Abstract
Purpose
This study was performed to compare the: i) 1-year survival rate of patients with hip fractures, ii) factors affecting mortality in patients with hip fractures, and iii) results of functional recovery at commissioned hospitals (CH) and veterans hospitals (VH) to characterize the quality of care provided in the Korean commissioned hospital system.
Materials and Methods
The study population consisted of 183 veteran patients (84 and 99 treated at a single VH and 39 CH, respectively) who underwent hip fracture surgery between January 2010 and February 2015. This study compared baseline characteristics (i.e., age, comorbidities, fracture types and surgical treatment approaches) of the two groups vs. clinical outcomes, and evaluated the waiting time, length of hospital stay, total medical expenses, mortality rate within one year, and functional recovery at last follow up.
Results
There were no significant differences in age, fracture types, comorbidities, ambulatory status before fracture, waiting time, or length of hospital stay between the two groups, however, the total medical cost was higher in the CH group (P=0.009). There was no significant difference in mortality within one year after hip fracture (P=0.224) or functional recovery at last follow-up (P=0.463) between the two groups.
The Korean population is aging faster than other developed countries1). Hip fractures are one of the most serious nonfatal injuries associated with falls in seniors, and are associated with high mortality, severe health problems, and low quality of life2345). Korean veterans experiencing a hip fracture can be treated at no cost to the patient at one of the 5 national veterans hospitals (VH), however, due to travel limitations of patients experiencing hip fractures, the 5 national VH may be insufficient to treat all patients. To overcome this unmet need, the Korea Veterans Health Service (KVHS) implemented the commissioned hospital (CH) system in 1986. Specifically, the KVHS assigned several hospitals in each province to offer full-cost coverage equivalent to VH in order to prevent any delays in the treatment of veterans suffering from injuries that render them incapable of traveling long distances. Evaluating the efficiency of the CH system can help ensure that veterans receive proper care and inform any necessary revisions. Whereas comparative studies on the treatment results between VH and CH have been undertaken internationally 67891011), similar studies specific to Korea have not yet been conducted. We compared the 1-year survival rates and other clinical outcomes of patients treated for hip fractures at VH vs. CH to determine the operating status of the CH system.
The study population consisted of 183 veteran patients who underwent hip fracture surgery; 84 patients were treated at a single VH and 99 were treated across 39 CH in the Honam region of South Korea, including a major city Gwangju and two provinces, between January 2010 and February 2015. All patients were male, and there were no bilateral fractures. The mean ages and body mass indexes (BMIs) of the two groups were compared, and fracture types were characterized as femur neck fractures or intertrochanteric fractures depending on fracture location. Length of hospitalization and total medical costs (i.e., sum of medical costs claimed by VH and CH to the KVHS and out-of-pocket payments) were compared. The VH group had no co-payment and the CH group had a co-payment for arbitrary uninsured materials and others. Patient capacity for activity before the hip fracture was classified as either: level 1, independent ambulator (patient able to perform activities alone or with walking-assistance tools such as cane and walker); level 2, dependent ambulator (patient required assistance from another individual to perform activities); and level 3, non-functional ambulator (patient incapable of activities other than moving in a wheelchair or resting in bed)12). The capacity for activity and death were evaluated retrospectively using hospital records, nursing home records, and phone calls to patients or their lineal family members. When information could not be easily obtained from patients or their lineal family members, or patients could not be contacted in the process of the survey, contact information could be obtained with the help of government offices to accurately determine if the patient had died or not and, in cases of death, when the death had occurred.
We classified the patients who died within one year following surgery into four groups according to the time of death: i) within 30 days, ii) within 90 days, iii) within 180 days, and vi) greater than 180 days post-surgery. We compared their preexisting comorbidities (i.e., dementia, ambulatory status before fracture, duration between injury and surgery) and surgical approach taken. Patients' medical histories, blood tests, and progress notes were used for analysis. We further analyzed patients with more than three comorbidities.
All data were statistically processed with the SPSS software version 17.0 (SPSS Inc, Chicago, IL, USA), with a P-value of <0.05 set as statistically significant. Kaplan-Meier survival analyses were performed with a one-year mortality end point. Student t-tests and chi-square tests were performed to compare between VH and CH groups and between deceased patients and survivors. Logistic regression analysis was used to determine factors that affected death.
There was no significant differences in age (VH=76.0 years and CH=76.6 years; P=0.667) or mean BMI (VH=22.1 and CH=21.9 kg/m2; P=0.654) among patients treated at VH and CH. Femur intertrochanteric fractures were more prevalent than neck fractures in both groups (VH group ratio, 46:38; CH group ratio, 60:39) (P=0.425). As shown in Table 1, there was no significant difference (P=0.798) in ambulatory status before fracturs when patients were divided into one of three stages (VH group: level 1 [n=58], level 2 [n=24], level 3 [n=2]; CH group: level 1 [n=69], level 2 [n=26], level 3 [n=4]). Hip hemiarthroplasty was performed on 36 cases with femoral neck fracture and 11 cases with intertrochanteric fracture in the VH group; and 38 cases with femoral neck fracture and 15 cases with intertrochanteric fracture in the CH group. Hip hemiarthroplasty was the most frequently performed surgical method in both groups (47 of 84 cases in the VH group; 53 of 99 cases in the CH group; P=0.273). The mean duration from injury to surgery was 2.3 days (range, 0–7 days) in the VH group and 2.5 days (range, 0–9 days) in the CH group; both groups performed surgery within 3 days (P=0.624) (Table 1). There were no significant differences between the two groups in terms of the prevalence of hypertension (P=0.106), diabetes (P=0.124), liver disease (P=0.896), cerebrovascular disease (P=0.259), cardiovascular disease (P=0.137), kidney disease (P=0.186), pulmonary disease (P=0.771), and dementia (P=0.540). There were 41 (48.8%) and 40 (40.4%) patients with three or more comorbidities in the VH and CH groups, respectively, and the difference was not significant (P=0.254). The mean duration of hospitalization was 24.47 days (and 10–61 days) for VH group and 24.02 days (8–66 days) for CH group, but the total medical cost was significantly higher in CH group (mean cost, 10,184,780 Korean won; P=0.009) (Table 1).
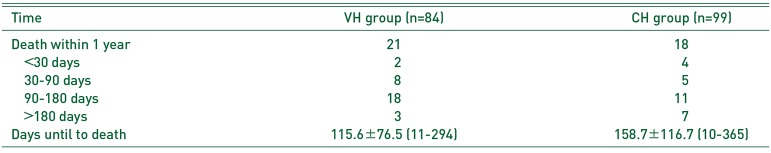
The number of death within one year was 21 (25.0%) in the VH group; the mean survival time was 115.6±76.5 days (range, 11–294 days) post-surgery. These deaths occurred within 30 days (n=2), within 90 days (n=8), within 180 days (n=18) of surgery. Three deaths occurred more than 180 days after the surgery. In the CH group, the number of death within one year was 18 (18.2%), with a mean survival time of 158.7±116.7 days (range, 10–365 days) post-surgery. These deaths occurred within 30 days (n=4), within 90 days (n=5), within 180 days (n=11) of surgery. Seven deaths occurred more than 180 days after the surgery (Table 2). Factors significantly affecting mortality in the VH group were renal disease (P=0.003), age (P=0.012), ambulatory status before fracture (P=0.020). In the CH group, cerebrovascular disease (P=0.016), age (P=0.002) and renal disease (P=0.002) were shown to significant affect mortality (Table 3). There was no significant difference between the two groups in the Kaplan-Meier survival analysis (P=0.224).
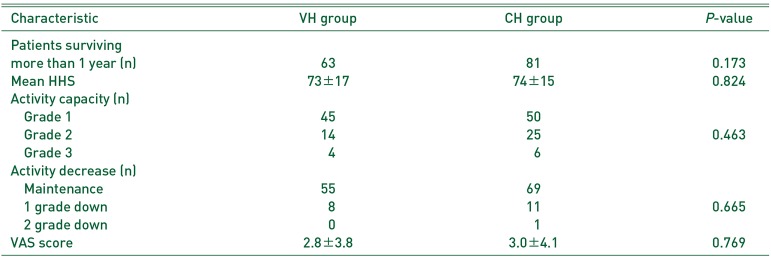
Eighty-one and 63 patients in the VH and CH groups, respectively, survived for more than a year after surgery and received clinical functional recovery evaluations. The mean HHS at last follow up of the VH and CH groups were not significantly different (73±17 [VH] and 74±15 [CH]; P=0.824). There was also no significant difference between gait recovery assessment at last follow up (VH group: level 1 [n=45], level 2 [n=14], level 3 [n=4]; CH group: level 1 [n=50], level 2 [n=25], level 3 [n=6]) (P=0.463). Two step declines in gait recovery were experienced by 0 patients in VH group and 1 in CH group, and one step declines were experienced by 8 patients in VH group and 11 in CH group (P=0.665). As shown in Table 4, the mean VAS scores were 2.8±3.8 for VH group and 3.0±4.1 for CH group, and there were no significances in the VAS score between the groups at last follow up (P=0.769).
The KVHS, established by the Korean government in November 1981 to be operated by the Ministry of Patriots and Veterans Affairs, is a semi-governmental agency which performs government-commissioned tasks pertaining to the health care and welfare of veterans. Korean veterans are provided government-funded medical care for acute and chronic disease at one of 5 VHs located nationwide15). However, it has become difficult for veterans, especially seniors, who live far from a VH to travel and be treated in these facilities. When required, the delivery of emergency services is particularly challenging. Thus, the KVHS commissioned a number of non-VH (designated CH) to provide medical care for national veterans to ensure that they receive prompt care near their residences during emergencies6). Since two hospitals on Jeju Island were first designated as CH in 1986, the total number of CH nationwide grew to 314 by September 20166). The number of hospitals designated as CH has been increasing year by year (n=56 in 1996, n=200 in 2007, and n=314 in 2016) to provide respectful and prompt treatment of veteran patients. On the contrary, the number of veterans is decreasing every year due to aging (n=782,430 in 2009 and n=734,135 in 2015). Therefore, it is very important to evaluate the propriety of the CH system operation in Korea to ensure that it is sufficient, but not excessive.
A similar system was implemented in the United States in November 1999, which was followed by vigorous studies comparing the therapeutic outcomes of patients admitted for emergencies between VH and CH in order to evaluate their benefit and reliability 7891011). The purpose of the CH system is to ensure that there is no delay in treatment. Cardiac disease and hip fracture are conditions which require prompt treatment in order to reduce mortality161718). Thus, a study on treatment delay and mortality is commonly used to evaluate the propriety of CH891011). Such studies are actively conducted in the United States and many other countries 6789101119) where VH systems are in place. Although Korea implemented the CH system 13 years prior to the United States, there are no studies comparing mortalities at VH vs. CH to analyze the propriety of the CH system for the surgical treatment of hip fractures. Richardson et al.10) reported that admissions at CH were associated with a 21% lower relative risk of death within one year compared to VH admissions, while Hutt et al.9) reported that Medicare beneficiaries with hip fracture repair in non-VH had better survival rates than veterans in VH facilities. Several factors (e.g., the presence of other medical illnesses, severity of illnesses, and duration between injury and surgery) may affect mortality following a hip fracture11161718). There are several factors affecting the mortality after hip fracture, including the patient's medical comorbidities, the severity of illness, and delay on surgery13161720). Richardson et al.10) suggested that patients treated at CH have lower mortality rates than those treated at VH because admission of veterans with hip fractures to a CH was associated with a shorter time to surgery. Based on this finding, the study suggests that multiple hospitals in the vicinity of veterans' residences must be designated as CH to increase veterans' accessibility to medical care and reduce hip fracture-associated mortality within one year of injury.
Nevertheless, the authors found no significant differences in the mortality rate within one year and waiting time between the CH and the VH groups in this study. In Korea, the number of veteran patients is decreasing annually and travel from residences to downtowns is becoming increasingly convenient with well-developed public transport and road networks. Little time is spent traveling from residence to a CH20), and no waiting for inpatient admission or surgery delay occurred in either hospital groups in our study, implying that the current number of CHs is sufficient21). Hutt et al.9) suggest that non-VH survival rates are superior to those at VH facilities because Veterans' Health Administration patients were more ethnically diverse, and have greater comorbidities than non-veterans. The results of a study by Hutt et al.9) are similar to those found here; Korean veterans are also elderly with comorbidities which consider veteran patients with hip fracture as high mortality risk group. On the other hand, in this study, patients treated in the VH and CH were of a single ethnicity and did not exhibit significantly different medical comorbidities, implying that the presence and number of medical comorbidities did not contribute to the significant difference in mortalities between the two groups. However, in the authors' study, patients treated at VH and CH groups consisted a single ethnicity, Asian, and did not exhibit significantly different age and medical comorbidities between two groups. This implies the presence and number of medical comorbidities did not contribute to the significant difference in mortalities between the two groups. In other words, the treatment range and abilities at CH is sufficient for the treatment of high-risk patients who need treatment for hip fractures, and there is no further need to transfer these patients to VH. Therefore, the existing CH system is estimated to be sufficient since the treatment range and abilities (types and numbers of medical care and medical equipment) are considered to be equal to or greater than the range and abilities at VH.
Preexisting medical illnesses, particularly metastatic cancer, renal failure, lymphoma, weight loss, and liver disease, are known to lead to increased risks of mortality following hip fracture11). In this study, the medical comorbidities significantly correlated with death within one year are renal disease and cerebrovascular disease in the VH and CH groups, respectively. Similar to the results of Bernstein22), age was significantly associated with death in both groups; in senior patients, the difference in mean age has a significant effect on the one-year mortality rate. Korea is entering a time of a super-aging society, and the average age of veterans is 72 years as of 201516). The treatment process will require more careful attention if a senior veteran with hip fracture visits a hospital, especially one with comorbidities (i.e., kidney or cerebrovascular disease) since he or she is considered to be at a high risk of mortality. However, since various factors can contribute to death, long-term multicenter studies are warranted to examine additional preoperative factors and their associations with mortality (e.g., fracture location and type, American Society of Anesthesiologists' classification, preoperative laboratory data [e.g., sodium, hemoglobin, and serum albumin]23) and severity of medical comorbidity). Similar to the results of the study by Aharonoff et al.24) which showed that preinjury dependency in basic activities of daily living is a predictor of one-year mortality in hip fractures in the elderly, this study shows that preoperative gait ability of the VH group had a significant effect on death within one year.
This is the first study in Korea to examine the propriety of CH system for veterans. In this study, ambulatory status before fracture affected mortality of patients treated at VH, but not at CH, however walking classifications were simplified (i.e., included only 3 levels). Further studies on gait recovery with more sensitivity (i.e., more levels) may be beneficial. We consider the number of CH and the care provided to be appropriate since there there was no significant difference in hip fracture-associated mortality or functional recovery between those treated at VH and CH. Additionally, no significant differences were found between those treated at VH or CH in: i) comorbidities, ii) 1-year post-surgery mortality, or iii) recovery of mobility among patients who survived for more than 1 year. These outcomes are assumed to be attributable to the fact that the current selection criteria for choosing CHs are valid. However, additional studies are required to further evaluate the severity of comorbid conditions. Considering the number of CH is increasing every year while the number of veteran patients is decreasing, there should be further study on evaluation on propriety of medical cost in CH since the cost is higher in CH than in VH, even though there is no difference in the length of hospital stay and surgery methods. Despite no differences in fracture type, surgical methods or hospitalization periods, we suggest that a significantly higher medical cost in CH than in VH is related to the costs of out-of-pocket expenses for materials that are uninsured by medical benefits in VHs. Therefore, the Korea Veterans Health Service should allow the use of mandatory materials necessary for the treatment of veteran patients and should cover medical costs associated with using these materials through examination on a regular basis. On the contrary, the use of unnecessary materials should be limited in order to reduce the burdens of patients for the purposes of the CH system.
Our study has several limitations. First, the number of cases is small, and does not include all Korean VH and CH, and did not consider regional characteristics. Since VH does not disclose patient information between VHs, and only basic information about patients who have been treated for CH in Korea is reported to the Korea veterans commissioned hospital system management team's management committee, additional studies are needed to acquire patient data from CHs to more comprehensively evaluate the CH system. Secondly, the degree of gait or accompanying disease is not subdivided, and it is difficult to evaluate the severity with medical records alone, so it is necessary to establish detailed criteria for objective evaluation. We had difficulties in data gathering and statistical analysis because of different evaluation criteria for patient's conditions (e.g., walking ability and comorbidities) between those treated at VH and CH. To overcome this challenge, computerization and comparison of medical data should be made easy by using a standardized medical record tool in CH and VH. It is anticipated that this process may aid in the evaluation and updates to the CH system. Finally, it is difficult to assess the propriety of the CH system using only hip fractures. Therefore, it is necessary to study the treatment results from diverse diseases that may develop in senior veterans in the future.
There was no delay in surgery in either hospital groups and there was no difference in the mortality rate within one year or functional recovery at last follow up after the treatment of the hip fracture in both VH and CH. The Korean CH system is operating well in accordance with its purpose. However, since there is no significant difference in treatment outcomes and clinical outcomes, further study on the propriety of future medical expenses of CH higher than VH is suggested.
References
1. Hyun KR, Kang S, Lee S. Population aging and healthcare expenditure in Korea. Health Econ. 2016; 25:1239–1251. PMID: 26085120.

2. Sterling DA, O'Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001; 50:116–119. PMID: 11231681.

3. Hall SE, Williams JA, Senior JA, Goldswain PR, Criddle RA. Hip fracture outcomes: quality of life and functional status in older adults living in the community. Aust N Z J Med. 2000; 30:327–332. PMID: 10914749.

4. French DD, Werner DC, Campbell RR, et al. A multivariate fall risk assessment model for VHA nursing homes using the minimum data set. J Am Med Dir Assoc. 2007; 8:115–122. PMID: 17289542.

6. List of consigned hospitals [Internet]. Sejong: Ministry of Patriots and Veterans Affairs;2014. 3. 17. cited 2017 Sep 10. Available from: http://www.mpva.go.kr/support/support250_view.asp?id=1982&ipp=10.
7. Gordon HS, Aron DC, Fuehrer SM, Rosenthal GE. Using severity-adjusted mortality to compare performance in a Veterans Affairs hospital and in private-sector hospitals. Am J Med Qual. 2000; 15:207–211. PMID: 11022367.
8. Lapcevic WA, French DD, Campbell RR. All-cause mortality rates of hip fractures treated in the VHA: do they differ from Medicare facilities? J Am Med Dir Assoc. 2010; 11:116–119. PMID: 20142066.

9. Hutt E, Radcliff TA, Henderson W, Maciejewski M, Cowper-Ripley D, Whitfield E. Comparing survival following hip fracture repair in VHA and Non-VHA facilities. Geriatr Orthop Surg Rehabil. 2015; 6:22–27. PMID: 26246949.

10. Richardson KK, Cram P, Vaughan-Sarrazin M, Kaboli PJ. Fee-based care is important for access to prompt treatment of hip fractures among veterans. Clin Orthop Relat Res. 2013; 471:1047–1053. PMID: 23322188.

11. Bass E, French DD, Bradham DD, Rubenstein LZ. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. 2007; 17:514–519. PMID: 17420142.

12. Cho HM, Lee K, Min W, et al. Survival and functional outcomes after hip fracture among nursing home residents. J Korean Med Sci. 2016; 31:89–97. PMID: 26770043.

13. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755. PMID: 5783851.
14. Maxwell C. Sensitivity and accuracy of the visual analogue scale: a psycho-physical classroom experiment. Br J Clin Pharmacol. 1978; 6:15–24. PMID: 666944.
15. Basic status of Veterans subject to end of July 2016 (including location) [Internet]. Sejong: Ministry of Patriots and Veterans Affairs;2016. 8. 05. cited 2017 Sep 10. Available from: http://www.mpva.go.kr/info/info600_view.asp?id=5621&ipp=50.
16. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004; 291:1738–1743. PMID: 15082701.

17. Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006; 332:947–951. PMID: 16554334.

18. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009; 91:922–927. PMID: 19567858.

19. Ireland AW, Kelly PJ, Cumming RG. Risk factor profiles for early and delayed mortality after hip fracture: Analyses of linked Australian Department of Veterans' Affairs databases. Injury. 2015; 46:1028–1035. PMID: 25813734.

20. Veterans' medical care support performance [Internet]. Daejeon: Statistics Korea;2018. 2. 23. cited 2017 Sep 10. Available from: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1566#quick_05.
21. Park BJ, Cho HM, Choi YS, Seo JW. What is important in selecting a designated hospital for the Korean veterans with hip fractures? Hip Pelvis. 2017; 29:97–103. PMID: 28611960.

22. Bernstein J. Fee-based care is important for access to prompt treatment of hip fractures among veterans. Clin Orthop Relat Res. 2013; 471:2036. PMID: 23546849.
23. Pimlott BJ, Jones CA, Beaupre LA, Johnston DW, Majumdar SR. Prognostic impact of pre-operative albumin on short-term mortality and complications in patients with hip fracture. Arch Gerontol Geriatr. 2011; 53:90–94. PMID: 20684997.

24. Aharonoff GB, Koval KJ, Skovron ML, Zuckerman JD. Hip fractures in the elderly: predictors of one year mortality. J Orthop Trauma. 1997; 11:162–165. PMID: 9181497.

Table 1
Baseline Demographics of Patients Treated in the Veteran Hospital (VH) and Commissioned Hospital (CH) Groups
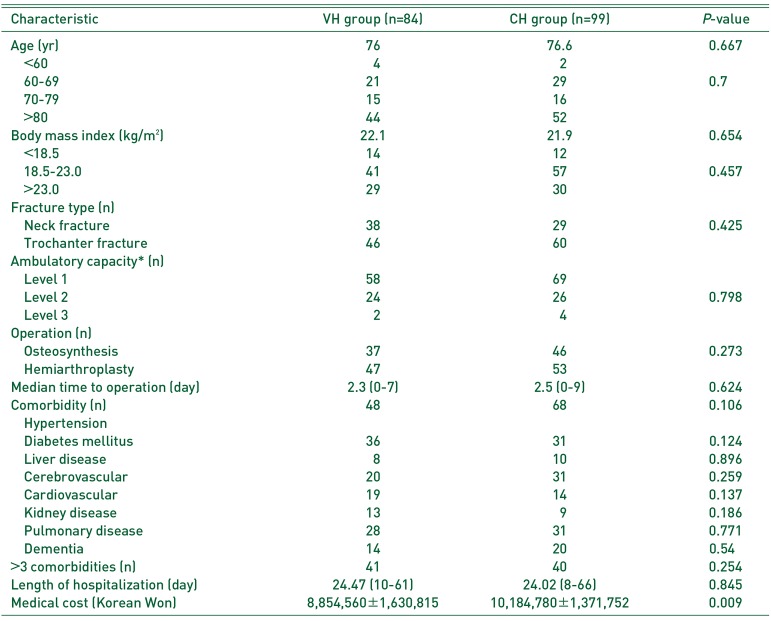
Table 2
The Analysis of Time to Death within One Year of Treatment
| Time | VH group (n=84) | CH group (n=99) |
|---|---|---|
| Death within 1 year | 21 | 18 |
| <30 days | 2 | 4 |
| 30–90 days | 8 | 5 |
| 90–180 days | 18 | 11 |
| >180 days | 3 | 7 |
| Days until to death | 115.6±76.5 (11–294) | 158.7±116.7 (10–365) |
Table 3
The Analysis of Underlying Disease
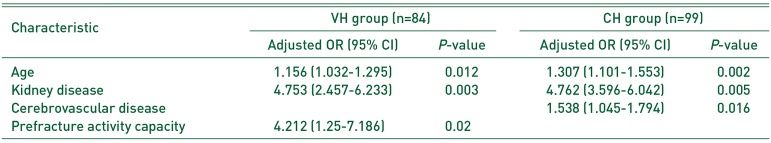
Table 4
Clinical Functional Outcomes at Final Follow-up of Patients Surviving More than One Year




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download