Abstract
Purpose
The purpose of this study was to compare the outcomes of osteosynthesis using compression hip screw fixation versus bipolar hemiarthroplasty in AO type A2 intertrochanteric fractures.
Materials and Methods
From March 2003 to December 2009, 89 patients were included in this study. They were treated using compression hip screws (43 cases) or bipolar hemiarthroplasty (46 cases). The mean age of patients was 77.7 years (65-94 years) and the mean follow-up period was 5.9 years (1-8.3 years). For comparison of the outcomes in the two groups, statistical analyses were performed with parameters including anesthesia time, operation time, amount of transfusion, hospital stay, general complications, clinical outcome, time of partial weight-bearing using a walker, and radiological failure rate.
Results
Differences in the amount of transfusion, general complications, and clinical outcome (Merle d'Aubigné and Postel score) were not statistically significant between the two groups. The bipolar hemiarthroplasty group showed better results than the compression hip screw group for anesthesia time and the time of partial weight-bearing using a walker. Radiological failures were observed in hips in one case (2.2%) of bipolar hemiarthroplasty, and in four cases (9.3%) of compression hip screw fixation.
Conclusion
Among elderly individuals with AO type A2 intertrochanteric fractures, patients treated with bipolar hemiarthroplasty were able to perform early ambulation. However, no significant difference in operation time, amount of postoperative transfusion, clinical results, hospital stay, and radiological failure rate was observed between the bipolar hemiarthroplasty and compression hip screw fixation groups.
The prevalence of osteoporotic fractures has increased with the recent acceleration of population ageing1). In particular, trochanteric fractures of the femur are osteoporotic fractures that mainly occur in the elderly with systemic problems, and are often treated surgically to prevent prolonged bed-ridden state caused by functional problems, such as hip joint pain, and the risk of complications2,3). Although the surgeries used to treat trochanteric fractures of the femur, namely compression hip screw (CHS) fixation, intramedullary nailing, and bipolar hemiarthroplasty (BHA), result in successful treatment of stable fractures, they need to be carefully chosen for patients with unstable fractures due to the difficulties in reduction, maintenance, and early acquisition of stability4,5). Compression hip screw fixation is widely used and has an advantage of facilitating bone reduction through compressive force induced by sliding of the compression screw6,7), but fixation failures have been reported such as perforation of the femoral head and excessive sliding of the screw8). Meanwhile, BHA is increasingly used because of its advantage of enabling early ambulation. However, this surgical method is associated with some problems, including difficulty in achieving early stability of the femoral stem due to posteromedial bone fragments causing instability, implant dissociation, infection, dislocation, subsidence of the femoral stem, and difficulty in surgical manipulation9,10,11). Although several authors have reported the clinical results of CHS fixation and BHA in elderly individuals with unstable intertrochanteric fractures of the hip4,5,10,12,13,14), there has been no comparative studies of these surgeries in AO type A2 intertrochanteric fractures. Therefore, we aimed to verify the hypothesis that there is no difference in clinical and radiological results between CHS fixation and BHA by retrospective analysis of outcomes of respective treatments in patients with AO type A2 intertrochanteric fractures.
This study included 109 patients aged over 65 years, who received surgical management from March 2003 to December 2009 due to AO type A2 intertrochanteric fractures. We excluded 20 patients who were followed up for less than 1 year, and retrospectively examined a total of 89 cases (16 men and 73 women). Of these, 43 received CHS fixation, while 46 received BHA. The mean age was 77.7 years (range, 65-94 years), and the mean follow-up period was 5.9 years (range, 1-8.3 years). The mean body mass index (BMI) was 22.2 kg/m2 (range, 15.4-31.6 kg/m2).
Operations were performed by a single surgeon (YHK). BHA was performed when severe osteoporosis or poor bone quality was anticipated on the basis of radiography in patients with substantial loss in trabecular bone mass in the proximal femur, or when reoperation was impossible due to the patient's systemic state. In all other cases, CHS fixation was performed. The prosthetic components used were CHS (Synthes-Stratec, Oberdorf, Switzerland) in all CHS fixation patients, and cementless femoral stems in all BHA patients: SL-PLUS (Smith & Nephew, Memphis, TN, USA; 41 cases), Versys (Zimmer, Warsaw, IN, USA; 3 cases), and ABG II (Stryker, Newbury, UK; 2 cases).
In CHS fixation patients, closed reduction under image intensifier was performed on the fracture table after anesthesia. When satisfactory anatomical reduction was achieved, a CHS was fixed through a lateral approach. In case of anatomical reduction failure, fixation was performed using a CHS and adjuvant devices such as a bone hook or a Lowman clamp by requiring greater exposure of the fracture site. Severely displaced and unstable lesser trochanter fragments were additionally fixed using cerclage wire. In BHA, the fracture site was exposed using a posterolateral approach, and then femoral neck resection was performed directly under the femoral head. After the reduction of lesser trochanter fragments, fixation was attempted in the calcar femorale and posterior lesser trochanter by firmly tightening 2 or 3 metal cerclage wires. The femoral stem component was inserted into the femur after rasping the femoral canal, and then 1 or 2 metal cerclage wires were additionally used to fix greater trochanter fragments. For postoperative rehabilitation, quadriceps-strengthening exercises and passive exercises of the hip and knee joints were carried out. From the seventh postoperative day, patients were allowed partial weight-bearing using a walker.
To evaluate the clinical outcome, we examined the Merle d'Aubigné-Postel score15) to assess pain and function, anesthesia time, operation time, the amount of postoperative transfusion, hospital stay, the starting time of partial weight-bearing, and systemic complications. Anesthesia time (based on the anesthesia records) was defined as the period from admission into the operating room to completion of operation, and the operation time was defined as the period from the incision to completion. The transfusion volume was defined as the number of packed blood units used from incision to discharge from the hospital. Hospital stay was defined as the period from the operation to discharge day. The time of partial weight-bearing was reviewed in the medical records. Radiological results were analyzed based on the pre-, post-operative and final follow-up radiographs (anterior-posterior and lateral) of the hip joint. To assess the failure rate, failures were defined as non-union, perforation, and sliding of >15 mm in the CHS group16), and dislocation, osteolysis around the femoral stem, and subsidence by >5 mm in the BHA group17). To identify systemic complications, we examined complications in the respiratory, circulatory, renal, urinary and gastrointestinal systems, and wound-related complications that occurred within 3 postoperative months.
Statistical analysis was performed using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). We used the Wilcoxon rank-sum test for continuous variables and Fisher's exact test for categorical variables. P-values of <0.05 were considered statistically significant.
There was no significant difference between the two groups in the demographic variables, which included the sex ratio, BMI, follow-up period, the number of associated diseases, and AO classification. The mean age was 75.5±6.4 years in the CHS group and 79.7±6.5 years in the BHA group. Patients were older in the BHA group. Bone mineral density was examined in 25 out of 89 patients. Of these, 20 were treated with BHA and 5 were treated with CHS fixation. The average T-score was -2.6±1.0 in the CHS group and -3.0±0.8 in the BHA group. The score was more favorable in the CHS group, but showed no statistically significant difference between the two groups (Table 1).
The amount of transfusion, general complications, and the Merle d'Aubigne and Postel score were not significantly different between the two groups. According to the Merle d'Aubigné-Postel score, pain, function, ambulation ability and the total score were similar in the two groups. Anesthesia time was 2.3±0.9 h in the CHS group and 1.5±0.7 h in the BHA group. Although a significantly longer anesthesia time was found in the CHS group (P<0.001), no significant difference in operation time was found. No difference between the two groups was observed in the amount of postoperative transfusion. The mean hospital stay was also similar (27.5±3.3 days in the CHS group and 26.5±2.7 days in the BHA group). The average time of starting partial weight-bearing using a walker was 22.8±7.2 days in the CHS group, and 13.6±7.0 days in the BHA group. Patients in the BHA group were able to begin partial weight-bearing earlier (P<0.001) (Fig. 1, 2).
Radiological findings revealed the failure rate of 9.3% (4 cases) in the CHS group and 2.2% (1 case) in the BHA group. Excessive sliding of the lag screw was detected in all cases of failure in the CHS group; in one of them, loosening of the lag screw was detected (Fig. 3, Table 2). In the failed case in the BHA group, damaged wire and non-union were observed and excessive subsidence of the femoral stem was detected (Fig. 4).
Postoperative systemic complications occurred in 25 cases (58%) in the CHS group, including pulmonary thromboembolism in 1 case, pneumonia in 1 case, wound complication in 1 case, urinary tract infection in 7 cases, acute kidney injury in 1 case, sores in 2 cases, electrolyte imbalance in 3 cases, pseudomembranous colitis in 2 cases, and delirium in 7 cases. Postoperative systemic complications occurred in 24 cases (52%) in the BHA group, including pulmonary congestion in 1 case, pulmonary thromboembolism in 2 cases, pneumonia in 3 cases, urinary tract infection in 6 cases, sores in 3 cases, electrolyte imbalance in 2 cases, and delirium in 7 cases. No significant difference was observed in the incidence of complications between the two groups (P=0.671; Table 3).
Postoperative care focuses on encouraging early ambulation of patients with intertrochanteric fractures to prevent complications caused by prolonged bed-ridden state3). For this reason, accurate anatomic reduction and stable internal fixation are essential, and several surgical methods have been implemented for this purpose18). There is no doubt that CHS fixation is an effective treatment for stable fractures, which has an advantage of bone union by reduction of the moment arm through controlled sliding of the lag screw. However, Hwang et al.19) and Kim et al.5) reported a high failure rate of surgery with the use of CHS, and unstable fracture type and severe osteoporosis were commonly detected in failed cases. In our study, radiological failure rate was 9.3% in the CHS group. The relatively low failure rate is likely due to the inclusion of only type A2 in our study, unlike previous studies that included type A3. The risk factors for CHS fixation failure are the reduction of the fracture, CHS location, and the presence of osteoporosis. In our study, 4 CHS fixation cases showed failure of anatomical reduction. The primary goal of fracture fixation is anatomical reduction and maintaining the continuity of the medial cortex of the fractured fragment, as assessed from anterior-posterior radiographs. The continuity of the medial cortex is important in resistance to the force of varus and posterior displacement20).
In BHA, partial weight-bearing can be initiated early. For this reason, BHA is increasingly used to treat intertrochanteric fractures in patients with severe osteoporosis. Kim et al.9) suggested that a rise in the use of BHA in intertrochanteric fractures over 4 years from 6% to 9% resulted from an increase in unstable fractures and osteoporosis with age. To overcome the instability caused by posteromedial bone fragments, Kim et al.21) used a calcar replacement stem, Jones22) introduced screw fixation of the lesser trochanter, and Lee et al.23) fixed the lesser and greater trochanters through band wiring. These studies reported favorable outcomes. In our study, stability of the fragment can be achieved by its fixation on the lesser trochanter using 2-4 wires; with this approach, failures were not detected except for subsidence of the femoral stem by >5 mm in one case (2.2%).
Park et al.24) found no difference in the bleeding volume and operation time between CHS fixation and cemented BHA. BHA showed better clinical results and reduced the incidence of complications. In our study, there was no difference in transfusion volume between the two groups. However, the CHS group showed longer anesthesia time, which was probably attributable to a longer time needed for preoperative bone reduction.
In most cases, the time of weight-bearing is determined by the surgeon. However, despite the surgeon's instructions, the actual starting time of weight-bearing seems to be different depending on the patient's systemic state, compliance, and tendency. Therefore, we allowed patients to freely perform postoperative weight-bearing and analyzed the actual starting time of weight-bearing as clinical results.
Early stability can be achieved by using a cementless implant, and early ambulation can be initiated by stable fixation of the lesser and greater trochanters. In a study by Kayali et al.12), full weight-bearing was initiated by the fourth postoperative week (on average) in elderly patients who underwent arthroplasty using a cementless implant due to an unstable intertrochanteric fracture. This starting time was significantly earlier than that of patients with internal fixation. In the present study, patients were able to start partial weight-bearing using a walker at an average of 13.6 postoperative days. Furthermore, ambulation was earlier in the BHA group than in the CHS group patients, who started weight-bearing at an average of 22.8 postoperative days. These findings imply that BHA is more favorable for early ambulation and rehabilitation in patients with intertrochanteric fractures in comparison with CHS fixation.
Our study has some limitations. First, the follow-up period was short, and we retrospectively investigated a relatively small number of patients. Second, we recognize that a limitation of this study is the starting time of weightbearing, which may have been affected by surgeons' instructions. Since there may be individual differences depending on the patients' muscular strength, the degree of postoperative recovery, and implant stability, we reviewed the actual starting time of weight-bearing to minimize the effect of surgeons' intervention. Third, this study was limited to patients classified as AO type A2 to minimize the difficulties in interpreting a large number of individual variables. Moreover, surgery was performed by a single surgeon to prevent potential errors due to the differences in surgeons' preference and experience.
Among elderly individuals with AO type A2 intertrochanteric fractures, patients treated with BHA were able to perform earlier ambulation than patients treated with compression hip screw fixation. However, there was no significant difference in operation time, the amount of postoperative transfusion, clinical results, hospital stay and radiological failure rate between the BHA and compression hip screw fixation groups.
Figures and Tables
Fig. 1
(A) A 85 years old woman patient had AO type A2 intertrochanteric fracture. (B) The postoperative radiograph shows appropriate reduction and fixation with compression hip screw. (C) The radiograph at 16 months after fixation shows complete healing of fracture.

Fig. 2
(A) A 77 years old woman patient had A2 type intertrochanteric fracture. (B) The immediate postoperative radiograph shows bipolar arthroplasty state. (C) The radiograph at 5 years after surgery shows stable fixation without complication.
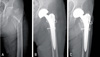
Fig. 3
(A) A 68 years old woman patient had A2 type intertrochanteric fracture. (B) The postoperative radiograph shows stable fixation with compression hip screw. (C) At 1.5 years after surgery, radiograph shows femoral head perforation and excessive sliding.

Fig. 4
(A) A 71 years old woman patient had A2 type intertrochanteric fracture. (B) The postoperative radiograph shows bipolar arthoplasty and wiring. (C) The radiograph at 2 years after surgery shows excessive subsidence of femoral stem.

References
1. Kim YS, Kim YH, Hwang KT, Choi IY. Isolated acetabular revision hip arthroplasty with the use of uncemented cup. J Arthroplasty. 2009; 24:1236–1240.

2. Kang HY, Yang KH, Kim YN, et al. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010; 10:230.

3. Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003; 17:53–56.

4. Nordin S, Zulkifli O, Faisham WI. Mechanical failure of Dynamic Hip Screw (DHS) fixation in intertrochanteric fracture of the femur. Med J Malaysia. 2001; 56:Suppl D. 12–17.
5. Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001; 25:360–362.

6. Bendo JA, Weiner LS, Strauss E, Yang E. Collapse of intertrochanteric hip fractures fixed with sliding screws. Orthop Rev. 1994; Suppl. 30–37.
7. Flores LA, Harrington IJ, Heller M. The stability of intertrochanteric fractures treated with a sliding screw-plate. J Bone Joint Surg Br. 1990; 72:37–40.

8. Rha JD, Kim YH, Yoon SI, Park TS, Lee MH. Factors affecting sliding of the lag screw in intertrochanteric fractures. Int Orthop. 1993; 17:320–324.

9. Kim DH, Lee SH, Ha SH, You JW. Changes in patient pattern and operation methods for intertrochanteric fractures. J Korean Orthop Assoc. 2011; 46:49–53.

10. Haentjens P, Casteleyn PP, De Boeck H, Handelberg F, Opdecam P. Treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Primary bipolar arthroplasty compared with internal fixation. J Bone Joint Surg Am. 1989; 71:1214–1225.

11. Hwang DS, Jung HT, Kim SB, Kim JS. Recovery of walking ability after operation for unstable intertrochanteric fractures of the femur in elderly. -timing on weight bearing-. J Korean Soc Fract. 1998; 11:296–303.

12. Kayali C, Agus H, Ozluk S, Sanli C. Treatment for unstable intertrochanteric fractures in elderly patients: internal fixation versus cone hemiarthroplasty. J Orthop Surg (Hong Kong). 2006; 14:240–244.

13. Grimsrud C, Monzon RJ, Richman J, Ries MD. Cemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures. J Arthroplasty. 2005; 20:337–343.

14. Haentjens P, Casteleyn PP, Opdecam P. Primary bipolar arthroplasty or total hip arthroplasty for the treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Acta Orthop Belg. 1994; 60:Suppl 1. 124–128.
15. Merle D'Aubigné R. Numerical classification of the function of the hip. 1970. Rev Chir Orthop Reparatrice Appar Mot. 1990; 76:371–374.
16. Baixauli F, Vicent V, Baixauli E, et al. A reinforced rigid fixation device for unstable intertrochanteric fractures. Clin Orthop Relat Res. 1999; (361):205–215.

17. Hwang D, Kwak S, Woo S. Results of cementless hemiarthroplasty for elderly patients with unstable intertrochanteric fractures. J Korean Hip Soc. 2004; 16:386–391.
18. Kaplan K, Miyamoto R, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. J Am Acad Orthop Surg. 2008; 16:665–673.

19. Hwang D, Lee C, Hong C, Kim K, Joo Y. Operative treatment for the unstable femur intertrochanteric fracture in the elderly. J Korean Hip Soc. 2005; 17:156–163.
20. Jensen JS, Sonne-Holm S, Tøndevold E. Unstable trochanteric fractures. A comparative analysis of four methods of internal fixation. Acta Orthop Scand. 1980; 51:949–962.

21. Kim SY, Kim YG, Hwang JK. Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures. A prospective, randomized study. J Bone Joint Surg Am. 2005; 87:2186–2192.
22. Jones JB. Screw fixation of the lesser trochanteric fragment. Clin Orthop Relat Res. 1977; (123):107.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download