Abstract
Purpose
Emergency operations for perforated peptic ulcer are associated with a high incidence of postoperative complications. While several studies have investigated the impact of perioperative risk factors and underlying diseases on the postoperative morbidity after abdominal surgery, only a few have analyzed their role in perforated peptic ulcer disease. The purpose of this study was to determine any possible associations between postoperative morbidity and comorbid disease or perioperative risk factors in perforated peptic ulcer.
Materials and Methods
In total, 142 consecutive patients, who underwent surgery for perforated peptic ulcer, at a single institution, between January 2005 and October 2010 were included in this study. The clinical data concerning the patient characteristics, operative methods, and complications were collected retrospectively.
Results
The postoperative morbidity rate associated with perforated peptic ulcer operations was 36.6% (52/142). Univariate analysis revealed that a long operating time, the open surgical method, age (≥60), sex (female), high American Society of Anesthesiologists (ASA) score and presence of preoperative shock were significant perioperative risk factors for postoperative morbidity. Significant comorbid risk factors included hypertension, diabetes mellitus and pulmonary disease. Multivariate analysis revealed a long operating time, the open surgical method, high ASA score and the presence of preoperative shock were all independent risk factors for the postoperative morbidity in perforated peptic ulcer.
The development of anti-secretory medications, including H2-blockers and proton pump inhibitors, together with the realization that peptic ulceration is an infectious disease whose causative agent, Helicobacter pylori, can be eliminated by anti-bacterial regimens, means that there is now a high probability of curing peptic ulcer disease and preventing its recurrence. As a result, there has been a marked decrease in the number of patients with uncomplicated peptic ulcers who have undergone elective surgery, and globally, the incidence of peptic ulcer disease has fallen in recent years.(1) However, the number of patients admitted for emergency surgery after peptic ulcer perforation has not undergone a similar decline, and peptic ulcer perforation remain a substantial healthcare problem.(1-4)
Emergency surgery for perforated peptic ulcer is associated with a high rate of postoperative complications (between 21% and 43%).(5,6) Several studies have investigated perioperative risk factors for postoperative morbidity in abdominal surgery. Bittner et al.(7) reported that underlying diseases are a major risk factors for postoperative morbidity, while Habu and Endo(8) revealed that a prolonged operating time and excessive blood loss were significantly associated with morbidity after surgery for gastric cancer in elderly patients. At present, little is known about the relationship between perioperative risk factors and postoperative morbidity for perforated peptic ulcer. The aim of this study was to investigate the contribution of perioperative risk factors and comorbid diseases to morbidity following peptic ulcer perforation surgery.
A retrospective study was performed with 143 patients with perforated peptic ulcer who underwent surgery at a single center between January, 2005 and October, 2010. Data concerning the sex, age, and the underlying diseases of the patients together with the location of the lesion(s), The American Society of Anesthesiologists (ASA) score, preoperative shock status at admission, interval between ulcer perforation and operation, operative method, operating time, and postoperative complications were collected.
One patient was excluded because the final pathological report revealed that he had gastric cancer.
Preoperative shock status was defined as persistent hypotension (systolic blood pressure <90 mmHg, mean arterial pressure <60 mmHg, or a reduction in systolic blood pressure >40 mmHg from baseline).
The following definitions were used to assess the complications:(9)
(1) leakage, defined as a dehiscence confirmed by contrast radiography; (2) fluid collection, defined as the presence of septic fluid in the abdominal cavity that resulted in a pyrexia of 38℃ and was confirmed by ultrasonography or computed tomography (CT); (3) intestinal obstruction, defined as a mechanical obstruction with an air-fluid level and the obstruction site being apparent during CT; (4) paralytic ileus, defined as the postoperative absence of bowel motility, as demonstrated by gaseous distension without an air-fluid level on a plain radiograph; (5) postoperative bleeding, defined as a condition requiring transfusion and confirmed by gastrofiberoscopy or intervention procedures; (6) wound problem, defined as the presence of serous fluid or pus at the incision site that led to delayed suture removal or wound resuturing; (7) pulmonary complication, defined as the presence of atelectasis, pleural effusion, empyema, pneumonia, or pneumothorax on plain chest radiograph or CT scan; (8) cardiac complication, defined as the postoperative presence of a symptom, a laboratory test result, and an electrocardiogram that are indicative of myocardial infarction, angina, or arrhythmia; (9) renal complication, defined as the presence of symptoms or laboratory blood test results that are indicative of acute renal failure; (10) hepatic complication, defined as the presence of symptoms or abnormal laboratory blood test results that require medication; (11) urological complication, defined as the presence of postoperative infection of the urinary tract, or absence of self voiding.
The underlying diseases of the patients were defined as follows:(9)
(1) Hypertension: patients diagnosed with hypertension by physicians were classified into two groups; those with controlled hypertension and those with uncontrolled hypertension.
(2) Heart disease: patients diagnosed with heart disease by a cardiologist were classified into two groups; those with severe heart disease (such as coronary vessel disease, congestive heart failure) and those with mild heart disease (such as atrial fibrillation with a normal ventricular rate).
(3) Chronic liver disease: patients diagnosed with liver cirrhosis by physicians with or without radiological confirmation, and patients diagnosed with chronic viral hepatitis on the basis of laboratory tests for the hepatitis A, B, and C viruses were classified into two groups; those with severe liver disease (such as liver cirrhosis with Child-Pugh class B, C) and those with mild liver disease (such as chronic viral hepatitis carrier, liver cirrhosis with Child-Pugh class A).
(4) Pulmonary disease: patients requiring perioperative management on the basis of previous abnormal pulmonary function tests, and patients with abnormal plain chest radiographs or CT scans.
(5) Tuberculosis: patients currently being prescribed antituberculosis medication or patients with a history of antituberculosis medication were classified into two groups; those with a presence of activity of tuberculosis and those with a complete recovery.
(6) Diabetes mellitus: patients diagnosed with diabetes mellitus and managed with oral hypoglycemic agents or insulin were classified into two groups; those with controlled diabetes and those with uncontrolled diabetes.
(7) Endocrine disease: patients with an established diagnosis of thyroid or adrenal disease.
(8) Neurological disease: patients diagnosed with neurological disease and receiving medication from our center or another clinic were classified into two groups; those with severe neurologic disease (such as stroke) and those with mild neurologic disease (such as spinal fracture without cord injury).
The operative procedures were done as follows:
(1) Primary repair with an omental patch: a simple suture was performed at the site of perforation, a strand of well-vascularized omentum was placed directly onto the perforation, and the sutures were knotted above the omentum.
(2) Truncal vagotomy with pyloroplasty: truncal vagotomy was performed by dividing the left and right vagus nerves above the hepatic and celiac branches and just above the gastroesophageal junction, by using ultrasonic shear or electrocauterization. Pyloroplasty was performed by open gastroduodenal junction, transversely, then close the opening site perpendicularly.
(3) Antrectomy and gastrojejunostomy: antrectomy was performed by ligating of the vessel that provides the gastric antrum (right gastic, right gastroepiploic), and dividing the duodenum just distal to the pylorus. The duodenum was closed by using a stapler, after which gastrojejunostomy was done by manually or by using a stapler.
(4) Primary repair with highly selective vagotomy: a simple suture was done at the site of perforation, and divided only the vagus nerves supplying the acid-producing portion of the stomach within corpus and fundus by using ultrasonic shear or electrocauterization. The vagal innervations of the gastric antrum were preserved.
The relationships between several factors and postoperative complications were analyzed using the chi-square test. A P-value<0.05 was considered to be statistically significant. A binary and multinomial logistic regression model was used for the univariate and multivariate analyses. SPSS version 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyses.
A total of 142 patients presented with perforated peptic ulcers. Of these, 108 were males (76.1%) and 34 were females (23.9%). Their mean age was 56.5 (15~88) years. Of the 142 patients, 3 (2.1%) had an ASA score of 1, 112 (78.9%) an ASA score of 2, 25 (17.6) an ASA score of 3, and 2 (1.4%) an ASA score of 4. There were 20 cases with preoperative shock status (14.1%). 68 patients (47.9%) underwent an operation within 24 hours of ulcer perforation, and 74 patients (52.1%) underwent an operation 24 hours after ulcer perforation (Table 1). Of the 142 patients, 97 (68.3%) and 45 (31.7%) had perforated gastric and duodenal ulcers, respectively. Open surgical approach was performed in 102 cases (71.8%) and laparoscopic approach was performed in 40 cases (28.2%). Primary repair, the most common method, was performed in 88 cases (62.0%). The other operations were truncal vagotomy and pyloroplasty (26 cases, 18.3%), antrectomy and gastrojejunostomy (26 cases, 18.3%), and primary repair with highly selective vagotomy (two cases, 1.4%). Combined organ resection was performed in 7 cases (4.9%). Five cases were subjected to cholecystectomy because gall bladder stone was present, 1 case was subjected to appendectomy because acute appendicitis was detected, and 1 case was subhected to hernia sac resection because right inguinal hernia was present. The mean operating time was 149.6 minutes (Table 2).
The overall postoperative morbidity rate was 36.6%. The most frequent postoperative complications were: wound problem (24 cases, 17.0%), pulmonary complication (24 cases, 17.0%), cardiac problem (6 cases, 4.2%), urological complication (6 cases, 4.2%), and fluid collection (6 cases, 4.2%) (Table 3). The overall mortality rate was 6.3%. All of the latter patients expired due to multi-organ failure following sepsis caused by postoperative pneumonia.
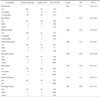
Univariate analysis was performed to identify operative risk factors of postoperative complications. An age above 60 years (P<0.01), sex (female, P=0.01), a high ASA score (P<0.01), the presence of preoperative shock (P=0.01), a surgical approach method (open method, P=0.01), and an operating time over 150 minutes (P=0.04) were associated significantly with postoperative morbidity (P<0.05) (Table 4). However, the type of operation, the use of combined organ resection, the site of perforation and the interval between ulcer perforation and operation were not significantly associated with postoperative morbidity.
The overall comorbidity rate was 51.4% (73 patients). The most frequent underlying diseases were hypertension (27.4%), diabetes mellitus (9.8%), and tuberculosis (7.0%) (Table 5). Univariate analysis was performed to determine which comorbidities were associated with postoperative morbidity. Hypertension (P=0.01), diabetes mellitus (P=0.04) and pulmonary disease (P=0.04) were associated significantly with overall postoperative morbidity. However, heart disease (P=0.75), chronic liver disease (P=0.69), tuberculosis (P=0.45), endocrine disease (P=0.36), and neurological disease (P=0.81) were not associated significantly with postoperative morbidity. In addition, the severity of the respective disease did not affect significantly to postoperative morbidity (Table 5).
Multivariate analysis was performed with the factors that were found to be statistically significant in the univariate analyses (Table 6). A high ASA score, the presence of preoperative shock, an open surgery, and a long operation time were statistically significant in the multivariate analysis (P<0.05). However hypertension, diabetes mellitus, pulmonary disease, age and sex were not significant factors (P>0.05). The risk of postoperative morbidity was increased by a high ASA score (odds ratio [OR]=6.1, 95% confidence interval [CI]=1.76~21.17), the presence of preoperative shock (OR=5.0, 95% CI=1.44~17.43), an open surgery (OR=2.8, 95% CI=1.01~7.99), and the operating time exceeding 150 minutes (OR=3.2, 95% CI=1.28~7.97).
Emergency operations for perforated peptic ulcer are associated with high morbidity and mortality rates. Studies that identify independent prognostic risk factors for postoperative morbidity in perforated peptic ulcer are warranted. The aim of this study was to investigate possible associations between postoperative morbidity and underlying disease or perioperative risk factors in perforated peptic ulcer. We found that a high ASA score, the presence of preoperative shock, an open surgery and a long operating time more than 150 minutes were risk factors for morbidity from a perforated peptic ulcer, but there was no association between postoperative morbidity from a perforated peptic ulcer and comorbid diseases.
The ASA classification is an assessment of the patient's preoperative physical status.(10) Lohsiriwat et al.(11) reported that the ASA classification could be used to predict poor surgical outcomes. In the present study, 3 (2.1%) patients had an ASA score of 1, 112 (78.9%) patients an ASA score of 2, 25 (17.6%) patients an ASA score of 3, and 2 (1.4%) patients an ASA score of 4. In univariate analysis, the ASA score was a significant risk factor for postoperative morbidity, and multivariate analysis revealed that the ASA score was an independent prognostic factor of morbidity from a perforated peptic ulcer.
Boey et al.(12) reported that preoperative shock and a long-standing perforation (≥24 hours) were important risk factors for postoperative morbidity and mortality following a perforated peptic ulcer. In the present study, 20 patients (14.1%) had a preoperative shock status and 74 patients (52.1%) had a long-standing perforation (≥24 hours). The patients with preoperative shock were associated with more postoperative morbidity than patients with a stable blood pressure (65.0% vs. 31.7%). Moreover, multivariate analysis revealed that preoperative shock was an independent prognostic factor for postoperative morbidity. On the other hand, a long-standing perforation was not a significant prognostic factor in univariate and multivariate analysis (P>0.05).
Linder et al.(13) reported that degree of peritonitis affects morbidity after an operation for intestinal perforation. However, in the present study, there was no data available about the degree of peritonitis in most cases; therefore, it was not possible to analyze the relationship between the degree of peritonitis and postoperative morbidity.
Lau et al.(14) and Sanabria et al.(15) reported that laparoscopic repair of perforated peptic ulcer was feasible and that laparoscopic repair and open repair groups do not differ significantly in terms of postoperative morbidity. Moreover, Siu et al.(16) reported that, compared to open repair, laparoscopic repair was associated with a shorter operating time, earlier removal of the peritoneal drain, fewer postoperative analgesics, a shorter hospital stay, an earlier return to a normal diet, and lower postoperative morbidity. In the present study, although the laparoscopic repair group had a longer average operating time than the open repair group, the difference was less than 10 minutes. Moreover, in univariate analysis, laparoscopic repair was associated with less postoperative morbidity than open repair (17.9% vs. 42.7%). Moreover, multivariate analysis revealed that the surgical approach was an independent prognostic factor for postoperative morbidity. However, the present study is a retrospective study and thus it remains possible that there was some selection bias that caused the patients who were in good general condition to belong to the laparoscopic surgery group.
When we analyzed patients who were in a stable condition upon admission, we performed primary repair. There was a significant decrease in wound complications in the laparoscopic surgery group rather than the open surgery group.
It has been known as the operating time influences postoperative morbidity. Hwang et al.(17) found that an operating time exceeding 3 hours was associated with a higher morbidity rate than shorter operating times. In our study, the median operating time was 149.6 minutes. When the patients were divided into two groups on the basis of this mean time, we found that the patients with an operating time that exceeded 150 minutes were significantly more likely to suffer postoperative morbidity than the patients with shorter operating times (45.8% vs. 28.9%). Both the univariate and multivariate analyses also revealed that a long operating time was an independent prognostic factor for postoperative morbidity. However, it should also be noted that long operations may reflect difficult cases that lead to difficult operations.
Male gender is significantly associated with perforated peptic ulcer, as males account for 71.4~94.5% of perforated peptic ulcer cases.(18-24) However, while Sonnenberg(25) also found this, they also observed that the proportion of female patients has increased in recent years. In the present study, the proportion of males to females was 3.1 to 1. The morbidity rate was significantly higher for female patients than male patients, and female gender was found to be a statistically significant risk factor for postoperative morbidity (P<0.05) in univariate analysis but not multivariate analysis.
Age has been recognized as an important prognostic factor for perforated peptic ulcer. Testini et al.(26) revealed that patients over 65 years have a significantly higher mortality rate after surgery for perforated peptic ulcer than younger patients because of the more frequent presence of comorbid diseases. In the present study, the mean age of the patients was 56.5 years. Univariate analysis revealed that the postoperative morbidity rate for patients over 60 years of age (52.3%) was significantly higher than that for younger patients (23.4%). In particular, an age exceeding 60 years was significantly associated with urological complications. This may relate to the fact that benign prostatic hyperplasia increases with aging. However, age was not an independent prognostic factor for postoperative morbidity in multivariate analysis.
About 11.5~40.9% of patients with peptic ulcer disease have comorbid diseases. Park and Kang(20) and Ko et al.(27) reported that pulmonary disease was the most frequent comorbid disease, followed by hypertension and diabetes mellitus. Noguiera et al.(3) reported that hypertension was the most frequent comorbid disease, followed by pulmonary disease. In the present study, the most frequent comorbid diseases were hypertension (27%) and diabetes mellitus (9.7%). The patients with comorbid diseases had higher postoperative morbidities. In addition, univariate analysis found that hypertension, diabetes mellitus and pulmonary disease were significantly associated with a higher rate of postoperative morbidity. In particular, compared to normotensive patients, patients with hypertension were significantly more likely to suffer wound problems, pulmonary complications, and urological complications (P<0.05). Notably, the mean age of patients with hypertension was 71.2 years. In contrast, the mean age of normotensive patients was 50.9 years (P=0.008). Additionally, compared to normotensive patients, patients with hypertension were significantly associated with diabetes mellitus (P=0.022) and heart disease (P=0.016). Jeong et al.(9) reported that patients with heart disease had high morbidity rates after radical surgery for gastric cancer. The result that patients with heart disease had high morbidity rates after radical surgery for gastric cancer as Jeong et al.(9) reported, could be one of the reasons why patients with hypertension have a higher postoperative morbidity rate than normotensive patients. However, multivariate analysis showed that hypertension was not an independent prognostic factor of postoperative morbidity.
Hirsch and McGill(28) and Stagnaro-Green(29) observed that patients with diabetes mellitus who undergo surgery have an increased risk of postoperative morbidity. In addition, Schiff and Welsh(30) reported that patients with diabetes mellitus are at particularly high risk of infection, including wound, skin, and urinary tract infections and pneumonia, and that their mortality rate is about 20%. However, Jeong et al.(9) did not detect an increase in postoperative morbidity for patients with diabetes mellitus who had good perioperative glucose control. In the present study, univariate analysis revealed that diabetes mellitus was significantly associated with increased postoperative morbidity. However, diabetes mellitus differed from hypertension in that significant associations with specific complications were not observed. Moreover, multivariate analysis did not find that diabetes mellitus was an independent prognostic factor of postoperative morbidity. This may relate to the fact that the number of patients with diabetes mellitus was small. To verify the relationship between diabetes mellitus and morbidity after surgery for perforated peptic ulcer, additional studies should be conducted with more patients with diabetes mellitus.
There were several limitations in our study. First, the number of patients who had respective underlying diseases were insufficient for determining the contribution of those diseases to postoperative morbidity. Moreover, the data about underlying disease were collected retrospectively; thus, it was impossible to categorize exactly according to disease entity and severity. Second, there could have been some selection bias since the patients who were in poor condition tended to be in the open surgery group. This could have affected the results regarding the surgical approach. Third, the study was retrospective and possible confounding factors could not be controlled.
The major strength of this study was that it examined the contribution of various underlying diseases to morbidity following perforated peptic ulcer surgery, although no underlying disease was found to be significantly associated with postoperative morbidity in this study. While several studies have investigated the relationship between overall underlying diseases and postoperative morbidity, the relationship between respective underlying diseases and postoperative morbidity for peptic ulcer perforation has not yet been studied. To verify the relationship between respective underlying disease and postoperative morbidity, a more prospective study with more patients with respective underlying diseases should be performed.
In conclusion, a high ASA score, the presence of preoperative shock, an open surgery and a long operating time more than 150 minutes are high risk factors for morbidity. In contrast, there is no association between postoperative morbidity and comorbid disease in patients with a perforated peptic ulcer. For patients with a high ASA score or preoperative shock, every effort should be made to shorten the operating time. Additionally, laparoscopic primary repair can be one of the strategies to decrease postoperative morbidity for patients with a high ASA score, unless the vital signs of patient are unstable.
Figures and Tables
Table 4
Univariate analysis of correlation between postoperative complication and clinical or perioperative characteristics

References
1. Chalya PL, Mabula JB, Koy M, McHembe MD, Jaka HM, Kabangila R, et al. Clinical profile and outcome of surgical treatment of perforated peptic ulcers in Northwestern Tanzania: A tertiary hospital experience. World J Emerg Surg. 2011. 6:31.

2. Mäkelä J, Laitinen S, Kairaluoma MI. Complications of peptic ulcer disease before and after the introduction of H2-receptor antagonists. Hepatogastroenterology. 1992. 39:144–148.
3. Noguiera C, Silva AS, Santos JN, Silva AG, Ferreira J, Matos E, et al. Perforated peptic ulcer: main factors of morbidity and mortality. World J Surg. 2003. 27:782–787.

4. Scheeres DE, DeKryger LL, Dean RE. Surgical treatment of peptic ulcer disease before and after introduction of H2 blockers. Am Surg. 1987. 53:392–395.
5. Imhof M, Epstein S, Ohmann C, Röher HD. Duration of survival after peptic ulcer perforation. World J Surg. 2008. 32:408–412.

6. Rahman MM, Islam MS, Flora S, Akhter SF, Hossain S, Karim F. Mortality in perforated peptic ulcer patients after selective management of stratified poor risk cases. World J Surg. 2007. 31:2341–2344.

7. Bittner R, Butters M, Ulrich M, Uppenbrink S, Beger HG. Total gastrectomy. Updated operative mortality and long-term survival with particular reference to patients older than 70 years of age. Ann Surg. 1996. 224:37–42.
8. Habu H, Endo M. Gastric cancer in elderly patients--results of surgical treatment. Hepatogastroenterology. 1989. 36:71–74.
9. Jeong SH, Ahn HS, Yoo MW, Cho JJ, Lee HJ, Kim HH, et al. Increased morbidity rates in patients with heart disease or chronic liver disease following radical gastric surgery. J Surg Oncol. 2010. 101:200–204.

10. Fitz-Henry J. The ASA classification and peri-operative risk. Ann R Coll Surg Engl. 2011. 93:185–187.

11. Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D. Perforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality. World J Surg. 2009. 33:80–85.

12. Boey J, Choi SK, Poon A, Alagaratnam TT. Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors. Ann Surg. 1987. 205:22–26.
13. Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E. The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis. Chirurg. 1987. 58:84–92.
14. Lau WY, Leung KL, Zhu XL, Lam YH, Chung SC, Li AK. Laparoscopic repair of perforated peptic ulcer. Br J Surg. 1995. 82:814–816.

15. Sanabria AE, Morales CH, Villegas MI. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. 2005. (4):CD004778.

16. Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, et al. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002. 235:313–319.
17. Hwang J, Kim JM, Kim HS. Clinical study and factors influencing postoperative morbidity in perforated peptic ulcer patients. J Korean Surg Soc. 2007. 73:130–137.
18. Heo IU, Kim HK, Lee SZ. A clinical study on peptic ulcer perforation. J Korean Surg Soc. 1984. 27:567–575.
19. Kang G, Kim CY, Min YD, Kim SH. Results of surgical treatment for perforated peptic ulcer. J Korean Surg Soc. 1993. 44:214–222.
20. Park JS, Kang JK. A clinical review in ulcer perforation of stomach and duodenum. J Korean Surg Soc. 1983. 25:736–744.
21. Kang RG, Jung SY, Suh JW. A clinical evaluation and follow up results of the surgical management on 172 patients with perforated peptic ulcer. J Korean Surg Soc. 1992. 42:292–303.
22. Lee HW, Ahn SI, Yang DH, Lee CH, Sohn JH, Kwon OJ, et al. A clinical review of peptic ulcer during 22 yrs (1968~1989). J Korean Surg Soc. 1993. 44:159–174.
23. Bae SW, Hwang JY, Lee YG. A clinical study of perforated peptic ulcer. J Korean Surg Soc. 1989. 36:737–743.
24. Shin HW, Moon SH, Lee YC, Kim JS, Chung BW, Chung KS. APACHE II score in emergency operation for perforation of gastroduodenal ulcer. J Korean Surg Soc. 1994. 47:501–509.
25. Sonnenberg A. Changes in physician visits for gastric and duodenal ulcer in the United States during 1958-1984 as shown by National Disease and Therapeutic Index (NDTI). Dig Dis Sci. 1987. 32:1–7.

26. Testini M, Portincasa P, Piccinni G, Lissidini G, Pellegrini F, Greco L. Significant factors associated with fatal outcome in emergency open surgery for perforated peptic ulcer. World J Gastroenterol. 2003. 9:2338–2340.

27. Ko JW, Hong SJ, Ban JY, Kim JH. Risk factors associated with mortality in emergency surgery for perforated peptic ulcer. J Korean Surg Soc. 2004. 67:373–378.
28. Hirsch IB, McGill JB. Role of insulin in management of surgical patients with diabetes mellitus. Diabetes Care. 1990. 13:980–991.

29. Stagnaro-Green A. Perioperative glucose control: does it really matter? Mt Sinai J Med. 1991. 58:299–304.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download