osteotomy, the distal segment of the innominate bone containing the entire acetabulum was shifted forward, downward, and outward so that the osteotomy site was opened anterolaterally. The bone graft was inserted on its edge into the osteotomy site and held with two K wires. In double pelvic procedures, only the iliac and pubic osteotomies were done, with the ischium left intact, whereas in salter osteotomy only iliac osteotomy was performed. The decision for the type of pelvic osteotomy was made intra-operatively based on the patient's age and acetabular anatomy to allow adequate coverage of the femoral head.
Postoperatively, hips were immobilized in a 1 1/2 hip spica in position of slight flexion, abduction and internal rotation for 6 weeks. This was changed to an abduction splint for an additional 6 weeks, which allows non-weight bearing flexion and extension mobilization of the hip joints. K wires were removed after consolidation at the osteotomy site (typically at 6 weeks). Partial weight bearing started after 12 weeks with crutches for 2 weeks, followed by full weight bearing. Patients with bilateral dysplasia experienced the procedure on both hips at an interval of 6 weeks. The patients were followed up in the outpatient clinic at 4 month intervals during the first 2 years.
Clinico-pathological data on 19 boys and 46 girls with 53 unilateral dislocations (31 right unilateral dislocations, 22 left unilateral dislocations) and 12 bilateral dislocations were evaluated. The average age at presentation was 11.02±3.43 years (range, 8–15 years). According to the Tönnis classification, 68.8% patients had grade 3 or 4 dislocations. All patients had a minimum follow up of two years. A comprehensive demographic profile of patients is presented in detail in Table 1.
The criteria described by Severin are commonly used to assess the radiographic results following treatment of DDH. Postoperatively, no patients were classified as Severin grade V; 38 (49.4%), 19 (24.7%), 14 (18.2%), and 6 (7.8%) were classified as Severin grade I, II, III and IV, respectively. The pre- and postoperative distribution of patients according to radiological (Severin's criteria) and clinical (McKay's criteria) criteria are presented in Tables 2 and 3, respectively.
The clinical results-according to the Mackay's scoring system-were also favorable. At the conclusion of the study, the condition of hips was excellent (n=22, 28.6%), good (n=44, 57.1%), fair (n=9, 11.7%), and poor (n=2, 2.6%). The unsatisfactory cases were the nine fair patients (11.7%) with a stable painless hip, yet positive Trendelenburg sign and limitation of movement. Both patients with poor outcome had unstable, painful hip with evidence of AVN of the femoral head. No patients developed limb length discrepancy (LLD). Postoperative stiffness of the hip occurred in three patients. Repeated arthrotomy at the time of plate removal disclosed extensive scarring but no other intraarticular pathology.
In western countries, DDH is typically diagnosed early–likely due, in part, to existing screening programs. However, in developing countries like Pakistan, with low literacy rates, high prevalence of patients living in poverty, and a tendency to use alternative medicine (e.g., traditional and religious healers), DDH diagnosed in adolescence is still a common occurrence. Adding to the complexity in diagnosing DDH is a lack of access to health facilities due to a self-financed healthcare system and a lack of expertise in this complex condition. The majority of patients with DDH are girls, and as limping is a great handicap in Asian societies, it is especially difficult for them to get married or obtain employment. In view of these special cultural considerations-and because Asian societies often do not provide equal opportunities to the handicapped-most patients insist strongly on surgical treatment. Therefore, we performed open-reduction hip surgery in cases where there was even the slightest chance of restoring a normal joint structure, in patients aged over 8 years, and even in some postpubescent patients. Figures 1, 2, 3 illustrate preoperative and post-operative radiological outcomes of 3 such female patients.
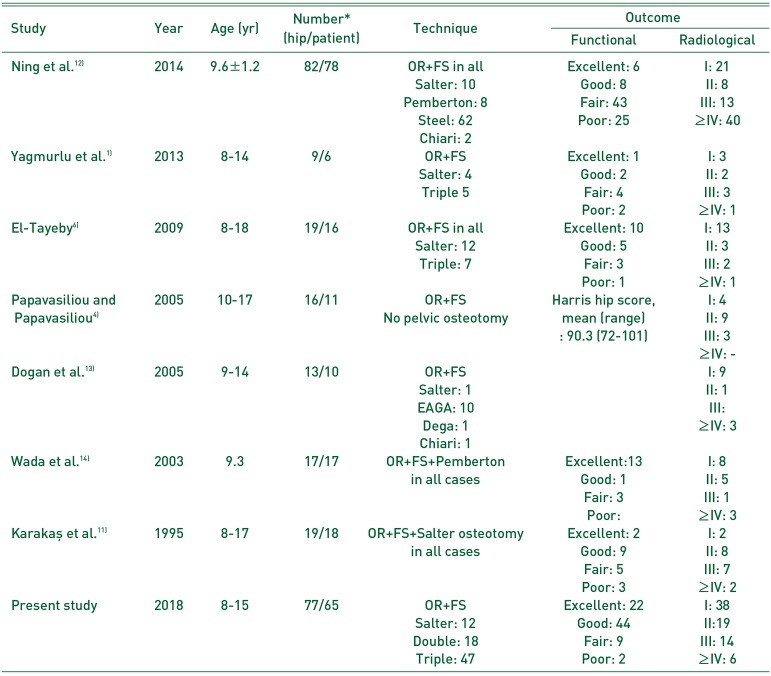
Management of neglected DDH for children 8 years of age and older is a matter of great controversy4). On reviewing the literature (Table 414611121314)), reports on the management of late, neglected DDH presenting after the age of 8 years were scarce, probably because there are so few cases of the condition in the developed world6). Few authors have suggested that operative treatment in neglected cases is not advisable, or even dangerous4). Others reported satisfactory results in evaluations of large series where open reduction with femoral shortening was employed3456); in these cases, ages at operation ranged from 3 to 1415), 4 to 102), 8 to 173), and 10 to 17 years4). In the current study, the age range was 8 to 15 years, with an average of 11 years. At a mean follow-up of 7.5 years, Karakaş et al.11) obtained good or excellent clinical and radiographic outcomes–according to McKay's and Severin's criteria, respectively-in 67% and 65% of 55 hips with a one-stage operation. Forlin et al.16) reported that in 20 DDH treatment-naïve children between the ages of 4 and 12 years who received a one-stage operation, 70% (n=17) of hips were in good or excellent condition (according to the McKay's and Severin's classifications) at mean follow up of 5 years. Interestingly, this group reported a higher likelihood of poor outcomes in patients who, at the time of surgery, were older than 7 years. Ganger et al.17) reported that 80% of hips treated with a one-stage operation experienced excellent or good results according to the Severin's classification after a mean follow-up of 3.5 years. Galpin et al.18) reported that 75% to 85% of patients experienced good radiographic and clinical results after open reduction combined with femoral shortening and pelvic osteotomy in children between 2 and 8 years of age. Importantly, each of these studies indicated that the younger the patients receive the operation, the better the results achieved; our findings reveal similar clinical and radiographic results.
Femoral shortening: i) facilitates reduction of the femoral head into the acetabulum by relaxing muscles around the hip joint, and ii) decreases pressure on the femoral head which reduces the risk of osteonecrosis and allows rotational realignment of the femoral head, resulting in a more stable reduction1). Vallamshetla et al.2) stated that “too much shortening is often better than too little” and this appears to be a critical commentary on one of the keys to successful reduction and excellent functional outcomes. Femoral shortening has little effect on leg length difference because bringing down the head into the acetabulum will compensate for such shortening to a great extent and the relative overgrowth of the femur after the osteotomy in children less than 12 years of age will correct the deficit in the follow-up period1). Regardless of the selected approach, a stable, painless, mobile hip should be the target1). In our study, none of the 12 patients who underwent single-stage corrective surgery for bilateral DDH experienced LLD. The two patients who developed AVN of the femoral head during follow up in our study, presented with leg length shortening on the operated side of 1.5 cm and 2 cm, respectively. The remaining patients in our study developed limb lengthening on the operated side of roughly 1 cm during the two year follow-up period. In our study, LLD was not considered a complication because it was not an issue which concerned the patient or the parents, and was found to decrease gradually at follow up. In our patients, a shoe lift was sufficient to address the LLD experienced in our patients.
Ok et al.3) indicated a belief that the first important surgical principle is an “excessive femoral neck varus”; femoral shortening up to 1.5 cm was their next concern. Such excessive varus places the femoral head deeply within the acetabulum, moreover, it minimizes the joint pressure after reduction. Shih and Shih7) indicated that they felt that a femoral neck shaft angle measuring 100° to 110° is the best radiographic outcome. Normal acetabular remodeling cannot be expected in the majority of hips after only varus derotation osteotomy in older children6). Based on our clinical judgement, varus derotation was conducted in only 11.7% (n=9) of patients included in this study; however, we cannot substantiate this with the measurement of neck shaft angle at the time of final follow-up. Indirect support of our decisions to not conduct a varus can be seen by the fact that the majority of our patients obtained good to excellent scores according to both Severin's and Mackay's scoring systems. A longer duration of follow-up would certainly be necessary to determine the eventual outcome of not adding a varus component to this treatment.
Papavasiliou and Papavasiliou4) did not mention any pelvic procedures adopted in their 11 patients (16 hips) with ages ranging from 10 to 17 years. In this series, pelvic osteotomy of some sort was required in all the cases to ensure adequate coverage of the femoral head. Modern surgical methods used to improve femoral head coverage are pelvic osteotomies: Chiari, Salter and the triple osteotomy. A comparison between these three methods is best made taking into account indications for all three methods, acetabulum dysplasia and hip incongruence in the adolescent age19).
The results of our study revealed a significant improvement in the radiological features of the operated hip joints with restoration of good function in more than three-quarters of patients. However, our study is limited by the short follow-up time (i.e., 2 years) which is not sufficient to evaluate the possibility of late-presenting Bucholz-Ogden type 2 osteonecrosis.
There are two major advantages in operative treatment of DDH in the periadolescent period. First, it may offer these patients a mobile and pain-free hip. Secondly, it may restore hip anatomy, thus increasing the probability of a successful hip replacement operation in adult life. Based on the experience presented here, we recommend the triple procedure of open reduction, femoral shortening and pelvic osteotomy for treatment of DDH in older children.
References
1. Yagmurlu MF, Bayhan IA, Tuhanioglu U, Kilinc AS, Karakas ES. Clinical and radiological outcomes are correlated with the age of the child in single-stage surgical treatment of developmental dysplasia of the hip. Acta Orthop Belg. 2013; 79:159–165. PMID: 23821967.
2. Vallamshetla VR, Mughal E, O'Hara JN. Congenital dislocation of the hip. A re-appraisal of the upper age limit for treatment. J Bone Joint Surg Br. 2006; 88:1076–1081. PMID: 16877609.
3. Ok IY, Kim SJ, Ok JH. Operative treatment of developmental hip dysplasia in children aged over 8 years. J Pediatr Orthop B. 2007; 16:256–261. PMID: 17527102.

4. Papavasiliou VA, Papavasiliou AV. Surgical treatment of developmental dysplasia of the hip in the periadolescent period. J Orthop Sci. 2005; 10:15–21. PMID: 15666117.

5. Ashley RK, Larsen LJ, James PM. Reduction of dislocation of the hip in older children: a preliminary report. J Bone Joint Surg Am. 1972; 54:545–550. PMID: 5055152.
6. El-Tayeby HM. One-stage hip reconstruction in late neglected developmental dysplasia of the hip presenting in children above 8 years of age. J Child Orthop. 2009; 3:11–20. PMID: 19308607.

7. Shih CH, Shih HN. One-stage combined operation of congenital dislocation of the hips in older children. J Pediatr Orthop. 1988; 8:535–539. PMID: 3170731.

8. McKay DW. A comparison of the innominate and the pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res. 1974; (98):124–132. PMID: 4817221.

9. Tönnis D. Congenital hip dislocation. Avascular necrosis. New York: Thieme-Stratton;1982.
10. Severin E. Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand. 1941; 84(Suppl 63):1–142.
11. Karakaş ES, Baktir A, Argün M, Türk CY. One-stage treatment of congenital dislocation of the hip in older children. J Pediatr Orthop. 1995; 15:330–336. PMID: 7790490.

12. Ning B, Yuan Y, Yao J, Zhang S, Sun J. Analyses of outcomes of one-stage operation for treatment of late-diagnosed developmental dislocation of the hip: 864 hips followed for 3.2 to 8.9 years. BMC Musculoskelet Disord. 2014; 15:401. PMID: 25432778.

13. Dogan M, Bozkurt M, Sesen H, Yildirim H. One-stage treatment of congenital severely dislocated hips in older children through various acetabuloplasty techniques: 22 children followed for 1–5 years. Acta Orthop. 2005; 76:212–219. PMID: 16097546.
14. Wada A, Fujii T, Takamura K, Yanagida H, Taketa M, Nakamura T. Pemberton osteotomy for developmental dysplasia of the hip in older children. J Pediatr Orthop. 2003; 23:508–513. PMID: 12826952.

15. Browne RS. The management of late diagnosed congenital dislocation and subluxation of the hip-with special reference to femoral shortening. J Bone Joint Surg Br. 1979; 61:7–12. PMID: 422637.

16. Forlin E, Munhoz da Cunha LA, Figueiredo DC. Treatment of developmental dysplasia of the hip after walking age with open reduction, femoral shortening, and acetabular osteotomy. Orthop Clin North Am. 2006; 37:149–160. viPMID: 16638446.

17. Ganger R, Radler C, Petje G, Manner HM, Kriegs-Au G, Grill F. Treatment options for developmental dislocation of the hip after walking age. J Pediatr Orthop B. 2005; 14:139–150. PMID: 15812282.

18. Galpin RD, Roach JW, Wenger DR, Herring JA, Birch JG. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg Am. 1989; 71:734–741. PMID: 2732262.

19. Vukasinović Z, Spasovski D, Zivković Z, Slavković N, Cerović S. Triple pelvic osteotomy in the treatment of hip dysplasia. Srp Arh Celok Lek. 2009; 137:239–248. PMID: 19594064.
Fig. 1
Case presentation of a 10 year-old female with neglected developmental dysplasia of hip (DDH). (A) Preoperative X-ray showing left side Tönnis grade 4 DDH. (B) Immediate postoperative X-ray after open reduction, femoral shortening and triple pelvic osteotomy. (C) The follow-up X-ray after 6 months. (D) The follow-up X-ray after 2 years revealing congruent hip joint without evidence of avascular necrosis in femoral head. (E) Clinical picture illustrating patient's ability to squat.
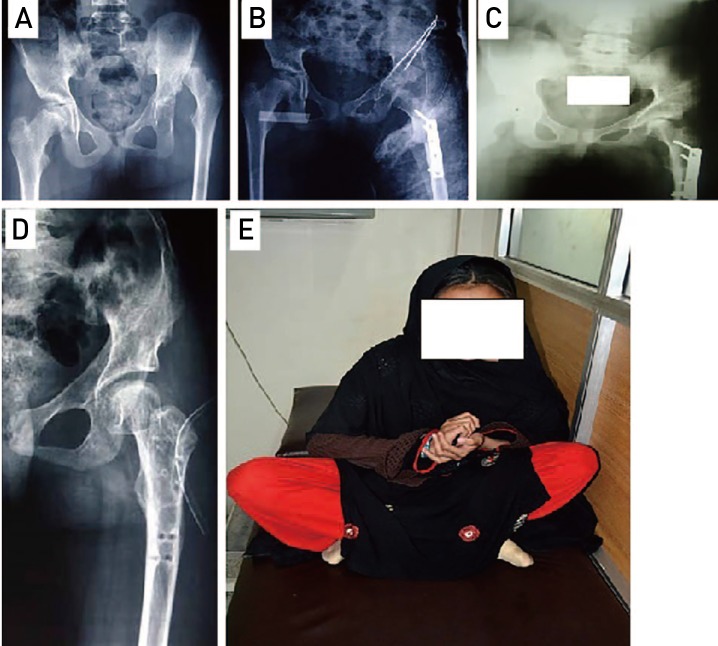
Fig. 2
Case presentation of an 11 year-old female with neglected developmental dysplasia of hip (DDH). (A) Preoperative X-ray showing bilateral Tönnis grade 4 DDH. (B) Immediate postoperative X-ray after bilateral open reduction, femoral shortening and Salter osteotomy on right side and double pelvic osteotomy on left side. (C) The follow-up X-ray after 1 year. (D) The follow up X-ray after removal of femur plates showing congruent hip joint bilaterally after two year. However, there is evidence of avascular necrosis in femur head on left side.
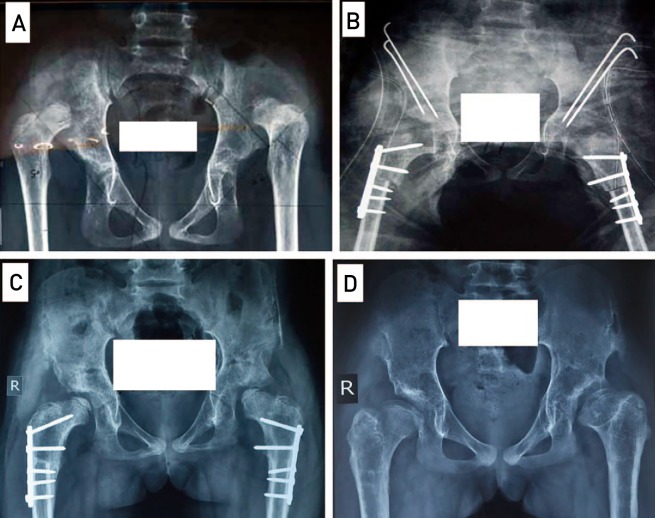
Fig. 3
Case presentation of 12 year-old female with neglected developmental dysplasia of hip (DDH). (A) Preoperative X-ray shows Tönnis grade 4 DDH on the right side. (B) Immediate postoperative X-ray after open reduction, femoral shortening and Salter osteotomy. (C) The follow-up X-ray after 1 year. (D) The follow-up X-ray after 2 years showing congruent hip joint with evidence of avascular necrosis in femur head.
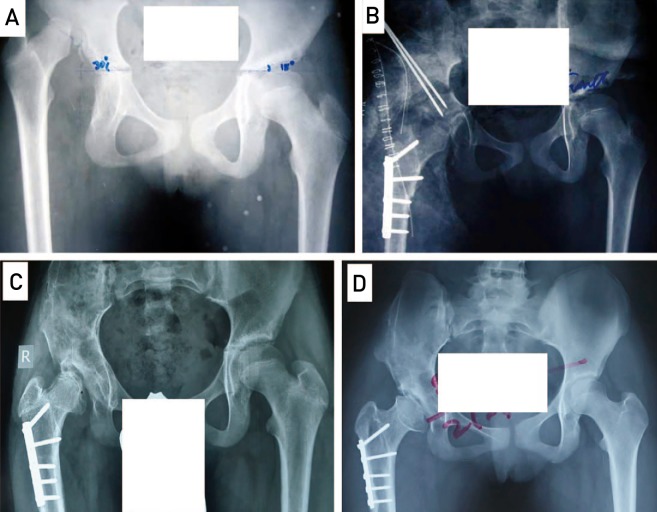
Table 1
Clinico-demographic Profile of Patients
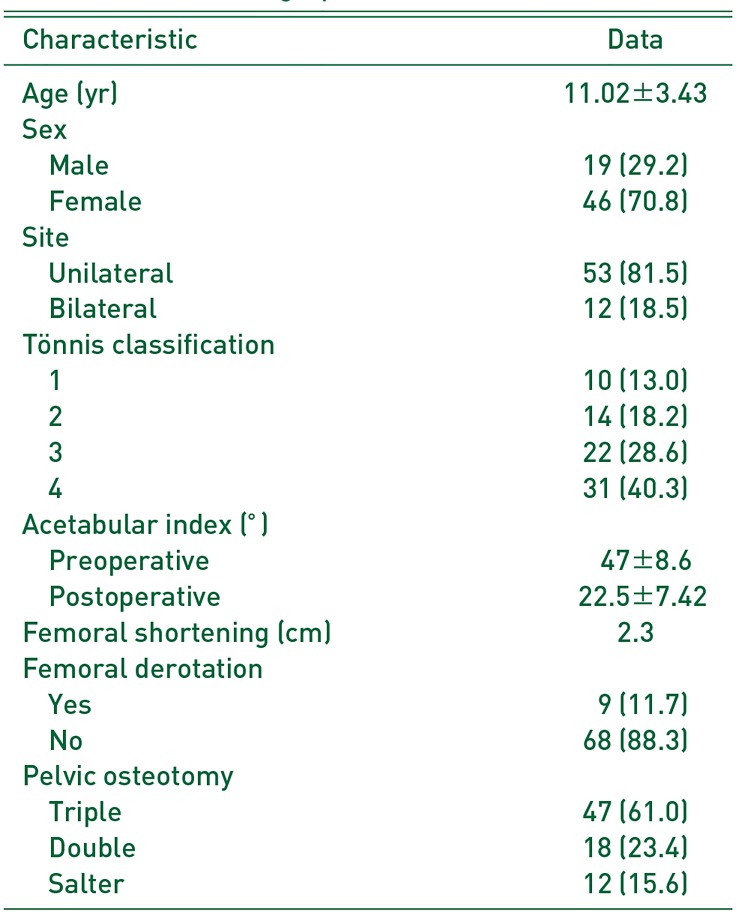
Table 2
Functional Outcome according to Mckay's Criteria
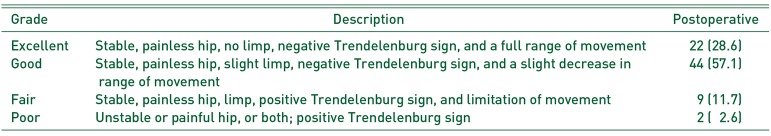
Table 3
Radiological Outcomes according to Severin's Classification
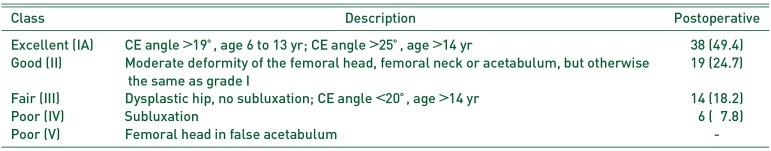
Table 4
Comparison of Results from Published Studies
| Study | Year | Age (yr) | Number* (hip/patient) | Technique | Outcome | |
|---|---|---|---|---|---|---|
| Functional | Radiological | |||||
| Ning et al.12) | 2014 | 9.6±1.2 | 82/78 | OR+FS in all | Excellent: 6 | I: 21 |
| Salter: 10 | Good: 8 | II: 8 | ||||
| Pemberton: 8 | Fair: 43 | III: 13 | ||||
| Steel: 62 | Poor: 25 | ≥IV: 40 | ||||
| Chiari: 2 | ||||||
| Yagmurlu et al.1) | 2013 | 8–14 | 9/6 | OR+FS | Excellent: 1 | I: 3 |
| Salter: 4 | Good: 2 | II: 2 | ||||
| Triple 5 | Fair: 4 | III: 3 | ||||
| Poor: 2 | ≥IV: 1 | |||||
| El-Tayeby6) | 2009 | 8–18 | 19/16 | OR+FS in all | Excellent: 10 | I: 13 |
| Salter: 12 | Good: 5 | II: 3 | ||||
| Triple: 7 | Fair: 3 | III: 2 | ||||
| Poor: 1 | ≥IV: 1 | |||||
| Papavasiliou and Papavasiliou4) | 2005 | 10–17 | 16/11 | OR+FS | Harris hip score, mean (range) : 90.3 (72–101) | I: 4 |
| No pelvic osteotomy | II: 9 | |||||
| III: 3 | ||||||
| ≥IV: - | ||||||
| Dogan et al.13) | 2005 | 9–14 | 13/10 | OR+FS | I: 9 | |
| Salter: 1 | II: 1 | |||||
| EAGA: 10 | III: | |||||
| Dega: 1 | ≥IV: 3 | |||||
| Chiari: 1 | ||||||
| Wada et al.14) | 2003 | 9.3 | 17/17 | OR+FS+Pemberton in all cases | Excellent:13 | I: 8 |
| Good: 1 | II: 5 | |||||
| Fair: 3 | III: 1 | |||||
| Poor: | ≥IV: 3 | |||||
| Karakas¸ et al.11) | 1995 | 8–17 | 19/18 | OR+FS+Salter osteotomy in all cases | Excellent: 2 | I: 2 |
| Good: 9 | II: 8 | |||||
| Fair: 5 | III: 7 | |||||
| Poor: 3 | ≥IV: 2 | |||||
| Present study | 2018 | 8–15 | 77/65 | OR+FS | Excellent: 22 | I: 38 |
| Salter: 12 | Good: 44 | II:19 | ||||
| Double: 18 | Fair: 9 | III: 14 | ||||
| Triple: 47 | Poor: 2 | ≥IV: 6 | ||||




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download