Abstract
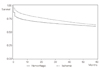
Stroke is the most common cause of death as single-diseases in South Korea. And it generates additional medical cost through high incidence of related disabilities and complications, which would become more important with the rapid aging process in Korean society. This study was preformed to identify stroke patients' mortality and its associated factors. Patients diagnosed as stroke (ICD-10 code I60-I63) in 2003 were identified. Their follow-up mortality rate in 5 years and related factors (stroke type, sex, age, type of first admission hospital, comorbidity score) were analyzed using national health insurance claim data and national cause of death statistics. The mortality rate peaked in early days after attack, and decreased subsequently as the survive time gets longer. The mortality rate was higher in hemorrhagic stroke than ischemic stroke, in female than male, with the older age, and with the higher comorbidity score. It is recommended that the early intervention at general hospital or tertiary referral hospital should be promoted to decrease the mortality rate in stroke patients, and related quality assurance programs have to be enforced.
Figures and Tables
Acknowledgment
This study was supported by Health Insurence Review & Assessment Institute, Health Insurance Review & Assessment Service, Seoul, Korea.
References
1. Health Insurance Review and Assessment Service. Report on adequacy for stroke. 2007. Seoul: Health Insurance Review and Assessment Service.
2. Thrift AG, Dewey HM, Sturm JW, Srikanth VK, Gilligan AK, Gall SL, Macdonell RA, McNeil JJ, Donnan GA. Incidence of stroke subtypes in the North East Melbourne Stroke Incidence Study (NEMESIS): differences between men and women. Neuroepidemiology. 2009. 32:11–18.

3. Sarti C, Stegmayr B, Tolonen H, Mahonen M, Tuomilehto J, Asplund K. Are changes in mortality from stroke caused by changes in stroke event rates or case fatality? Results from the WHO MONICA Project. Stroke. 2003. 34:1833–1840.

4. Bian J, Dow WH, Matchar DB. Medicare HMO penetration and mortality outcomes of ischemic stroke. Am J Manag Care. 2006. 12:58–64.
5. Hallstrom B, Jonsson AC, Nerbrand C, Norrving B, Lindgren A. Stroke incidence and survival in the beginning of the 21st century in southern Sweden: comparisons with the late 20th century and projections into the future. Stroke. 2008. 39:10–15.

6. Andersen HE, Schultz-Larsen K, Kreiner S, Forchhammer BH, Eriksen K, Brown A. Can readmission after stroke be prevented? Results of a randomized clinical study: a postdischarge follow-up service for stroke survivors. Stroke. 2000. 31:1038–1045.
7. Brainin M, Bornstein N, Boysen G, Demarin V. Acute neurological stroke care in Europe: results of the European Stroke Care Inventory. Eur J Neurol. 2000. 7:5–10.

8. Bushnell CD, Lee J, Duncan PW, Newby LK, Goldstein LB. Impact of comorbidities on ischemic stroke outcomes in women. Stroke. 2008. 39:2138–2140.

9. Widen Holmqvist L, von Koch L, Kostulas V, Holm M, Widsell G, Tegler H, Johansson K, Almazan J, de Pedro-Cuesta J. A randomized controlled trial of rehabilitation at home after stroke in southwest Stockholm. Stroke. 1998. 29:591–597.

10. Rundek T, Nielsen K, Phillips S, Johnston KC, Hux M, Watson D. Health care resource use after acute stroke in the Glycine Antagonist in Neuroprotection (GAIN) Americas trial. Stroke. 2004. 35:1368–1374.

11. Ytterberg C, Anderson Malm S, Britton M. How do stroke patients fare when discharged straight to their homes? A controlled study on the significance of hospital follow-up after one month. Scand J Rehabil Med. 2000. 32:93–96.

12. Johnston KC, Li JY, Lyden PD, Hanson SK, Feasby TE, Adams RJ, Faught RE Jr, Haley EC Jr. Medical and neurological complications of ischemic stroke: experience from the RANTTAS trial. RANTTAS Investigators. Stroke. 1998. 29:447–453.

13. Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P. Impact of functional status at six months on long term survival in patients with ischemic stroke: prospective cohort studies. BMJ. 2008. 336:376–379.

14. Kim SH, Lee YS, Lee SM, Yoon BW, Park BJ. Body mass index and risk of hemorrhagic stroke in Korean adults: case-control study. J Prev Med Public Health. 2007. 40:313–320.

15. Kim JH, Lim NY, So HY, Kang KS, Min HS, Park GH, Park SY, Cho BH, Han HS, Kim SY. An analysis on the research papers about exercise interventions to the stroke survivors. Korean J Rehabil Nurs. 2007. 10:116–124.
16. Park GO, Shin SJ. Activities of daily living and fatigue in the stroke patients. Korean J Rehabil Nurs. 2010. 13:23–31.
17. Park SY. The effects of exercise on functional status, activity of daily living and social re-adjustment in stroke patients. Korean J Rehabil Nurs. 2007. 10:12–20.
18. Lee KW, Ha MK, Ha KS, Kim RB, Park KS. The association of social support and quality of life of stroke patients in a city. J Agric Med Community Health. 2010. 35:46–55.

19. Jang IS, Han JY, Choi IS, Lee SG, Kim IG, Lee MK. Influence of the initial readings of blood pressure components on functional outcome in acute ischemic stroke patients. J Korean Geriatr Soc. 2009. 13:128–134.

22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998. 36:8–27.

23. Kaplan MH, Feinstein AR. The importance of classifying initial co-morbidity in evaluating the outcome of diabetes mellitus. J Chronic Dis. 1974. 27:387–404.

24. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987. 40:373–383.

25. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004. 57:1288–1294.

26. Kolominsky-Rabas PL, Heuschmann PU, Marschall D, Emmert M, Baltzer N, Neundorfer B, Schoffski O, Krobot KJ. Lifetime cost of ischemic stroke in Germany: results and national projections from a population-based stroke registry: the Erlangen Stroke Project. Stroke. 2006. 37:1179–1183.

27. Bravata DM, Ho SY, Meehan TP, Brass LM, Concato J. Readmission and death after hospitalization for acute ischemic stroke: 5-year follow-up in the medicare population. Stroke. 2007. 38:1899–1904.

28. Andersen KK, Andersen ZJ, Olsen TS. Predictors of early and late case-fatality in a nationwide danish study of 26 818 patients with first-ever ischemic stroke. Stroke. 2011. 42:2806–2812.

29. Goulart AC, Bensenor IM, Fernandes TG, Alencar AP, Fedeli LM, Lotufo PA. Early and one-year stroke case fatality in Sao Paulo, Brazil: applying the World Health Organization's stroke STEPS. J Stroke Cerebrovasc Dis. 2011. 06. 24. [Epub]. http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2011.04.017.

30. Marsden DL, Spratt NJ, Walker R, Barker D, Attia J, Pollack M, Parsons MW, Levi CR. Trends in stroke attack rates and case fatality in the Hunter region, Australia 1996-2008. Cerebrovasc Dis. 2010. 30:500–507.

31. Burke TA, Venketasubramanian RN. The epidemiology of stroke in the East Asian region: a literature-based review. Int J Stroke. 2006. 1:208–215.

32. Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003. 2:43–53.

33. Bejot Y, Rouaud O, Durier J, Caillier M, Marie C, Freysz M, Yeguiayan JM, Chantegret A, Osseby G, Moreau T, Giroud M. Decrease in the stroke case fatality rates in a French population-based twenty-year study: a comparison between men and women. Cerebrovasc Dis. 2007. 24:439–444.

34. Turin TC, Kita Y, Rumana N, Nakamura Y, Takashima N, Ichikawa M, Sugihara H, Morita Y, Hirose K, Okayama A, Miura K, Ueshima H. Is there any circadian variation consequence on acute case fatality of stroke? Takashima Stroke Registry, Japan (1990-2003). Acta Neurol Scand. 2011. 05. 26. [Epub]. http://dx.doi.org/10.1111/j.1600-0404.2011.01522.x.

35. Minelli C, Fen LF, Minelli DP. Stroke incidence, prognosis, 30-day, and 1-year case fatality rates in Matao, Brazil: a population-based prospective study. Stroke. 2007. 38:2906–2911.

36. Kim CG, Park HA. Predictors of in-hospital death of stroke patients regarding the demographics and previous medical illness. Korean J Stroke. 2006. 8:179–186.
37. Stroke Risk in Atrial Fibrillation Working Group. Comparison of 12 risk stratification schemes to predict stroke in patients with nonvalvular atrial fibrillation. Stroke. 2008. 39:1901–1910.
38. Niewada M, Kobayashi A, Sandercock PA, Kaminski B, Czlonkowska A. Influence of gender on baseline features and clinical outcomes among 17,370 patients with confirmed ischemic stroke in the international stroke trial. Neuroepidemiology. 2005. 24:123–128.

39. Olsen TS, Dehlendorff C, Andersen KK. Sex-related timedependent variations in post-stroke survival-evidence of a female stroke survival advantage. Neuroepidemiology. 2007. 29:218–225.

40. Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, Khatiwoda A, Lisabeth L. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008. 7:915–926.

41. Conforto AB, Paulo RB, Patroclo CB, Pereira SL, Miyahara Hde S, Fonseca CB, Yamamoto FI, Marchiori PE, Evaristo EF, Scaff M. Stroke management in a university hospital in the largest South American city. Arq Neuropsiquiatr. 2008. 66:308–311.

42. Howard VJ, Acker J, Gomez CR, Griffies AH, Magers W, Michael M 3rd, Orr SR, Phillips M, Raczynski JM, Searcy JE, Zweifler RM, Howard G. An approach to coordinate efforts to reduce the public health burden of stroke: the Delta States Stroke Consortium. Prev Chronic Dis. 2004. 1:A19.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download