Abstract
Purpose
This study investigated the clinical presentations of symptomatic Clostridium difficile infection (CDI) in children.
Methods
We reviewed the medical records of 43 children aged <20 years who showed either positive C. difficile culture or C. difficile toxin test results between June 2010 and April 2014.
Results
Of the 43 patients (mean age 6.7 years), 22 were boys. Sixteen patients (37.2%) showed both positive C. difficile culture and toxin test results. Seventeen out of 43 children (39.5%) had preexisting gastrointestinal diseases, and 26 children had other medical conditions that were risk factors for CDI. Twenty-eight children had a history of antibiotic treatment for >3 days, and the most frequently prescribed antibiotic was amoxicillin-clavulanate (35.7%). Twenty-eight patients were diagnosed with CDI despite taking probiotic supplements, most commonly Lactobacillus acidophilus (53.6%). The most common symptom was diarrhea (72.1%) at the time CDI was diagnosed. C. difficile was eradicated in 11 patients (25.6%) after treatment with oral metronidazole for 10-14 days, and in the two patients (4.6%) who required two courses of oral metronidazole. Sixteen patients (37.2%) showed clinical improvement without any treatment.
Clostridium difficile was first isolated in 1935 by Hall and O'Toole [1], and is one of the most common causes of antibiotic-associated diarrhea in high-income countries. C. difficile is a gram positive, cytotoxin-producing anaerobic bacterium commonly existing in colonies without exhibiting symptoms. However, under stressful conditions such as exposure to antibiotics, it causes symptoms due to disruption of the intestinal microflora barrier. The symptoms of C. difficile infection (CDI) vary from mild diarrhea (usually self-limited) to pseudomembranous colitis, fulminant colitis, toxic megacolon, and even death [2]. In healthy newborns and infants are infected by enteric C. difficile, but the potent exotoxins have no effect in these infants, in contrast to severe diarrhea and colitis in older children and adults [3,4].
The incidence of CDI has rapidly increased since 1990, and the mortality rate has increased markedly since 2000 [5,6,7,8]. The incidence of CDI in children and the median hospital charge for this diagnosis code have increased [9,10].
The importance of a high number of lactobacilli in intestinal flora for the health and longevity of humans was first acknowledged before the 20th century [11]. In 1965, Lilly and Stillwell [12] first used the term "probiotics." Since then, various types of probiotics were found. Many scientists believed that such probiotics would be effective for CDI due to their ability to maintain normal flora. Although many studies are available about the relationship between probiotics and their effects on the prevention and treatment of CDI in adults, this relationship is not well known in children.
In this study, we investigated the clinical characteristics of symptomatic CDI in children and adolescents based on the clinical presentation, related preexisting gastrointestinal (GI) disease, implicated antibiotics, and whether various probiotics really have protective effects against CDI.
Positive C. difficile culture or C. difficile toxin A, B test results were found in 775 patients at Hanyang University Medical Center between June 2010 and April 2014. Among the 775 patients, 732 patients aged >20 years were excluded. Therefore, 43 patients were included in this study. All 43 patients had any GI symptoms when they were diagnosed with CDI, and three had more than one episode of CDI.
The stool samples were pre-treated with 99% ethanol for 30 min at room temperature. The samples were inoculated on selective media with antibiotics (Clostridium difficile Moxalactam Norfloxacin), and cultured anaerobically for 24-48 h at 36℃. Suspected C. difficile colonies were identified with an API Rapid ID 32A system (bioMérieux SA, Lyon, France). C. difficile toxin A and B were detected by VIDAS C. difficile Toxin A&B (bioMérieux SA) kits.
We retrospectively reviewed data of patients from medical records, including age and sex distribution; the number of patients with preexisting GI disease; the number of patients with a history of antibiotic treatment during the former several months; which antibiotics were implicated; the number of patients treated with probiotic therapy in conjunction with the antibiotics to protect against CDI; and eradication treatment. The treatment plan was as followings; for patients with suspected CDI, ongoing antibiotic treatment was stopped. If symptoms of CDI persisted for 5 days after antibiotic withdrawal, treatment for CDI was started. Oral metronidazole for 10-14 days was the initial treatment, followed by oral vancomycin for 10 days if stool culture results after metronidazole treatment were positive for C. difficile. Oral metronidazole treatment was repeated in two patients because their parents did not provide consent for oral vancomycin treatment.
Data were analyzed using IBM SPSS Statistics 21.0 (IBM Co., Armonk, NY, USA). Continuous variables were represented as mean±standard deviation. Categorical variables were analyzed using the chi-square test or Fisher's exact test. p-values <0.05 were considered statistically significant.
Among the 43 patients with CDI, 22 were boys and 21 were girls. The majority of children were aged ≤3 years (22 children, 51.2%), and 15 were aged <1 year (34.9%). The mean age of the patients was 6.7±6.8 years, which was higher in boys (8.7 years) than in girls (4.8 years) (Fig. 1).
Forty patients showed a positive C. difficile culture result, and 19 patients (44.2%) showed a positive C. difficile toxin A or B result. Sixteen patients (37.2%) showed both positive C. difficile culture and C. difficile toxin test results. Three patients showed a positive toxin test result, but negative culture result. The age distribution of toxin-positive CDI was similar to that of culture-positive CDI. Twelve patients (63.2% with toxin-positive CDI) were aged <3 years (Fig. 2).
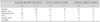
Seventeen out of 43 children (39.5%) had preexisting GI diseases: four had Crohn's disease; three had allergic colitis and/or eosinophilic colitis; three had severe GI complications associated with chemotherapy; two had recurrent abdominal pain; two had chronic diarrhea; and one child each had constipation, diverticulitis, and zinc deficiency with diarrhea. Twenty-six patients (60.4%) had no history of GI diseases but had various other medical conditions: 12 with extra-intestinal infections (otitis media, tonsillitis, pneumonia, bronchitis, sinusitis, sepsis) and were treated with antibiotics for greater than 3 days; three premature babies who were hospitalized long-term in the neonatal intensive care unit; and five hospitalized for a major extra-intestinal operation and/or trauma (Table 1).
Twenty-eight out of 43 patients (65.1%) were previously exposed to antibiotics during the former several months, and 22 kinds of antibiotics were prescribed. The most common antibiotic was amoxicillin-clavulanate, used in 10 patients (35.7%). Trimethoprim/sulfamethoxazole was used in 6 patients (21.4%), and for long-term prophylaxis of protozoal infections in two patients who had cancer. Cefotaxime and cefdinir were used in 4 patients, respectively (14.2%). Ampicillin, gentamicin, cefepime, and ceftriaxone were used in 2 patients each (7.1%) (Table 2).
Probiotics were prescribed for prophylaxis of CDI in 28 patients concomitantly with antibiotic therapy. Twelve different kinds of probiotics were identified, and the mean duration of probiotic treatment was 32.9±61.7 weeks. The patients with Crohn's disease had taken probiotics for many years previously. Lactobacillus acidophilus was the most commonly used (15 patients, 53.6%), followed by Bacillus subtilis and Streptococcus faecium (Table 3).
The most common clinical symptom was change in stool at the time CDI was diagnosed, especially watery diarrhea in 31 patients (72.1%). Other major symptoms were abdominal pain, fever, and vomiting. Abdominal pain was more commonly seen in patients with preexisting GI diseases. However, there were no other statistically significant relationships among underlying GI diseases, history of antibiotic treatment, or prophylactic probiotics (Table 4).
Eleven patients (25.6%) treated with metronidazole for 10-14 days (1 cycle) showed negative C. difficile culture results on follow-up. C. difficile was eradicated in the two patients treated with two cycles of oral metronidazole. Oral vancomycin was administered to four symptomatic patients with positive C. difficile stool culture results; negative C. difficile culture results were obtained after treatment in 3 of the 4 patients. One of the patients with Crohn's disease was a vancomycin non-responder (repeated C. difficile positivity), but GI symptoms were relieved after oral vancomycin; hence, eradication treatment was stopped. Repeat oral metronidazole treatment was administered in one child with persistent symptoms after oral vancomycin treatment; C. difficile stool culture results were negative after this treatment. Six patients showed clinical improvement with metronidazole or ciprofloxacin, but were lost to follow-up with no stool data. Sixteen patients (37.2%) showed clinical improvement without any treatment (Table 5).
C. difficile is one of the common infectious causes of health care-related. It is a Gram-positive, sporeforming anaerobic rod bacterium that produces toxin. It can cause diarrhea and colitis due to inflammation of the intestinal epithelium and cell death. CDI incidence is lower in children than in adults. Due to the protective effects of the premature immune system and maternal antibodies, it is often remains asymptomatic in its simple colonized form after infection [13]. Similarly, the proportion of toxin-positive CDI in our study was lower than that in other age groups. At the age of two, the percentage of asymptomatic, simple colonized-form decreases to 6%, and after two years old, the rate drops to the similar percentages in adults (3%) [14]. In other words, the incidence of CDI tends to rapidly decrease after the age of 2 years [15,16]. Similar to the epidemiology studies in the United States, our study also showed that 40% of children with confirmed CDI were aged <2 years. One of the two neonates in our study who was <1 month of age showed both positive C. difficile culture and C. difficile toxin test results. Two neonates showed clinical improvement without any treatment. Our study participants were children with acute GI symptoms; therefore, the actual incidence of CDI could be slightly different in each age group.
Unlike in adults, risk factors in children are not well known. Known CDI risk factors and predisposing conditions in children include the following: young age, prolonged hospitalization, gastrostomy or jejunostomy tube feeding, broad-spectrum antibiotic therapy, hematopoietic stem cell and solid-organ transplantation, inflammatory bowel disease (IBD), neoplastic disease, immunodeficiency, cystic fibrosis, fungal infection, and viral gastroenteritis. In children, a significant association between CDI and proton-pump inhibitors therapy is more controversial [17,18]. In this study, most of the children with confirmed CDI also had at least 1 risk factor. Change of intestinal normal flora was thought to cause the underlying GI disease; further studies should be performed to identify the types of underlying diseases that cause CDI. In a study on the relationship between CDI and IBD, there was no difference between type of IBD and CDI in pediatric patients, though CDI was more common in ulcerative colitis patients in adults [19]. CDI is a well-known hospital-acquired disease. A study concerning the possibility of person to person transmission of C. difficile via molecular biologic methods revealed that there was no matching of the strains among the infected children, suggesting C. difficile was prevalent in the hospital environment in the shared spaces [20].
Many studies have found a relationship between antibiotic use and CDI. In adults, cephalosporins and fluoroquinolones increase predisposition to CDI compared with other antibiotics [21,22]. On the contrary, a study on the relationship between CDI and antibiotics in children showed that cefotaxime, amikacin, ampicillin, cefazolin, and vancomycin were most commonly associated with the development of CDI [23]. In our study, 10 of 26 patients with previous antibiotic exposure had been treated with amoxicillin-clavulanate. This is likely because amoxicillin-clavulanate is currently one of the most commonly preferred prescriptions in Korea.
Incidence of CDI has increased, and often progresses to severe disease. Many prevention measures for CDI have been used, including limiting the use of prophylactic broad-spectrum antibiotics, isolating infected patients in the hospital, and using appropriate hand washing. In addition, many studies have been conducted on the relationship between CDI and probiotics. The effect of probiotics on antibiotic-associated diarrhea is well known; probiotics use has also proven relatively effective for CDI. Also, the study of Saccharomyces boulardii has been increasingly used for prophylaxis of CDI, and many studies are on-going about other intestinal medicines [17,24,25,26]. However, except for a case report of S. boulardii treatment for recurrent CDI, the number of large-sized studies on the prophylactic effect of CDI with probiotics other than S. boulardii is limited [17,27]. In our study, CDI was confirmed in 28 patients who had been treated with probiotics (including S. boulardii). Although the two patients with Crohn's disease had been treated with probiotics for >1 year, they still repeatedly presented with symptomatic CDI.
The limitations of this study are the lack of a control group because of the retrospective nature of the study, and inability to measure the dosage of the probiotics given for prophylaxis of CDI. It was reported that a high enough dose of probiotics (5 billion colony-forming unit/day) may be effective in treating or preventing one out of seven cases of diarrhea [28]. In addition, all patients in our study had acute GI symptoms, there was no need to separate those with toxin-positive CDI and culture-positive CDI. In our study, we performed multiplex polymerase chain reaction on five patients for supplemental diagnosis; four of these patients showed positive results. However, the number of patients was very small for the data to be significant. Further evaluations should be performed in children to accurately diagnose CDI and to determine the use of probiotics as prophylaxis.
Figures and Tables
Table 1
Preexisting Clinical Conditions that Increase Predisposition to Clostridium difficile Infection

Values are presented as number only or number (%).
CDI: Clostridium difficile infection, NICU: neonatal intensive care unit.
*Three recurrent CDI episodes in the 2 patients with Crohn's disease; two recurrent CDI episodes in 1 prematurity. †Otitis media, tonsillitis, pneumonia, bronchitis, sepsis, sinusitis.
References
1. Hall IC, O'Toole E. Intestinal flora in new-born infants: with a description of a new pathogenic anaerobe, bacillus difficilis. Am J Dis Child. 1935; 49:390–402.
2. Burke KE, Lamont JT. Clostridium difficile infection: a worldwide disease. Gut Liver. 2014; 8:1–6.
3. Rousseau C, Poilane I, De Pontual L, Maherault AC, Le Monnier A, Collignon A. Clostridium difficile carriage in healthy infants in the community: a potential reservoir for pathogenic strains. Clin Infect Dis. 2012; 55:1209–1215.

4. Jangi S, Lamont JT. Asymptomatic colonization by Clostridium difficile in infants: implications for disease in later life. J Pediatr Gastroenterol Nutr. 2010; 51:2–7.

5. Kelly CP, LaMont JT. Clostridium difficile--more difficult than ever. N Engl J Med. 2008; 359:1932–1940.
6. Zilberberg MD, Shorr AF, Kollef MH. Increase in adult Clostridium difficile-related hospitalizations and casefatality rate, United States, 2000-2005. Emerg Infect Dis. 2008; 14:929–931.

7. Pépin J, Valiquette L, Alary ME, Villemure P, Pelletier A, Forget K, et al. Clostridium difficile-associated diarrhea in a region of Quebec from 1991 to 2003: a changing pattern of disease severity. CMAJ. 2004; 171:466–472.
8. Katikireddi V. UK launches inquiry into Clostridium difficile outbreak. CMAJ. 2005; 173:138.
9. Cohen MB. Clostridium difficile infections: emerging epidemiology and new treatments. J Pediatr Gastroenterol Nutr. 2009; 48:Suppl 2. S63–S65.
10. Zilberberg MD, Tillotson GS, McDonald C. Clostridium difficile infections among hospitalized children, United States, 1997-2006. Emerg Infect Dis. 2010; 16:604–609.

11. Metchnikoff E. The prolongation of life: optimistic studies. London: William Heinemann;1907. p. 161–183.
12. Lilly DM, Stillwell RH. Probiotics: growth-promoting factors produced by microorganisms. Science. 1965; 147:747–748.

13. McFarland LV, Brandmarker SA, Guandalini S. Pediatric Clostridium difficile: a phantom menace or clinical reality? J Pediatr Gastroenterol Nutr. 2000; 31:220–231.
14. Bryant K, McDonald LC. Clostridium difficile infections in children. Pediatr Infect Dis J. 2009; 28:145–146.
15. Kim J, Smathers SA, Prasad P, Leckerman KH, Coffin S, Zaoutis T. Epidemiological features of Clostridium difficile-associated disease among inpatients at children's hospitals in the United States, 2001-2006. Pediatrics. 2008; 122:1266–1270.

16. Wendt JM, Cohen JA, Mu Y, Dumyati GK, Dunn JR, Holzbauer SM, et al. Clostridium difficile infection among children across diverse US geographic locations. Pediatrics. 2014; 133:651–658.

17. Pant C, Deshpande A, Altaf MA, Minocha A, Sferra TJ. Clostridium difficile infection in children: a comprehensive review. Curr Med Res Opin. 2013; 29:967–984.
18. Sandora TJ, Fung M, Flaherty K, Helsing L, Scanlon P, Potter-Bynoe G, et al. Epidemiology and risk factors for Clostridium difficile infection in children. Pediatr Infect Dis J. 2011; 30:580–584.

19. Hourigan SK, Oliva-Hemker M, Hutfless S. The prevalence of Clostridium difficile infection in pediatric and adult patients with inflammatory bowel disease. Dig Dis Sci. 2014; 59:2222–2227.

20. Warrack S, Duster M, Van Hoof S, Schmitz M, Safdar N. Clostridium difficile in a children's hospital: assessment of environmental contamination. Am J Infect Control. 2014; 42:802–804.

21. Monaghan T, Boswell T, Mahida YR. Recent advances in Clostridium difficile-associated disease. Postgrad Med J. 2009; 85:152–162.
22. Khan R, Cheesbrough J. Impact of changes in antibiotic policy on Clostridium difficile-associated diarrhoea (CDAD) over a five-year period in a district general hospital. J Hosp Infect. 2003; 54:104–108.

23. Kim BC, Yang HR, Jeong SJ, Lee KH, Kim JE, Ko JS, et al. Clostridium difficile colitis in childhood: associated antibiotics. Korean J Pediatr Gastroenterol Nutr. 2002; 5:143–149.

24. McFarland LV. Meta-analysis of probiotics for the prevention of antibiotic associated diarrhea and the treatment of Clostridium difficile disease. Am J Gastroenterol. 2006; 101:812–822.

25. Hell M, Bernhofer C, Stalzer P, Kern JM, Claassen E. Probiotics in Clostridium difficile infection: reviewing the need for a multistrain probiotic. Benef Microbes. 2013; 4:39–51.

26. Goldenberg JZ, Ma SS, Saxton JD, Martzen MR, Vandvik PO, Thorlund K, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2013; 5:CD006095.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download