Abstract
Purpose
To compare and analyze clinical and radiologic outcomes of cemented versus cementless bipolar hemiarthroplasty for treatment of femur neck fractures.
Materials and Methods
A total of 180 patients aged 65 years and over older who underwent bipolar hemiarthroplasty for treatment of displaced femur neck fractures (Garden stage III, IV) from March 2009 to February 2014 were included in this study. Among the 180 patients, 115 were treated with cemented stems and 65 patients with cementless stems. Clinical outcomes assessed were: i) postoperative ambulatory status, ii) inguinal and thigh pain, and iii) complications. The radiologic outcome was femoral stem subsidence measured using postoperative simple X-ray.
Results
The cemented group had significantly lower occurrence of complications (postoperative infection, P=0.04) compared to the cementless group. There was no significant difference in postoperative ambulatory status, inguinal and thigh pain, and femoral stem subsidence.
Conclusion
For patients undergoing bipolar hemiarthroplasty, other than complications, there was no statistically significant difference in clinical or radiologic outcomes in our study. Selective use of cemented stem in bipolar hemiarthroplasty may be a desirable treatment method for patients with poor bone quality and higher risk of infections.
The incidence of osteoporotic fragility fractures continues to increase along with an aging global population. Selection of adequate treatment is very important, since hip fractures, including femur neck fractures, may lead to complications such as chronic pain, disability, low quality of life, high morbidity and mortality rates, and others1234).
In the treatment of older patients with displaced femur neck fracture, bipolar hemiarthroplasty (BHA) is a more commonly accepted treatment, compared with internal fixation, because this modality offers advantages including earlier ambulation, a lower probability of reoperation and better functional outcomes56). In BHA, whether there is a better choice between cemented or cementless stems still raises much controversy178). The use of cementless stems is considered a better choice for relatively younger elderly patients with good bone quality as it has the advantage of being an easier surgical procedure and involves a shorter cement manipulation time. However, this approach has some disadvantages, including risk of thigh pain and periprosthetic fractures567891011). The use of cemented stems has been shown to be better in achieving initial fixation in older patients with poor bone quality and is less likely to result in thigh pain and stem loosening, however, is reported to have a higher risk of cardiovascular and respiratory complications due to cement toxicity or pulmonary embolization caused by bone marrow contents and methylmethacrylate particles9101112131415). This study aimed to compare and analyze clinical and radiologic outcomes in cemented versus cementless BHA for treatment of femur neck fractures in patients older than 65 years with a minimum follow-up of six months.
This retrospective study included a total of 180 patients aged 65 years and over who underwent BHA for treatment of displaced femur neck fractures (Garden stage III and IV) in Inje University Sanggye Paik Hospital (Seoul, Korea) from March 2009 to February 2014 with a minimum follow-up of six months. Patients who had pathologic fractures due to malignant disease, received bilateral hip replacements, or accompanied fractures at different sites other than the hip were excluded. This study was approved by the institutional review board of Inje University Sanggye Paik Hospital (IRB no. SGPAIK 2015-06-026).
Before surgery, the type of stem (cemented or cementless) was determined according to Dorr classification of the proximal femur and cortical thickness on preoperative simple X-rays. Cementless stems were used in Dorr type A femur and cemented stems were used in Dorr type C femur. For patients with Dorr type B femur, both types of stem were used depending on patient's age and bone quality according to femoral cortical thickness16). Cortical thickness was measured based on cortical index ratio (CTI) of the proximal femur introduced by Nash and Harris17). Patient's age, medical history, and osteoporosis were considered for the selection of stem of Dorr type B femur. For patients with poor bone quality and the risk of periprosthetic fractures, cemented stems were used (cemented group, 115 patients); and for others, cementless stems were used (uncemented group, 65 patients).
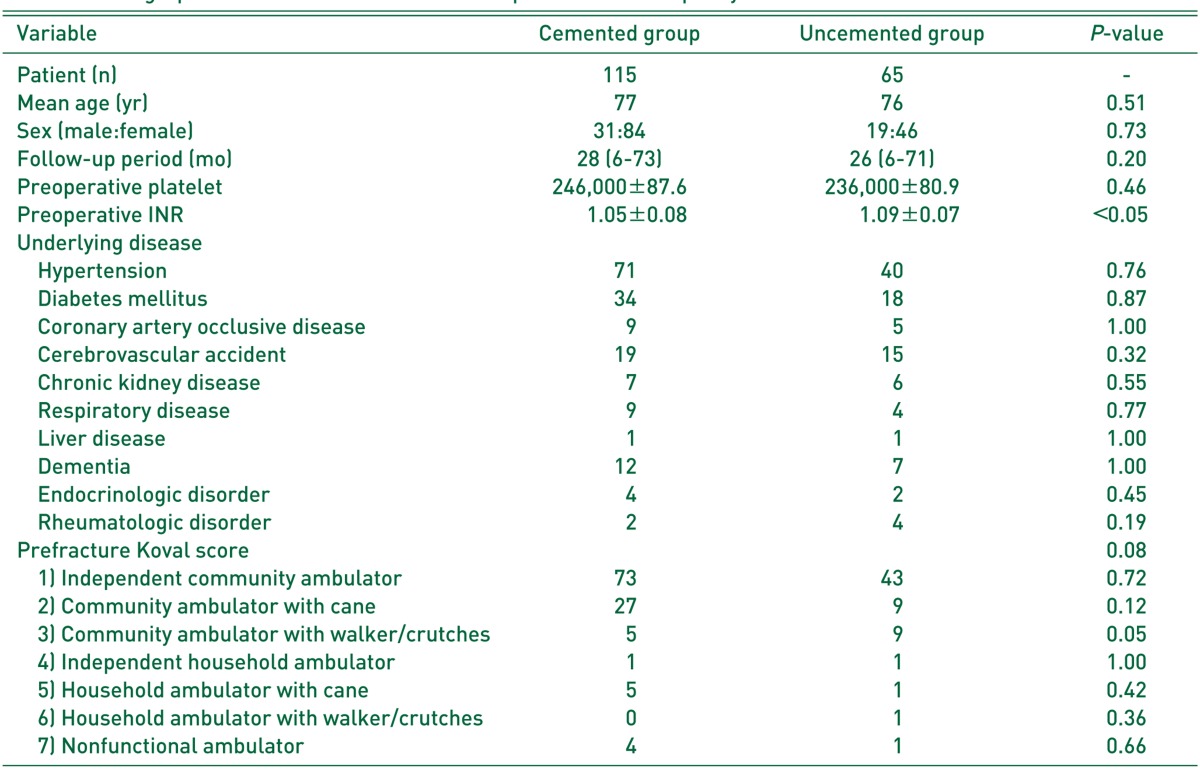
Patient's age, gender, underlying disease, duration of operation in each group, intraoperative blood loss, and postoperative drained blood volume until catheter removal were examined. Preoperative platelet count and international normalized ratio (INR) were also examined for the possible effect of these factors on intraoperative and postoperative blood loss before comparing differences between the two groups (Table 1).
The mean follow-up period was 28 months (range, 6-73 months) in the cemented group and 26 months (range, 6-71 months) in the uncemented group.
The femoral components used were standard-type femoral stems with smooth surfaces including CPT (Zimmer, Warsaw, IN, USA; 62 cases), Exeter (Howmedica, Benoist-Girard, France; 18 cases), C stem AMT (Depuy, Leeds, UK; 17 cases), IC straight stem (Implantcast, Buxtehude, Germany; 10 cases), Bencox® ID cemented (Corentec, Cheonan, Korea; 7 cases), and Logica cemented (Lima, Milano, Italy; 1 case). Bone cement (CMW3; Depuy, Warsaw, IN, USA) was used in all cases to fix femoral prosthetic components (Fig. 1).
The femoral prostheses used in cementless BHA were Tri-Lock (Depuy, Warsaw, IN, USA; 50 cases), Wagner Cone (Zimmer, Winterthur, Switzerland; 5 cases), Bencox® ID non-cemented (Corentec, Cheonan, Korea; 3 cases), Corail (Depuy J&J, Landayer, Chaumont, France; 2 cases), Summit (Depuy, Leeds, UK; 2 cases), C2 stem (Lima; 2 cases), and M/L Taper (Zimmer, Winterthur, Switzerland; 1 case) (Fig. 2).
All operations were performed by a single surgeon under spinal or general anesthesia using a modified Hardinge approach. In cementing technique, brushing and pulsatile irrigation of the femoral canal were done after intramedullary reaming and a plug was inserted into distal femoral canal. The femoral canal was filled with bone cement (Antibiotic Simplex® P; Stryker Orthopaedics, Limerick, Ireland) mixed with of vancomycin (1 g per 40 g of cement) using a cement gun.
Intraoperative blood loss was quantified by measuring saline irrigation fluid and weighing gauze used for blood collection during surgery. The postoperative volume of blood drained from the catheter was measured on a daily basis. Patients were asked to wear anti-embolism stockings on both legs to prevent pre- and post-operative deep vein thrombosis. By conducting quadriceps femoris muscle strengthening exercises immediately after surgery, closed suction drains were removed when daily drain output was less than 50 mL. Partial weight bearing was then allowed using a walker.
For clinical assessment, the difference between preinjury and post-operative ambulatory status (according to the Koval classification) and between pre-operative and last follow up visual analogue scale (VAS) scores in the groin and thigh were compared in each group. Major postoperative complications (intraoperative fractures, postoperative periprosthetic fracture, hip dislocation, pulmonary embolism, cerebral infarction, myocardial infarction, postoperative infection, pneumonia, respiratory failure, reoperation, and death) were compared between the two groups.
For radiographic evaluation, fractures and dislocations were identified based on post-operative and follow-up simple X-rays. The vertical subsidence of the femoral stem was measured on simple X-rays taken immediately after surgery and at final follow-up, and the difference between these values were compared in each group. A decrease of more than 5 mm of subsidence in the vertical distance of the femoral stem was considered to be significant18).
Student's t-test was used to compare continuous variables (age, follow-up period, operation time, intraoperative blood loss and postoperative volume of blood drained until drain removal, and preoperative platelet count and INR) between the two groups. Chi-square test was performed to compare the differences in gender, postoperative Koval walking ability and the degree of inguinal and thigh pain. Fisher's exact test was used to analyze femoral component subsidence and postoperative complications. Radiologic measurements were analyzed using Marosis M-view 5.4 (Marotech, Seoul, Korea). Statistical analyses were performed using SPSS 16.0 software (SPSS Inc., Chicago, IL, USA), and differences were considered statistically significant at P<0.05.
The two groups (i.e, cemented versus cementless femoral stems) did not differ significantly by age, gender, underlying disease and follow-up period. There was no significant difference in pre-injury Koval ambulatory status between the two groups (Table 1). Platelet counts and INR were examined preoperatively; there was no statistically significant difference in platelet count between the two groups (cemented group, 246,000±87.6; uncemented group, 236,000±80.9; P=0.16). However, INR was significantly higher in the uncemented group (cemented group, 1.05±0.08; uncemented group, 1.09±0.07; P<0.05), but INR ranged within the normal range (INR 0.80-1.20) in both groups. The duration of operation (minutes) was significantly longer in the cemented group compared to the uncemented group (cemented group, 104±17 minutes; uncemented group, 93±18 minutes; P=0.05). Despite this, no difference was found in intraoperative blood loss (cemented group, 465±151 mL; uncemented group, 472±150 mL; P=0.76), the postoperative drainage volume was significantly higher in the uncemented group (cemented group, 216±100 mL; uncemented group, 313±170 mL; P<0.05). The correlation between preoperative INR and total amount of postoperative blood loss had no statistical significance (P=0.551).
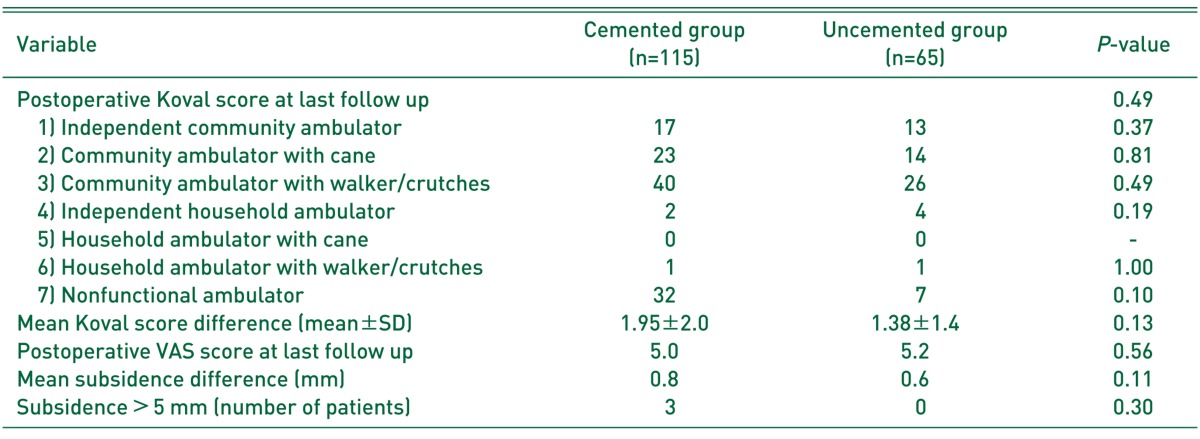
Upon clinical evaluation, changes in Koval scores indicating ambulatory status between pre- and postfracture and VAS scores indicating inguinal and thigh pain at final follow-up were not significantly different (Table 2).
Upon radiographic evaluation, the vertical subsidence of the femoral stem was measured postoperatively and at final follow-up, and there was no significant difference in the mean value of the change in vertical distance between the two groups. More than 5 mm of vertical subsidence of the femoral stem was observed in three cases (cemented group) versus none (uncemented group), a difference that was not statistically significant as determined using the Fisher's exact test (Table 2).
According to the results of chi-square test performed to test statistical difference in major postoperative complications and sub-categories between the two groups, the uncemented group had significantly higher rates of major complications. Of all complications, postoperative infection occurred in three cases in the uncemented group (P<0.05), and all of them underwent reoperation (P<0.05) (Table 3). Postoperative death occurred in two of 115 patients in the cemented group and two of 65 patients in the uncemented group. One of two patients in the cemented group had pulmonary embolism on the 12th postoperative day, and the other patient died of cardiogenic shock caused by angina pectoris on the 2nd postoperative day. One of two patients in the uncemented group expired due to pulmonary embolism occurred on the 18th postoperative day. The other patient died of septic shock, despite antibiotic therapy after removal of metal implants due to infection at the surgical site occurred on the 1st postoperative day (Table 3).
In this study, the cemented group had a longer operation time and smaller bleeding volume compared with the uncemented group. Moreover, those in the cemented group were less likely to have postoperative infection. There was no statistically significant difference in terms of postoperative inguinal and thigh pain, ambulatory ability and the vertical subsidence of the femoral stem between the two groups.
The use of a cemented femoral component in hip replacement surgery for patients with femur neck fractures is reported to be related with cardiovascular and respiratory complications (due to cement toxicity), embolisms (caused by arrhythmia), and bone marrow contents invasion to circulatory system78910111213). On the contrary, the use of a cementless femoral component is suggested to be associated with complications including thigh pain, stress shielding, periprosthetic fractures and others19). In our study, although cardiovascular and respiratory complications such as postoperative myocardial infarction or pulmonary embolism occurred in patients with cemented stems, no significant difference was found compared with the uncemented group and favorable outcome was obtained without postoperative infection. In addition, there was no significant difference in regards to ambulatory ability, inguinal and thigh pain and vertical subsidence of the femoral stem between the two groups. A meta-analysis of Li et al.20) and Luo et al.21) revealed that patients with cemented stems had better postoperative clinical outcomes and less severe thigh pain, and they had no difference in major postoperative complications compared with patients with cementless stems. Ng and Krishna22) reported that no difference was found in the incidence of major complications between the two groups; postoperative thigh pain was more severe in the uncemented group, and insignificant difference was found in ambulatory ability comparable to the result of this study. Moreover, comparable to the findings of this study, Taylor et al.23) reported no difference in postoperative thigh pain and walking ability between the two groups, and a significantly higher complication rate in the uncemented group. In contrast, a significant difference was found in subsidence rates between the two groups in the present study.
In our study, postoperative infection occurred in three patients in the uncemented group, exhibiting statistically significant difference; reoperation was performed in all cases. These cases were diagnosed by performing ultrasound-guided joint aspiration at the surgical site due to persistent postoperative fever and increased levels of inflammation markers (erythrocyte sedimentation rate, C-reactive protein level). One of these patients who was receiving hemodialysis due to diabetes mellitus (DM) and end-stage renal disease died of sepsis. Another patient was under medical treatment for stroke, and the other patient was receiving drug treatment for rheumatoid arthritis. In preoperative examination, findings indicative of inflammation related to infection were not detected in those patients. We undertook every possible effort to prevent intraoperative and postoperative complications by suspending any drug taken by the patients including anti-platelet, antithrombotic and anti-rheumatic agents prior to surgery through interdisciplinary care. Each of the three patients had no indication of inflammation in preoperative screening and no history of septic arthritis.
Parvizi et al.24) proposed multiple strategies for preventing postoperative infection following hip replacement, algorithmic approaches and treatment by reviewing several previous studies including optimization of surgical environment and patient's preoperative condition. In order to minimize infection, preoperative evaluation and management of patient's conditions should proceed through check-up and screening tests for a range of factors including DM, obesity, malnutrition, urinary tract infection, anti-rheumatic drugs, anemia, methicillin-resistant Staphylococcus aureus and others. They also suggested that infection rates can be lowered through intraoperative administration of prophylactic antibiotics, sterilization and shaving of the surgical site and use of antibiotic cement. In our hospital, we intended to prevent complications through regulation of blood glucose, nutritional supply, anemia correction, suspension of anti-platelet agents and anti-rheumatic agents and others by examining the above preoperative risk factors, but postoperative infection occurred in three cases. Of these patients, one female patient with complex diseases, in addition to DM and chronic renal failure, had past history of neurological surgery due to subarachnoid hemorrhage, dementia, antithrombotic drug use, and poor nutritional status. Although operations were performed after regulating preoperative risk factors as much as possible, she was at a high risk of getting infections by having diminished immune function due to long-term problems with blood glucose regulation (HbA1c level of 8.3 at the time of hospital admission), a body mass index of 22.9 kg/m2, chronic renal failure and others. For these reasons, the use of antibiotic-impregnated cement stems appeared to be a better choice to prevent infection. Another patient was a 79-year old male patient with no significant past medical history except for the use of antithrombotics due to past history of stroke and underwent anemia correction preoperatively. The last patient was a 69-year old female who was taking anti-rheumatic drugs including steroids, methotrexate, disease modifying anti-rheumatic drugs and others for 20 years due to rheumatoid arthritis, and she received surgery in our hospital after suspending these drugs through interdisciplinary care with the Department of Internal Medicine (Division of Rheumatology). The risk of infection in patients with inflammatory arthropathy is about two to three times higher than that of healthy individuals, and this is attributable to the effect of combined use of multiple drugs on injury healing and infection25). Nevertheless, practice guidelines for the use of drugs for minimizing infection rate and regulating postoperative inflammatory arthropathy have not yet been clearly established in patients requiring surgery. In this regard, the International Consensus Group have recently introduced practical guidelines for suspension of anti-rheumatic drugs26).
Previous studies reported a longer operation time in patients with cemented stems202227), comparable to our study, or revealed no difference in outcome after cemented versus cementless BHA728).
The difference in operation time in the present study seems to be attributable to cement manipulation time, and this may differ depending on surgeon's technical skills. Despite the difference in operation time, there was no significant difference in intraoperative blood loss volume between the two groups, while a significant difference was observed in the postoperative volume of blood drained (P<0.05). The result showing no difference in intraoperative blood loss between two groups can be interpreted that cement manipulation had insignificant influence in surgical procedure to bring changes in intraoperative blood loss under condition that patients in two groups have the same bleeding tendency, and this may also differ depending on surgeon's surgical skills. Postoperative blood loss volume was significantly greater in the uncemented group, and this outcome was comparable to the finding of Park et al.28). On the other hand, Ng and Krishna22) and Figved et al.27) reported a higher intraoperative bleeding volume in the cemented group. The authors of this study searched for literature on a hemostasis effect of cement insertion to the femoral canal, but previous studies have not yet clarified the exact mechanism and further investigation is warranted.
There are some limitations to note in the present study. This study was limited in radiologic evaluation due to a short follow-up period, ranging from 6 to 73 months (cemented group) and 6 to 71 months (uncemented group). Although the follow-up period of less than one year accounted for a relatively small proportion (14 out of 180), long-term studies are thought to be warranted. As mentioned earlier, two groups were classified based on the Dorr classification of proximal femoral morphology and cortical thickness on preoperative simple X-rays. This is considered as a limitation of our study, since this is not a completely objective method for classification due to potential interobserver error. However, we performed all operations by thoroughly confirming anatomical structure and bone quality of the proximal femur in the operating room. Cementless stems were used in Dorr type A and cemented stems were used in Dorr type C. On the contrary, selection bias may arise because cemented or cementless stems were chosen depending on patient's age and bone quality according to femoral cortical thickness in patients with Dorr type B femur. The choice of a stem was changed in some cases in the operating room after confirming different bone quality unlike our preoperative prediction. No statistically significant difference was observed in preoperative platelet count between the two groups, while the uncemented group had higher INR values than the cemented group. Even though the mean INR stayed within the normal range in both groups and no significant difference was found in the correlation between preoperative INR and bleeding volume between the two groups, these may have served as factors that have affected the results of the study. In addition, the use of different types of stems needs to be improved in the future by using the same femoral component.
In our study, there was no statistically significant difference in clinical and radiologic outcomes between the two groups undergoing cemented versus cementless BHA for treatment of femur neck fracture. Selective use of antibiotic-impregnated cemented stems in BHA may be a desirable treatment method for older patients with poor bone quality and higher risk of infection to help reduce the risk of postoperative infections.
Notes
References
1. Bhandari M, Devereaux PJ, Tornetta P 3rd, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005; 87:2122–2130. PMID: 16140828.
2. Branco JC, Felicíssimo P, Monteiro J. Epidemiology of hip fractures and its social and economic impact. A revision of severe osteoporosis current standard of care. Acta Reumatol Port. 2009; 34:475–485. PMID: 19820671.
3. Cuckler JM, Tamarapalli JR. An algorithm for the management of femoral neck fractures. Orthopedics. 1994; 17:789–792. PMID: 7800601.

4. Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop. 2011; 45:15–22. PMID: 21221218.

5. Frihagen F, Nordsletten L, Madsen JE. Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ. 2007; 335:1251–1254. PMID: 18056740.

6. Parker MJ, Gurusamy K. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006; (4):CD001708. PMID: 17054139.

7. Emery RJ, Broughton NS, Desai K, Bulstrode CJ, Thomas TL. Bipolar hemiarthroplasty for subcapital fracture of the femoral neck. A prospective randomised trial of cemented Thompson and uncemented Moore stems. J Bone Joint Surg Br. 1991; 73:322–324. PMID: 2005165.

8. Fallon KM, Fuller JG, Morley-Forster P. Fat embolization and fatal cardiac arrest during hip arthroplasty with methylmethacrylate. Can J Anaesth. 2001; 48:626–629. PMID: 11495867.

9. Foster AP, Thompson NW, Wong J, Charlwood AP. Periprosthetic femoral fractures--a comparison between cemented and uncemented hemiarthroplasties. Injury. 2005; 36:424–429. PMID: 15710161.
10. Khan RJ, MacDowell A, Crossman P, et al. Cemented or uncemented hemiarthroplasty for displaced intracapsular femoral neck fractures. Int Orthop. 2002; 26:229–232. PMID: 12185525.

11. Lennox IA, McLauchlan J. Comparing the mortality and morbidity of cemented and uncemented hemiarthroplasties. Injury. 1993; 24:185–186. PMID: 8509191.

12. Lo WH, Chen WM, Huang CK, Chen TH, Chiu FY, Chen CM. Bateman bipolar hemiarthroplasty for displaced intracapsular femoral neck fractures. Uncemented versus cemented. Clin Orthop Relat Res. 1994; (302):75–82.

13. Skyrme AD, Jeer PJ, Berry J, Lewis SG, Compson JP. Intravenous polymethyl methacrylate after cemented hemiarthroplasty of the hip. J Arthroplasty. 2001; 16:521–523. PMID: 11402421.

14. Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006; 88:2583–2589. PMID: 17142407.
15. Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006; 88:249–260. PMID: 16452734.
16. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14:231–242. PMID: 8363862.

17. Nash W, Harris A. The Dorr type and cortical thickness index of the proximal femur for predicting peri-operative complications during hemiarthroplasty. J Orthop Surg (Hong Kong). 2014; 22:92–95. PMID: 24781623.

18. Johnston RC, Fitzgerald RH Jr, Harris WH, Poss R, Müller ME, Sledge CB. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Joint Surg Am. 1990; 72:161–168. PMID: 2303502.

19. Pitto RP, Koessler M, Kuehle JW. Comparison of fixation of the femoral component without cement and fixation with use of a bone-vacuum cementing technique for the prevention of fat embolism during total hip arthroplasty. A prospective, randomized clinical trial. J Bone Joint Surg Am. 1999; 81:831–843. PMID: 10391548.

20. Li T, Zhuang Q, Weng X, Zhou L, Bian Y. Cemented versus uncemented hemiarthroplasty for femoral neck fractures in elderly patients: a meta-analysis. PLoS One. 2013; 8:e68903. PMID: 23935902.

21. Luo X, He S, Li Z, Huang D. Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg. 2012; 132:455–463. PMID: 22160512.

22. Ng ZD, Krishna L. Cemented versus cementless hemiarthroplasty for femoral neck fractures in the elderly. J Orthop Surg (Hong Kong). 2014; 22:186–189. PMID: 25163952.

23. Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012; 94:577–583. PMID: 22488613.

24. Parvizi J, Heller S, Berend KR, Della Valle CJ, Springer BD. Periprosthetic joint infection: the algorithmic approach and emerging evidence. Instr Course Lect. 2015; 64:51–60. PMID: 25745894.
25. Bongartz T, Halligan CS, Osmon DR, et al. Incidence and risk factors of prosthetic joint infection after total hip or knee replacement in patients with rheumatoid arthritis. Arthritis Rheum. 2008; 59:1713–1720. PMID: 19035425.

26. Aggarwal VK, Tischler EH, Lautenbach C, et al. Mitigation and education. J Arthroplasty. 2014; 29(2 Suppl):19–25. PMID: 24360487.

27. Figved W, Opland V, Frihagen F, Jervidalo T, Madsen JE, Nordsletten L. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res. 2009; 467:2426–2435. PMID: 19130162.

Fig. 1
(A) A 78-year-old woman with left hip pain after a fall. Left hip anteroposterior view shows transcervical femur neck fracture of Garden stage III with underlying osteoporotic change. Proximal cortical bone loss and widening of the diaphyseal canal are observed (Dorr type B). (B) She has undergone bipolar hemiarthroplasty using cemented stem (CPT stem).
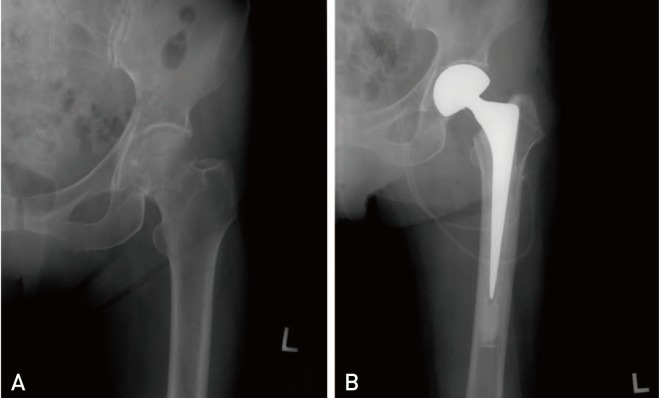
Fig. 2
(A) A 66-year-old woman with right hip pain after a fall. Right hip anteroposterior view shows transcervical femur neck fracture of Garden stage IV. Femur shaft is funnel-shaped and diaphyseal canal is narrow (Dorr type A). (B) She has undergone bipolar hemiarthroplasty using cementless stem (Tri-Lock stem).
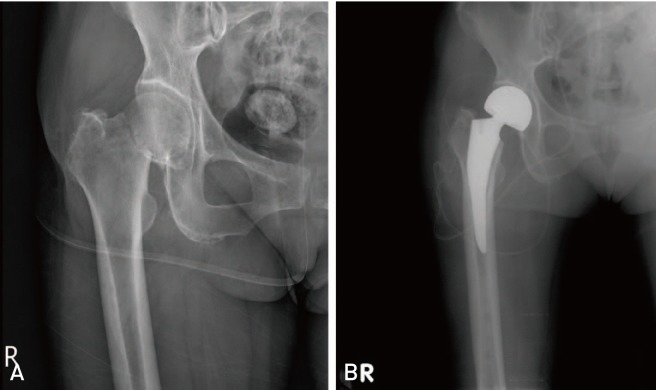
Table 3
Major Complications

*Statistically significant at Fisher's exact test.
†The patients underwent reoperation were all due to postoperative infection.
‡In cemented group, two patients expired owing to pulmonary thromboembolism and postoperative myocardiac infarction while two patients expired in uncemented group owing to pulmonary thromboembolism and postoperative infection. All patients expired in one month postoperatively.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download