Abstract
Focal osteoporotic bone marrow defect (FOBMD) is a radiolucent area corresponding to the presence of hematopoietic tissue rarely found in the jaws. FOBMD is most commonly located in the mandibular edentulous posterior area of a middle-aged female. From November 2011 to November 2012, we experienced three cases involving removal of implants that had accidentally fallen into the FOBMD area. All patients happened to be female, with a mean age of 54 years (range: 51-60 years). One case involved hypoesthesia of the lower lip and chin, while two cases healed without any complication. Displacement of an implant into the FOBMD area is an unusual event, which occurs rarely during placement of a dental fixture. The purpose of this study was to report on three cases of FOBMD and to provide a review of related literature.
Focal osteoporotic bone marrow defect (FOBMD) is a radiolucent area corresponding to the uncommon presence of hematopoietic tissue found in the jaws, usually at former extraction sites1,2. The lesion is usually asymptomatic and is incidentally detected during radiographic analysis. Radiographi-cally, it is localized, poorly demarcated radiolucency that varies in size, trabeculae, and border definition2-4.
Since FOBMD is occasionally included in the differential diagnosis of radiolucent lesions of the jaws, knowledge of the radiographic, clinical, and histopathological characteristics in association with accurate examination are mandatory to distinguish it from other most common intrabony defect lesions such as odontogenic cysts or traumatic bone cyst (TBC), aneurismal bone cyst, central giant cell granuloma, tumors, and primary or metastatic malignancies2.
Placement of dental implant has become a quite predictable procedure; nonetheless, there are risks associated with the surgical phase. Well-known intraoperative complications and accidents related to surgery include nerve damage, thermal damage, hemorrhage, damage of adjacent tooth, lack of primary stability, and displacement of implants.
The displacement of implants occurs intraoperatively or within a short period because of insufficient surgical technique or anatomical variances of the jaws. Deficiency of initial stability of implants can result from the low density of trabecular bone, thinness of the cortical bone, and osteopenia or osteoporosis; problems related to the use of surgical technique by an inexperienced operator, such as inadequate planning, overworking of the implant drilling, mishandling, and incorrect manipulation, have also been suggested as possible factors5,6. The investigators concluded that the medullar component in the posterior mandible may be similar to that found in the maxilla, and that it could facilitate the displacement of dental implants during surgery5.
In this report of 3 rare cases, the displacement of implants into the mandible corpus and its management are presented together with a review of literature on FOBMD.
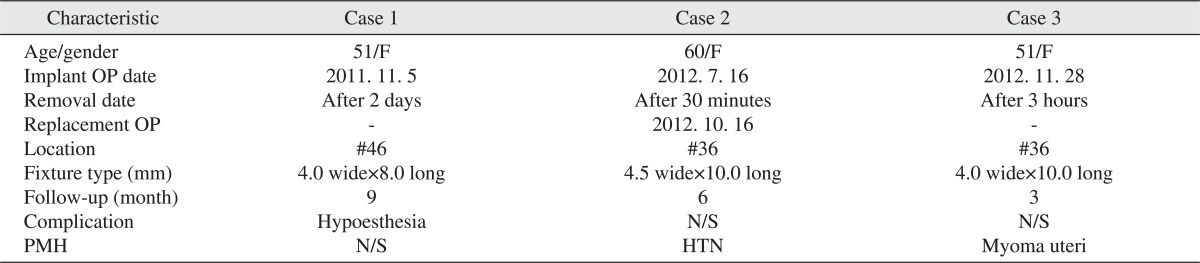
From November 2011 to November 2012, three women were referred to the Department of Oral and Maxillofacial Surgery, Gachon University Gil Medical Center for the management of displacement of dental implants into the posterior mandibular body during implant placement surgery. Detailed information of our patients in this paper are presented in Table 1. The mean age was 54 years (range: 51-60 years). The lesions in our cases were asymptomatic, with no ex pansion of the cortical jawbone detected. A provisional diagnosis of odontogenic cyst or tumor was done, and FOBMD was considered a differential diagnosis based on age, site, and clinical and radiographic findings. Two patients were referred by private dental clinic, with the other patient referred by another Department - Dental Center - of Gachon University Gil Medical Center. All three cases of implant removal surgery were performed by one operator.
A 51-year-old woman with no medical history was referred by a private dental clinic for the management of displacement of implant fixture in the right mandible posterior area on November 7, 2011. Two days earlier, an implant accidentally fell into the mandible body of the #46 area during implant surgery. She complained of hypoesthesia on the right lower lip and chin area. Cone-beam computed tomography (CBCT) imaging of the jaws showed 2.0×0.7 cm radiolucency with quite ill-defined and irregular borders located from the premolar area to the right midbody of the #46, #47 edentulous regions and indicated the implant location to be near the mandibular inferior border area.(Fig. 1. A) Block anesthesia of the right mandibular nerve was administered together with infiltration anesthesia of the surrounding tissues. A mucoperiosteal flap was raised, and a periosteal elevator was placed under the periosteum. Bone osteotomy (1.0×0.5 cm) was performed at the lateral corpus of the mandible with fissure bur and osteotomes. A rectangular cortical bone window was removed. The implant (4.0 mm wide, 8.0 mm long) was exposed and carefully removed without any damage to the mandibular neurovascular bundle. The inner side of the corpus was empty, without any cancellous bone. The osteotomy window was put back to its original position without fixation. The mucoperiosteal flap was replaced and sutured. Postoperatively, a 5-day course of amoxicillin and chlorhexidine rinse was prescribed. The sutures were removed 7 days postoperatively. She complained of hypoesthesia of the right lower lip and chin area during the 9 months' follow-up.(Fig. 1. B)
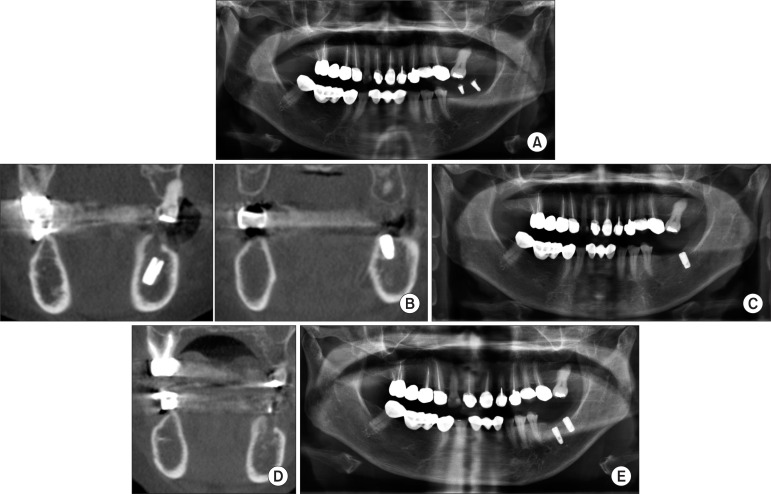
A 60-year-old woman with medical history of hypertension was referred by another department of our dental center for the management of displacement of implant fixture in the left mandible posterior area on July 16, 2012. Thirty minutes earlier, one implant accidentally fell into the mandible body of the #36 area during implant surgery.(Figs. 2. A, 2. B) Note, however, that the #37 implant (4.5 mm wide, 8.0 mm long) placed simultaneously with #36 had good initial stability. CBCT imaging of the jaws showed radiolucency with quite ill-defined and irregular borders located from the premolar area to the left midbody of the #36, #37 edentulous regions and indicated the implant location to be near the mandibular canal.(Fig. 2. B) The removal of implant fixture followed the same procedure as that of case 1. The implant was 4.5 mm wide and 10.0 mm long.(Fig. 2. C) Three months later, replacement of the #36 implant (4.0 mm wide, 10 mm long) was performed with autogenic and xenogenic bone graft.(Fig. 2. E) Bone grafts were made on the upper third portion of the implant. It had three-walled defects, but primary stability was sufficient. Six months after the #37 implant placement and three months after the #36 implant replacement, secondary surgery was performed, followed by the delivery of prosthetics; healing proceeded uneventfully without any postoperative complication.
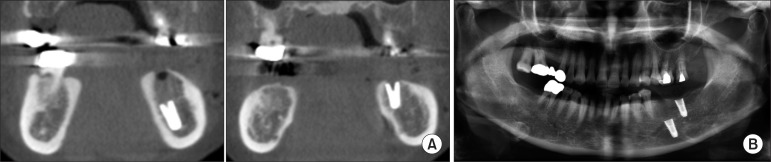
A 51-year-old woman with medical history of myoma uteri was referred by a private dental clinic for the management of displacement of implant fixture in the left mandible posterior area on November 28, 2012. Three hours earlier, one implant accidentally fell into the mandible body of the #36 area during implant surgery.(Figs. 3. A, 3. B) The CBCT image of the jaws showed radiolucency with quite ill-defined and irregular borders located from the premolar area to the left midbody of the #36, #37 edentulous regions and indicated the implant location to be near the mandibular inferior border. The removal of implant fixture followed the same procedure as that of case 1. The implant was 4.0 mm wide and 10.0 mm long. Healing proceeded uneventfully during the 3 months' follow-up.
FOBMD of the jaws has been reported as an unusual radiolucency often detected fortuitously in the posterior mandible of a middle-aged woman2,7-9. Radiographically, this radiolucency varies in size from several millimeters to centimeters in diameter, and the shape and borders are ill-defined with fine central trabeculation1,3,9. The lesion frequently occurs in an edentulous region where tooth extraction was previously performed4,7. The pathogenesis of the lesion is not confirmed. Various theories include the following: aberrant bone regeneration after tooth extraction; persistence of fetal marrow, and; marrow hyperplasia in response to increased demand for erythrocytes9. Some osteoporotic bone marrow defects (OBMDs) are multifocal; others are bilateral, and few of them are symptomatic1-4. More than 75% of all cases are discovered in adult women. About 70% occur in the posterior mandible, often in edentulous areas. No clinical and radiological expansion of the jaw is noted9. According to the study conducted by Shankland and Bouquot4, the bilateral occurrence of OBMD within the jaws affected 3% of patients. Previous OBMDs documented in English literature frequently indicate that the radiographic appearance may be confused with other intraosseous patho-logic conditions1-4,7,8. Mandibular cysts or tumors often have bilateral radiolucency with indistinct margins. Based on age, site, and clinical and radiographic findings, OBMD was considered a differential diagnosis. The final diagnosis of OBMD should be established on microscopic features1,4. Microscopically, the existence of hematopoietic marrow composed of erythroid, monocytic, granulocytic, and lympho-cytic series as well as megakaryocytes associated with fatty marrow is required for the diagnosis of this lesion4,7-9.
FOBMD was considered a differential diagnosis based on age, site, and clinical and radiographic findings without biopsy for all our cases. Radiologically, cortical bone density and thickness were at normal levels; the endosteal cortical margin was even, and there were no cystic epithelial walls.(Figs. 1-3) The cancellous bone marrow was almost absent, and the pattern with hematopoietic marrow tissue was filled roughly. Our CBCT imaging showed the weakness of bone marrow density near the mandibular canal of the molar area.(Figs. 1. A, 2. B, and 3. A) Thus, we diagnosed our 3 patients as FOBMD based on age, site, and clinical and radiographic findings.
TBCs10 of the jaws are asymptomatic cystic lesions detected incidentally on radiographs or during surgery. The lesion is mainly diagnosed among young patients most frequently during the second decade of life, with men affected somewhat more frequently. Expansion of the cortical plate of the jaw bone is often noted, usually buccally, resulting in intraoral and extra-oral swelling. TBC, or extension of the empty bone cavity, will stop expanding once the cortical bone has been reached. A characteristic of TBC is the "scalloping effect" when extending between the roots of the vital teeth10. Preoperatively, we could not detect any radiolucency to confirm diagnosis of TBC radiographically. A histological examination of TBC revealed normal-looking bone spicules with parts of vascular connective tissue. Occasional hemosiderin-laden macrophages were also noted10. Nonetheless, FOBMD frequently occurs in an edentulous region of a middle-aged woman, and a radiolucent appearance is usually not observed on the preoperative panoramic radiograph2. Based on the panoramic view of our patients, we could not detect any cystic lesion on the mandible (Figs. 1. B, 2. B, and 3. B), finding that the cancellous bone marrow was almost nonexistent based on CBCT imaging.(Figs. 1. A, 2. B, and 3. A)
Whether the lesion is TBC or OBMD, the radiolucent appearance of a possible lesion was more likely not observed on the preoperative panoramic radiograph5. Bender and Seltzer11 showed that the removal of cancellous bone from the posterior region of cadaver mandibles did not alter the radiographic appearance of the trabeculae. It was only when the endosteal surface of the cortical bone was removed was the radiographic image altered.
None of our patients had a medical history of osteoporosis. Note, however, that osteoporosis is very common particularly among postmenopausal women. The lesion is characterized by decrease in bone mass and strength5. Vlasiadis et al.12 demonstrated that later postmenopausal date and number of tooth loss were related to higher degree of osteoporosis. Studies of subjects with osteoporosis have shown no differences in the survival of implants compared with healthy subjects; a review of the published data did not find evidence that osteoporosis could be a risk factor for osseointegrated dental implants13. The #37 (4.5 mm wide, 8.0 mm long) implant placed simultaneously with #36 (4.5 mm wide, 10.0 mm long) had good initial stability.(Figs. 2. B, 2. C) Note, however, that only the #36 implant fell down into the mandible body.(Fig. 2B) Three months later, the replacement of the #36 implant (4.0 mm wide, 10 mm long) was performed with autogenic and xenogenic bone graft. The bone grafts were made on the upper third portion of the implant. It had three walled defects, but primary stability was sufficient. Six months after the #37 implant placement and three months after the #36 implant replacement (Fig. 2E), delivery of prosthetics was carried out, and healing proceeded uneventfully without any postoperative complication.
The displacement of an implant will occur intraoperatively or within a short period due to the poor use of surgical technique by an inexperienced operator or anatomical variances. Failure of initial implant stability can result from low trabecular bone density, decreased thickness of the cortical bone, anatomical variances, and osteopenia or osteoporosis; problems related to the use of surgical technique by an inexperienced operator, such as inadequate planning, overworking of the implant drilling, mishandling, and incorrect manipulation, have also been suggested as possible factors5,6. According to Theisen et al.,14 during the tightening of the healing screw, the implant was displaced inferiorly into the preparation, and attempts to remove the screw and retrieve the implant body resulted in the further inferior displacement of the implant body. One case (case 1) exhibited hypoesthesia of lower lip and chin. She already had hypoesthesia on the lower lip when she visited our dental center. Thus, we assumed that the nerve had been damaged when the implant fell down into the mandible.
Although dental implant surgery is considered a simple and predictable procedure, unforeseen complications and rare accidents could occur especially in the posterior segments with lower trabecular bone density than in anterior segments. As previously reported by Theisen et al.,14 when the location of the inferior alveolar canal could not be delineated on a panoramic radiograph, large medullary components could be detected on the CT section. Thus, additional radiographic evaluations such as preoperative CT may be necessary for patients whose molar teeth were extracted much earlier in their life, particularly among postmenopausal women. Operators should take care against implant displacement into FOBMD. We recommend securing the healing screw in the implant body prior to the placement of the implants. Even if implants fall down into FOBMD, removal of the implants was performed carefully without any damage to nerve and vessel bundles, and replacement of implants was done as a common method of immediate placement after teeth extraction. Nonetheless, additional studies with more cases and long-term follow-up should be conducted.
References
1. Schneider LC, Mesa ML, Fraenkel D. Osteoporotic bone marrow defect: radiographic features and pathogenic factors. Oral Surg Oral Med Oral Pathol. 1988; 65:127–129. PMID: 3277106.

2. Bravo-Calderón DM, Oliveira DT, Martins Dos Santos WH. Bilateral osteoporotic bone marrow defects of the mandible: a case report. Head Face Med. 2012; 8:22. PMID: 22873712.

3. Lipani CS, Natiella JR, Greene GW Jr. The hematopoietic defect of the jaws: a report of sixteen cases. J Oral Pathol. 1982; 11:411–416. PMID: 6819349.

4. Shankland WE, Bouquot JE. Focal osteoporotic marrow defect: report of 100 new cases with ultrasonography scans. Cranio. 2004; 22:314–319. PMID: 15532316.
5. Bayram B, Alaaddinoglu E. Implant-box mandible: dislocation of an implant into the mandible. J Oral Maxillofac Surg. 2011; 69:498–501. PMID: 21238846.

6. Lamas Pelayo J, Peñarrocha Diago M, Martí Bowen E, Peñarrocha Diago M. Intraoperative complications during oral implantology. Med Oral Patol Oral Cir Bucal. 2008; 13:E239–E243. PMID: 18379448.
7. Makek M, Lello GE. Focal osteoporotic bone marrow defects of the jaws. J Oral Maxillofac Surg. 1986; 44:268–273. PMID: 3457122.

8. Sencimen M, Delilbasi C, Gulses A, Okcu KM, Gunhan O, Varol A. Focal osteoporotic hematopoietic bone marrow defect formation around a dental implant: a case report. Int J Oral Maxillofac Implants. 2011; 26:e1–e4. PMID: 21365033.
9. CHI AC. Bone pathology. In : Neville BW, Damm DD, Allen CM, Bouquot JE, editors. Oral and maxillofacial pathology. 3rd ed. St. Louis: Saunders-Elsevier;2009. p. 613–677.
10. Xanthinaki AA, Choupis KI, Tosios K, Pagkalos VA, Papanikolaou SI. Traumatic bone cyst of the mandible of possible iatrogenic origin: a case report and brief review of the literature. Head Face Med. 2006; 2:40. PMID: 17096860.

11. Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: I. 1961. J Endod. 2003; 29:702–706. PMID: 14651274.
12. Vlasiadis KZ, Skouteris CA, Velegrakis GA, Fragouli I, Neratzoulakis JM, Damilakis J, et al. Mandibular radiomorphometric measurements as indicators of possible osteoporosis in postmenopausal women. Maturitas. 2007; 58:226–235. PMID: 17923346.

13. Grant BT, Amenedo C, Freeman K, Kraut RA. Outcomes of placing dental implants in patients taking oral bisphosphonates: a review of 115 cases. J Oral Maxillofac Surg. 2008; 66:223–230. PMID: 18201600.

14. Theisen FC, Shultz RE, Elledge DA. Displacement of a root form implant into the mandibular canal. Oral Surg Oral Med Oral Pathol. 1990; 70:24–28. PMID: 2196504.

Fig. 1
A. Preoperative coronal (left) and sagittal (right) cone-beam computed tomography showing the displacement of the #46 implant near the mandibular border of case 1. B. Follow-up panorama taken 3 months after the removal operation indicates the resolution of the lesion on the #46 area.
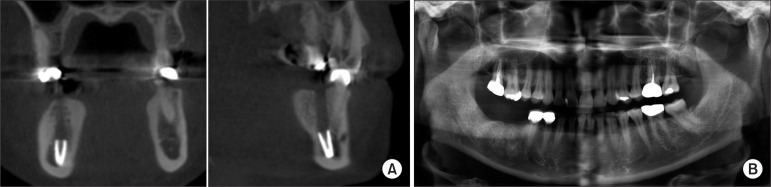
Fig. 2
A. Preoperative panorama showing normal bone on the left mandibular body without any cystic lesion of case 2. B. Preoperative cone-beam computed tomography showing the displacement of #36 implant (left) near the inferior alveolar nerve and normal position of #37 implant (right) of case 2. C. Postoperative panoramic view of #36 implant removal surgery of case 2. D. Follow-up computed tomography taken 3 months after the removal operation indicates the resolution of the lesion of case 2. E. Follow-up panoramic view after the placement of # 36 implant of case 2.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download