Introduction
The incidence of gastric cancer has gradually been declining worldwide. However, gastric cancer has exhibited the highest prevalence rate in Korea, and it ranks as one of the leading causes of cancer death, followed by lung cancer.(
1,
2) In recent years, early cancer detection in many cases is gradually increasing due to diagnosis technology advancement and frequent checkups. Moreover, a 5-year survival rate of gastric cancer has been showing an increasing trend.(
3,
4) Due to the advancement of endoscopic and laparoscopic surgery, the quality of life is improving and complications of surgery are reduced.(
5) However, advanced gastric cancer (AGC) is still frequently detected,(
6,
7) and a 5-year survival rate of AGC is not promising despite curative gastrectomy.(
8)
Clinico-pathologic characteristics affecting the prognosis of gastric cancer are depth of tumor invasion, nodal status, distant metastasis, macroscopic types of tumor, tumor size, histologic type and others.(
3)
Tumor size belongs to the category of factors for determining stages of cancers including breast cancer, lung cancer, pancreatic cancer, and others.(
9) Thus, stages are determined according to the sizes of tumor, and therapeutic treatments vary depending on the size. However, few studies have analyzed the effect of tumor size on the prognosis of gastric cancer. Hence, the authors of this study investigated the effect of tumor size on the prognosis of gastric cancer.
Materials and Methods
This study conducted a retrospective analysis on 1,697 patients who underwent curative surgery among the total of 1,897 patients who received gastrectomy after a diagnosis with gastric cancer in the Department of Surgery of Hanyang University Medical Center, from June 1992 to August 2009. The curative surgery was defined as a surgery which was performed on M0 patients who underwent lymph node dissection with more than 16 dissected nodes without any distant metastasis. In case of adjacent organ invasion of T4b (7th American Joint Committee on Cancer [AJCC] staging system),(
10) combined resection of invaded organs was carried out, and the resection margin must be negative. Study population comprised of 720 early gastric cancer (EGC) patients and 977 AGC patients. The median follow-up period was 50 months until August 31, 2011. The follow-up rate was 97.0% (1,897/1,955). Tumor sizes ranged 0.3~15.0 cm (median=3 cm, mean±standard deviation [SD]=3.2±2.1 cm) in case of EGC and 1.0~20.0 cm (median=6 cm, mean±SD=6.4±3.0 cm) in case of AGC. By taking the median tumor size as the standard, the study defined tumors less than 3 cm in size as small tumors and those that are more than 3 cm in size as large tumors in EGC. Meanwhile, tumors less than 6 cm in size were set as small tumors and more than 6 cm as large tumors in AGC.
To analyze the survival rate in each group, univariate and multivariate analyses were conducted on patient's factors (age, sex), tumor factors (depth of invasion, nodal status, tumor size, tumor site, histologic type, lymphatic invasion, venous invasion, perineural invasion), and treatment factors (type of surgery).
PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis. Kaplan-Meier survival analysis was performed for univariate analysis of the survival rate, while Cox regression analysis was performed for multivariate analysis. A P-value of less than 0.05 was considered statistically significant.
Discussion
Tumor size can be determined quite easily in the preoperative exam and the accuracy of information is fairly reliable. In recent years, tumor size has been continuously pointed out as one of the critical factors determining the prognosis in gastric cancer. Hence, the necessity of study has lately been underscored as a crucial issue.
Establishing the standard of tumor size is a considerably critical issue in categorizing gastric cancers based on the tumor size. Previous studies classified tumors based on their own standards. When Adachi et al.(
11) categorized patients' tumor sizes by 2 cm, relatively significant survival rate was observed between tumors with 4 cm and 10 cm in size. Subsequently, they categorized patients into 3 groups; with tumors less than 4 cm, in between 4 cm to 10 cm, and larger than 10 cm. Giuliani et al.(
12) classified patients into three groups with sizes less than 26 mm, in between 26~50 mm, and more than 50 mm, based on the survival rate. Li et al.(
13) took 10 cm or above as the standard by setting the standard at 90% depending on patient distribution. Saito et al.(
14) took the most statistically significant result as the standard in terms of disease-specific survival when they set the standard as 8 cm in the study using the Cox proportional hazard model to find the critical point. Liu et al.(
15) took 6 cm as the standard by calculating the mean of the tumor sizes in the study on the tumor size of T3 gastric cancer. This study calculated the median by classifying gastric cancers into EGC and AGC with tumor sizes of 3 cm and 6 cm, respectively. Using medians are thought to be valid to exclude statistic errors in tumor size and establish objective standards. However, this issue needs to be further discussed since there is no definite basis regarding the tumor size.
The significance of tumor size can be viewed from two aspects. First, the frequency of endoscopic and laparoscopic surgery has lately been surged in case of EGC. However, its indication has not yet been established. Independent factors are the tumor size, lymphatic invasion and submucosal invasion according to the multivariate analysis on lymph node metastasis in EGC.(
16) Thus, Maehara et al.(
16) asserted that tumor size is a reliable predictor in examining the tumor behavior in EGC. On the other hand, Tsujitani et al.(
17) did not consider the tumor size as an independent prognostic factor. They reported that tumor size and macroscopic appearance are the most reliable factors in determining the indication of endoscopic mucosal resection since the predictability of preoperative depth of tumor invasion is inaccurate and determining nodal status is unreliable. In case of EGC, the tumor size does not belong to an independent prognostic factor in this study. Second, the tumor size is a crucial factor in the evaluation of the prognosis. A previous study reported that tumor size is more significant prognostic factor than depth of invasion in gastric cancers without serosal invasion and lymph node metastasis.(
18) However, the tumor size does not fall under one of the factors determining the different stages in gastric cancer.(
19,
20) Hence, further studies on the effects and prognosis depending on the tumor size are essential by analyzing the characteristics of gastric cancer, based on detailed clinicopathologic classifications. This study analyzed the relationship between tumor size and prognosis in all patients with AGC. Although a poor prognosis was assessed in case of large tumors, this study reclassified and reanalyzed AGC, according to the depth of tumor invasion, one of the main factors determining the prognosis of gastric cancer. A statistically significant difference (P<0.0001) was shown in the prognosis depending on the depth of tumor invasion of AGC (T2, T3, T4a, T4b). A meaningful difference was observed in the survival rate (P<0.0001) (
Table 4), when each survival rate was examined by classifying AGC, according to serosal invasion (T2, T3 vs. T4a, T4b). This study further investigated on the relationship between the tumor size and prognosis by a depth of tumor invasion in AGC. Moreover, this study analyzed the prognostic significance of tumor size in each group by dividing AGC into 2 groups, based on the presence of serosal invasion by considering an adequate number of the cases. As a result, the tumor size was an independent factor affecting in the prognosis of both groups, regardless of differences in the depth of tumor invasion.
The clinical characteristics of tumor size have not yet been adequately clarified in terms of large gastric cancers. However, large tumor size is profoundly associated with Borrmann type IV, adjacent organ invasion (T4) and higher lymph node and distant metastasis rate.(
21,
22) For this reason, most patients have stage III or stage IV cancers, low possibility of radical resection in many cases, and lower 5-year survival rate.(
23) Likewise, clinico-pathologic characteristics vary depending on the tumor size, and distinct differences are present in the survival rate. Therefore, utilizing a standardized tumor size could be substantially meaningful in arranging the treatment during the postoperative follow-up period by analyzing the evaluation factors of prognosis of cancers.
Adachi et al.(
11) categorized patients into 3 groups- with tumors less than 4 cm, in between 4 cm to 10 cm, and larger than 10 cm in size- and compared the 10-year survival rate of the 3 groups. The survival rates were 92%, 66%, and 33%, respectively, exhibiting the statistically significant difference. The tumor size was an independent prognostic factor along with T and N according to multivariate analysis. Therefore, they reported that tumor size is a simple predictor in the progress of tumor and survival of patients. Saito et al.(
14) compared the 5-year survival rate in 2 groups with tumors less than 8 cm and more than 8 cm in size. The survival rates were 89.7% and 54%, respectively, showing a statistically significant difference. Moreover, they reported that tumor size is an independent prognostic factor along with T and N factors and lymphatic invasion, according to the multivariate analysis. Jun et al.(
24) compared the 5-year survival rates of 2 groups with tumors below and above 3.5 cm. The survival rates were 86.8% and 62%, respectively, showing a statistically significant difference. In addition, the tumor size was reported to be an independent prognostic factor through multivariate analysis. Liu et al.(
15) also reported that the tumor size is an independent prognostic factor by taking 6 cm, the standard in the multivariate analysis. A significant difference was found in the prognosis depending on the tumor size, especially in stages IIIb and IV.
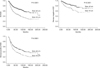
In this study, no difference was present in the survival rates by using the median value of 3 cm for the tumor size as the standard in case of EGC. However, when the median value of 6 cm in AGC was used as the standard, significant differences of 71.0% and 48.5% (P<0.0001) were observed, respectively. Moreover, the 5-year survival rates were 86.6% vs. 72.8% (P<0.0001) and 54.2% vs. 38.3% (P<0.0001) in serosa negative group and positive group, respectively, exhibiting a statistically significant difference in both groups. Tumor size was an independent prognostic factor in AGC, along with the patient's age, depth of tumor invasion, nodal status, and venous invasion. Therefore, the tumor size is thought to be a simple but significant factor in the evaluation of the prognosis.
To investigate the effect of tumor size on the prognosis of gastric cancer patients, this study examined 1,697 patients who underwent curative surgery. The study defined tumors less than 3 cm as small tumors, and those that are more than 3 cm as large tumors, in 720 EGC patients. Meanwhile, tumors less than 6 cm in size were set as small tumors, while more than 6 cm as large tumors, in 977 AGC patients. The study has acquired the following results.
Tumor size was an independent prognostic factor in AGC, unlike in EGC. Independent prognostic factors in EGC were age and histologic type. A statistically significant difference was observed in the survival rate, based on tumor size in AGC. Tumor size in AGC was an independent prognostic factor. Furthermore, it was an independent prognostic factor in the result of analysis carried out based on the presence of serosal invasion.






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download