Abstract
Purpose
We aimed to study the pattern of liver-injury in children with dengue fever (DF) and validate serum aminotransferase ≥1,000 IU/L as a marker of severe DF.
Methods
Children admitted with DF were included. DF was defined by presence of clinical criteria and positive serological or antigen tests in absence of other etiology. DF severity was graded as dengue without or with warning signs and severe dengue. Liver-injury was defined as alanine aminotransferase (ALT) more than twice the upper limit of normal (boys, 30 IU/L; girls, 21 IU/L).
Results
Of 372 children with DF, 144 (38.7%) had liver-injury. Risk of liver-injury and aminotransferase levels increased with DF severity (p<0.001). Recommended ALT and aspartate aminotransferase (AST) cut-off at ≥1,000 IU/L had sensitivity 4.8% (5/105), specificity 99.3% (265/267) for detection of severe DF. In children with ALT and AST <1,000 IU/L (n=365), the area under receiver operating curves for prediction for severe DF, were 0.651 (95% confidence interval [CI], 0.588–0.714; p<0.001) for ALT and 0.647 (95% CI, 0.582–0.712; p<0.001) for AST. Serum ALT at 376 IU/L and AST at 635 IU/L had sensitivity and specificity comparable to ≥1,000 IU/L for defining severe DF.
Dengue virus (DENV) is transmitted to humans through female Aedes mosquito bites. All four serotypes (DENV 1–4) of DENV cause a common febrile illness, known as dengue fever (DF), and pose a major health problem in developing countries including India [1].
DF primarily run a mild and self-limiting course, though occasionally it may be life-threatening. Overall, DF carries an approximately 1% risk of death [1]. Severity of DF is graded in categories that facilitate patient care and prognosis assessment. Earlier, World Health Organization (WHO) had graded severity as DF, dengue hemorrhagic fever (DHF) and dengue shock syndrome [2]. Changing epidemiology of DF leads to difficulty in applying criteria for DHF in the clinical situation and studies revealed clinically severe dengue cases that failed to meet strict criteria of DHF [34]. Considering the need for redefining severity of DF, WHO reclassified severity as severe DF (SDF) and non-severe DF with the later group sub-classified into dengue without warning signs (dengue with no warning signs, DNWS) and dengue with warning signs (DWS) [1]. Patients with SDF are more likely to have adverse outcome and need hospitalization and management in an intensive care unit. Early recognition of SDF is essential for timely intervention and judicious use of scarce critical care support. SDF is diagnosed in presence of either of the following criteria (i) severe plasma leak leading to shock or respiratory distress due to fluid accumulation, (ii) severe bleeding as judged by the physician, or (iii) sever organ involvement as suggested by alanine aminotransferase (ALT) or aspartate aminotransferase (AST) ≥1,000 IU/mL or impaired consciousness or heart or other organ [1]. Among all the three SDF defining criteria, marked elevation (>1,000 IU/L) of ALT or AST is an objective criteria easily and widely available [1].
Elevation of serum levels of ALT and AST are biochemical indicators for hepatocyte damage. Liver injury (LI) in patients with DENV infection is common and several hypotheses have been proposed to explain the mechanism of LI [5]. Severity of LI ranges from asymptomatic mild elevation of serum levels of aminotransferase to life-threatening acute liver failure (ALF) [678]. The majority of data on LI in DENV infection is from the adult population. Regarding Indian children, DENV related LI is not well studied [91011].
The city of Lucknow in India recently faced an epidemic of DF in the second half of 2016. This retrospective study was focused on studying the pattern of LI in children admitted with DF and validate the WHO suggested aminotransferase ≥1,000 IU/L as SDF defining criteria in children.
This retrospective study was conducted in Lucknow, India. Children of age 1 to 18 years, admitted between July 2016 and December 2016 with diagnosis of DF, were included if at least one set of values for total serum bilirubin, ALT and AST were available during the course of DF illness. Children were included irrespective of severity of DF or liver involvement.
For retrospective data review, children with DF were identified by reviewing the departmental admission/discharge register for the study period. Patient's case files of identified children were retrieved, and relevant clinical and laboratory data were extracted in a predefined data collection form.
DF was diagnosed in presence of the following three criteria: (i) probable dengue as suggested by WHO, (ii) positive test result for either DENV specific immunoglobulin M antibody or NS1 antigen, and (iii) absence of other etiology likely to explain the illness, if required. Severity of DF was graded into DNWS, DWS and SDF to comply with WHO criteria.
According to WHO, probable dengue is defined as an acute febrile illness in a person that lived/traveled to a dengue endemic area and has at least two features among the following: nausea, vomiting; rash; aches and pains; positive tourniquet test and; leucopenia. Warning signs include abdominal pain or tenderness, persistent vomiting, clinical fluid accumulation, mucosal bleed, lethargy or restlessness, liver enlargement >2 cm, increase in hematocrit with rapid decrease in platelet count. Further, severe dengue is defined in presence of evidence of either of the following three features: (i) severe plasma leakage leading to shock or fluid accumulation with respiratory distress, (ii) severe bleeding as judged by clinician, and (iii) severe organ involvement such as liver (suggested by ALT or AST ≥1,000 IU/L), central nervous system (suggested by impaired consciousness), heart or other organ.
During the hospital stay, the children were treated according to the WHO guidelines recommended for treatment of DF [1]. According to the clinical requirement, children were investigated to exclude other causes of acute febrile illnesses such as malaria, enteric fever, hepatitis A virus etc.
Serum level of ALT and AST were chosen as a marker of LI. For a child with multiple values of serum enzymes available during illness, ALT and AST values temporally closest to the nadir of platelets counts were included for analysis and disease severity was also noted for the same day.
To define the upper limits of normal (ULN), the cut-offs for ALT and AST were ascertained as 30 and 38 IU/L for boys and 21 and 33 IU/L for girls, respectively. These limits were chosen from a study with a reasonable representation of children and represents 95th percentile of the normal range [12]. Because of higher specificity for liver [13], ALT level was chosen to define LI. A child was assumed to sustain LI at serum ALT >2×ULN (ALT >60 IU/L for boys, >42 IU/L for girls).
Outcome of a child was recorded as either favorable or adverse. Children discharged in satisfactory condition had favorable outcomes. Children either discharged on parents' request or died were recorded as having adverse outcomes.
Numerical and categorical data are expressed as median (range) and proportion or ratio. Intergroup comparison was done using non-parametric statistical tests with level of significance at p<0.05. Statistical software program SPSS version 20 (IBM Co., Armonk, NY, USA) was used for data analysis.
Children's records were reviewed after obtaining institute's ethic committee permission with waiver of consent.
The clinical characteristics and the relevant laboratory parameters of the cohort of children included in analysis are summarized in Table 1. Two thirds of the children were boys. Majority of our children belonged to the adolescent age group. Seventeen (4.6%) children had adverse outcomes that include ten deaths (DNWS two, SDF eight) and seven children discharged on request (DWS two, SDF five). None of the deaths were related to ALF. Prevalence of various indicators of liver involvement progressively increased with advancing disease severity. Median levels of ALT and AST revealed progressive and significant increase with increasing severity of DF (Fig. 1).
According to our cut-off limits, 144 (38.7%) children with DF had LI. Median (range) levels of ALT and AST among children without LI were 34 (11–60) and 38 (7–60) for DNWS, 42 (18–58) and 43 (22–217) for DWS, 56 (4–306), and 65 (23–162) for SDF respectively. Their levels were not significantly different between the three subgroups (p=0.244 for ALT, 0.070 for AST). In all three DF severity subgroups, median levels of ALT and AST were significantly higher (p<0.001) among children with LI than those without LI.
Demographic profile, clinical characteristics, laboratory investigations and outcomes of the children with LI are summarized in Table 2. Proportions of children developing LI increased significantly with increasing severity of DENV infection (p<0.001). In children with LI, the ALT and AST elevation revealed good correlation (Pearson's coefficient 0.812, p<0.001; Fig. 2). This correlation was good for SDF (r=0.844, p<0.001) and moderate for DNWS (r=0.641, p=0.001) and DWS (r=0.631, p<0.001) subgroups. Levels of ALT and AST increased significantly with advancing grades of disease (Fig. 3).
Seven children with LI, had ALT and/or AST ≥ 1,000 IU/L. Five had SDF and two had non-severe dengue. In our cohort, the ALT and AST cut-off at ≥ 1,000 IU/L had sensitivity 4.8% (5/105), specificity 99.3% (265/267), positive predictive value 71.4% (5/7) and negative predictive value 72.6% (265/365) for detection of SDF.
Among children with ALT and AST <1,000 IU/L (n=365), the area under the receiver operating curves (AUROC) for prediction of SDF were 0.651 (95% confidence interval [CI], 0.588–0.714; p<0.001) and 0.647 (95% CI, 0.582–0.712; p<0.001) for ALT and AST respectively. Serum ALT level at 376 IU/L revealed sensitivity and specificity of 5.0% and 99.2% respectively. Similarly, serum AST at 635 IU/L revealed sensitivity and specificity of 5.0% and 98.1% respectively (Fig. 4).
This single center, retrospective study included 372 children with DF affected during an epidemic. Overall, approximately one third of the children sustained LI. Median levels of ALT and AST were significantly higher in presence of LI. Extent of ALT and AST elevation revealed good correlation with each other. Among those with LI, levels of ALT and AST increased significantly with increasing severity of DF. The WHO suggested cut-off of ALT and AST ≥ 1,000 IU/L had sensitivity 4.8% (5/105) and specificity 99.3% for detection of SDF. Among children with ALT and AST <1,000 IU/L, the ROC curves had comparable sensitivity and specificity at ≥376 IU/L for ALT and ≥635 IU/L for AST respectively.
LI is known in DF and could manifest as either hepatomegaly, asymptomatic elevation of liver enzymes, mild icteric hepatitis or ALF. Several workers have studied the pattern of liver involvement in DENV infection. Majority of such studies have focused primarily on clinical features such as edema, ascites, jaundice etc as an indicator of LI. Such studies have clearly demonstrated elevation of ALT and AST in presence of LI but the pattern of elevation of such enzymes are not well studied, especially in children [111415]. The association of serum levels of ALT or AST with severity of DF has not been studied.
The proportion of children that developed LI (38.7%) was relatively smaller in our study than previously reported 65.2% to 96% in adults [7910] and 90% in children [14]. Relatively lower prevalence of LI in our cohort could be because of differences in LI defining criteria such as (i) we set the cut-off at twice the ULN for ALT instead of a value above the ULN; the only other study that used ALT >2×ULN criteria to define LI, affirmed 35.5% prevalence of LI in children with DF [16]; (ii) ALT alone, but not AST, was used to define LI that made our LI defining criteria more restrictive; in a generalized illness, such as DF, AST elevation is much more frequent and levels are higher than ALT because AST is affirmed in several tissues other than the liver and AST release from those tissue could be much more than its release from liver; (iii) relatively smaller proportion of children with SDF in our study as compared to previous studies; and (iv) there could be unidentified factors related to DENV such as virus genotype, subtypes or quasispecies phenomenon to explain such discrepancy.
Though, reported previously [17], none of the children in our study developed HENV related ALF. Previous small experiences have revealed ALF in up to 10% of those with severe disease [14]. The three largest experiences, that studied liver involvement in patients with DF and included more than 3,500 patients, did not find any patient of ALF [71118]. A recent large retrospective study of 1,926 patients revealed a low (0.31%) incidence rate of ALF in patients with DF [8]. Over representation of dengue related ALF in few series may be because of undiagnosed co-infection with hepatotropic viruses that could cause ALF or factors related to virulence of the virus involved in a given study.
Our results revealed increased risk of LI with increasing severity of DF. Proportions of children developing LI as well as median levels of ALT and AST increased with increasing disease severity. Similar results have been reported in previous studies [7111418]. In presence of LI, ALT and AST revealed good correlation and AST levels were relatively higher than ALT in contrast to hepatotropic virus induced acute hepatitis wherein ALT in much more than AST. Higher levels of AST in DF could be because of its release from tissues other than the liver. This relatively higher level of AST than ALT could help to differentiate between hepatotropic virus and DENV related LI.
In our study, WHO suggested ALT and/or AST level ≥1,000 IU/L revealed poor sensitivity and moderate positive predictive value for SDF. Overall, the ROC for ALT or AST had moderate AUROC and hence their levels were not determined to be a good indicator for SDF. A previous study done in a large cohort of adult patients has also revealed poor discriminatory power of ALT and AST levels for differentiating between severe and non-severe dengue [18]. In our cohort, ALT and AST levels above 376 IU/L and 635 IU/L revealed sensitivity and specificity comparable to the recommended limit of ≥1,000 IU/L, for predicting SDF. A recent study, that compared LI between adults and children with DF, revealed higher level of ALT and AST in adults than children [16]. These relatively lower levels of ALT and AST in children, than the recommended cut-off at ≥1,000 IU/L, may be because of either smaller body size and hence lower liver tissue mass or involvement of a different pathogenic mechanism inducing LI. Hence, our data suggests the need for (i) A relatively lower limits for serum ALT and AST as a marker of severe disease, and (ii) Separate cut-off for ALT and AST for predicting severe disease.
This study had strength such as (i) relatively larger cohort size, (ii) good representation of all three disease severity groups, and (iii) inclusion of children suffered during single epidemic during a short span of six months.
Our study had few limitations as well; first, the retrospective nature of the study; second, inclusion of single values of ALT and AST level, of which peaks may not temporally coincide with the worst stage of severity of DF; third, lack of details on temporal pattern of liver enzymes during the course of illness; and fourth, failure to measure serum lactate dehydrogenase, a marker of ischemic injury of liver [19], that could have improved our understanding about the pathogenesis of DENV related LI.
In conclusion, LI is common during the course of DF but ALF is uncommon. In presence of LI, AST is higher than ALT. Serum levels of liver enzymes increase with worsening disease severity. Serum ALT and AST levels of ≥1,000 IU/L is not a good predictor of SDF, and we could lower theses cut-offs to 376 IU/L for ALT and 635 IU/L for AST without compromising sensitivity and specificity of these markers.
Figures and Tables
Fig. 1
Boxplot comparing the serum levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) enzymes in children with liver injury (n=372) and different grades of dengue fever severity. Outliers are represented as asterix (between 1.5–3.0 times of box length) and empty circle (>3 times of box lengths) from a hinge.

Fig. 2
Correlation between serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels in children with dengue fever and liver injury. Enzyme levels are expressed in multiples of upper limits of normal (ALT and AST cut-offs taken at 30 and 38 IU/L for boys and 21 and 33 IU/L for girls respectively).
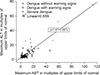
Fig. 3
Boxplot comparing the serum levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) enzymes in children with liver injury (n=144) and different grades of dengue fever severity. Outliers are represented as asterix (between 1.5–3.0 times of box length) and empty circle (>3 times of box lengths) from a hinge.

Fig. 4
Receiver operating curve (ROC) revealing serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) level for prediction of severe dengue.
AUROC: area under ROC.
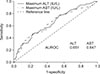
Table 1
Clinical Characteristics, Laboratory Investigations and Outcomes in Children with Dengue Fever

References
1. World Health Organization. Dengue: guidelines for diagnosis treatment prevention and control. Geneva: WHO;2009. p. 147.
2. World Health Organization. Dengue haemorrhagic fever: diagnosis, treatment, prevention and control. Geneva: WHO;1997. p. 84.
3. Alexander N, Balmaseda A, Coelho IC, Dimaano E, Hien TT, Hung NT, et al. Multicentre prospective study on dengue classification in four South-east Asian and three Latin American countries. Trop Med Int Health. 2011; 16:936–948.

4. Barniol J, Gaczkowski R, Barbato EV, da Cunha RV, Salgado D, Martinez E, et al. Usefulness and applicability of the revised dengue case classification by disease: multi-centre study in 18 countries. BMC Infect Dis. 2011; 11:106.

5. Seneviratne SL, Malavige GN, de Silva HJ. Pathogenesis of liver involvement during dengue viral infections. Trans R Soc Trop Med Hyg. 2006; 100:608–614.

6. Ling LM, Wilder-Smith A, Leo YS. Fulminant hepatitis in dengue haemorrhagic fever. J Clin Virol. 2007; 38:265–268.

7. Souza LJ, Alves JG, Nogueira RM, Gicovate Neto C, Bastos DA, Siqueira EW, et al. Aminotransferase changes and acute hepatitis in patients with dengue fever: analysis of 1,585 cases. Braz J Infect Dis. 2004; 8:156–163.

8. Kye Mon K, Nontprasert A, Kittitrakul C, Tangkijvanich P, Leowattana W, Poovorawan K. Incidence and clinical outcome of acute liver failure caused by dengue in a hospital for tropical diseases, Thailand. Am J Trop Med Hyg. 2016; 95:1338–1344.

9. Ahmad S, Dhar M, Srivastava S, Bhat NK, Shirazi N, Biswas D, et al. Dengue hepatitis sans dysfunction: experience of a single tertiary referral centre in the north Indian state of Uttarakhand. Trop Doct. 2013; 43:62–65.

10. Itha S, Kashyap R, Krishnani N, Saraswat VA, Choudhuri G, Aggarwal R. Profile of liver involvement in dengue virus infection. Natl Med J India. 2005; 18:127–130.
11. Saha AK, Maitra S, Hazra SCh. Spectrum of hepatic dysfunction in 2012 dengue epidemic in Kolkata, West Bengal. Indian J Gastroenterol. 2013; 32:400–403.

12. Poustchi H, George J, Esmaili S, Esna-Ashari F, Ardalan G, Sepanlou SG, et al. Gender differences in healthy ranges for serum alanine aminotransferase levels in adolescence. PLoS One. 2011; 6:e21178.

13. Schiff ER, Sorrell MF, Maddrey WC, Schiff L. Schiff's diseases of the liver. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2007.
14. Roy A, Sarkar D, Chakraborty S, Chaudhuri J, Ghosh P, Chakraborty S. Profile of hepatic involvement by dengue virus in dengue infected children. N Am J Med Sci. 2013; 5:480–485.

15. Jagadishkumar K, Jain P, Manjunath VG, Umesh L. Hepatic involvement in dengue fever in children. Iran J Pediatr. 2012; 22:231–236.
16. Martinez Vega R, Phumratanaprapin W, Phonrat B, Dhitavat J, Sutherat M, Choovichian V. Differences in liver impairment between adults and children with dengue infection. Am J Trop Med Hyg. 2016; 94:1073–1079.

17. Chongsrisawat V, Hutagalung Y, Poovorawan Y. Liver function test results and outcomes in children with acute liver failure due to dengue infection. Southeast Asian J Trop Med Public Health. 2009; 40:47–53.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download