Abstract
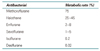
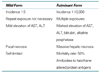
The liver is the major site of endogenous and exogenous drug metabolism. The primary result of drug metabolism is the production of more water-soluble and therefore more easily excreted drug metabolites. Drugs are sometimes biotransformed into more reactive metabolites, which may lead to toxicity. Volatile anesthetics, like most drugs, undergo metabolism in the body and are sometimes associated with toxic reactions. Here, author will discuss the metabolism and hepatic toxicity of inhaled anesthetics. Toxicity and liver injury have been reported after repeated exposure on subsequent occasions to different fluorinated anesthetics. This phenomenon of cross-sensitization has also been reported with the chlorofluorocarbon(CFC) replacement agents, the hydrochlorofluorocarbons(HCFCs). Halothane, enflurane, sevoflurane, isoflurane, desflurane are all metabolized to trifluoroacetic acid, which have been reported to induce liver injury in susceptible patients. The propensity to produce liver injury appears to parrel metabolism of the parent drug: halothane(20%) >>>> enflurane(2.5%) >> sevoflurane(1%) > isoflurane(0.2%) > desflurane(0.02%). The use of any anesthetic must be based on its benefits and risks, how it may produce toxicity, and in which patients it may be most safely administered. Nonhalogenated inhaled anesthetics (nitrous oxide, xenon) chemically inert and not metabolized in human tissue. The perfect anesthetic agents dose not exist. But ongoing research attempts to uncover emerging toxicities. Xenon is not currently approved for clinical use. Other than the expense associated with its use, it may be the most ideal anesthetic agent. In general, surgical manipulation or disturbance of the surgical site appears to be more important in decreasing hepatic blood flow than current anesthetic agents such as isoflurane, sevoflurane, and desflurane or technique. However, the clinician is challenged to balance new information with current clinical practices and choice the safest, most effective agents for each patient.
References
1. Krishna DR, Klotz U. Extrahepatic metabolism of drugs in humans. Clinical Pharmacokinet. 1994. 26:144–160.

2. Wilkinson G. Hardmann JG, Limbrid LE, Goodman GA, editors. Pharmacokinetics. The dynamics of drug absorption, distribution and elimination. Goodman and Gilman's the Pharmacological Basis of Therapeutics. 2001. 10th ed. New York: McGraw-Hill.
3. Gibson GG, Skett P. Introduction to drug metabolism. 1999. Chelteham, UK: Stanley, Thornes Publishers.
4. Banks RGS, Henderson RJ, Pratt JM. Reactions of gases in solution. Some reactions of nitrous with transition metal complexes. J Chem Soc. 1968. 3:Suppl A. 2886.
5. Amess JA, Burman JF, Ree GM, Nancekievill DG, Mollin DL. Megaloblastic haemopoiesis in patients receiving nitrous oxide. Lancet. 1978. 12:339–342.
6. Van Dyke RA. Chenoweth MB, editor. Biotransformation. Handbook of Experimental pharmacology. 1972. New York: Springer-Verlag;354.
7. Rao GS, Meridian DJ, Tong YS. Biochemical toxicology of chronic nitrous oxide exposures. Pharmacologist. 1979. 21:216.
8. Rice SA, Mazze RI, Baden JM. Effects of subchronic intermittent exposure to nitrous oxide in Swiss Webster mice. J Environ Pathol Toxicol Oncol. 1985. 6:271–281.
9. Cullen SC, Gross EG. The anesthetic properties of xenon in animals and human beings, with additional observations on krypton. Science. 1951. 113:580–582.

10. Morris LE, Knott JR, Pittinger CB. Electroencephalographic and blood gas observations in human surgical patients during xenon anesthesia. Anesthesiology. 1955. 16:312–319.

11. Lachmann B, Armbruster S, Schairer W, Landstra M, Trouwborst A, Van Daal GJ, et al. Safety and efficacy of xenon in routine use as an inhalational anaesthetic. Lancet. 1990. 335:1413–1415.

12. Luttropp HH, Thomasson R, Dahm S, Persson J, Werner O. Clinical experience with minimal flow xenon anesthesia. Acta Anaesthesiol Scand. 1994. 38:121–125.

13. Hofland J, Gultuna I, Tenbrinck R. Xenon anaesthesia for laparoscopic cholecystectomy in a patient with Eisenmenger's syndrome. Br J Anaesth. 2001. 86:882–886.

14. Burov NE, Molchanov IV, Nikolaev LL, Rashchupkin AB. [The method of low-flow xenon anesthesia]. Anesteziol Reanimatol. 2003. 3:31–34.
15. Goto T, Saito H, Shinkai M, Nakata Y, Ichinose F, Morita S. Xenon provides faster emergence from anesthesia than does nitrous oxide-sevoflurane or nitrous oxide-isoflurane. Anesthesiology. 1997. 86:1273–1278.

16. Rossaint R, Reyle-Hahn M, Schulte AM Esch J, Scholz J, Scherpereel P, Vallet B, et al. Multicenter randomized comparison of the efficacy and safety of xenon and isoflurane in patients undergoing elective surgery. Anesthesiology. 2003. 98:6–13.

17. Froeba G, Marx T, Pazhur J, Baur C, Baeder S, Calzia E, et al. Xenon does not trigger malignant hyperthermia in susceptible swine. Anesthesiology. 1999. 91:1047–1052.

18. Zhang P, Ohara A, Mashimo T, Imanaka H, Uchiyama A, Yoshiya I. Pulmonary resistance in dogs: A comparison of xenon with nitrous oxide. Can J Anaesth. 1995. 42:547–553.

19. Kharasch ED, Hankins DC, Fenstamaker K, Cox K. Human halothane metabolism, lipid peroxidation, and cytochromes P(450)2A6 and P(450)3A4. Eur J Clin Pharmacol. 2000. 55:853–859.

20. Brody GL, Sweet RB. Halothane anesthesia as a possible cause of massive hepatic necrosis. Anesthesiology. 1963. 24:29–37.

21. Subcommittee on the National Halothane Study of the Committee on Anesthesia. National Academy of Sciences: National Research Council. Summary of the National Halothane Study. Possible association between halothane anesthesia and postoperative necrosis. JAMA. 1966. 197:775–788.
23. Pohl LR. An immunochemical approach of identifying and characterizing protein targets of toxic reactive metabolites. Chem Res Toxicol. 1993. 6:786–793.

24. Joshi PH, Conn HO. The syndrome of methoxyflurane associated hepatitis. Ann Intern Med. 1974. 80:395–401.
25. Cousins MJ, Mazze RI. Methoxyflurane nephrotoxicity: A study of dose response in man. JAMA. 1973. 225:1611–1616.

26. Eger EI II, Smuckler EA, Ferrell LD, Goldsmith CH, Johnson BH. Is enflurane hepatotoxic? Anesth Analg. 1986. 65:21–30.
27. Sigurdsson J, Hreidarsson AB, Thjodleifsson B. Enflurane hepatitis: A report of a case with a previous history of halothane hepatitis. Acta Anaesthesiol Scand. 1985. 29:495–496.

28. Christ DD, Kenna JG, Kammerer W, Satoh H, Pohl LR. Enflurane metabolism produces covalently bound liver adducts recognized by antibodies from patients with halothane hepatitis. Anesthesiology. 1988. 69:833–838.

29. Stoelting RK, Blitt CD, Cohen PJ, Merin RG. Hepatic dysfunction after isoflurane anesthesia. Anesth Analg. 1987. 66:147–153.

30. Brunt EM, White H, Marsh JW, Holtmann B, Peters MG. Fulminant hepatic failure after repeated exposure to isoflurane anesthesia: A case report. Hepatology. 1991. 13:1017–1021.

31. Turner GB, O'Rourke D, Scott GO, Beringer TR. Fatal hepatotoxicity after re-exposure to isoflurane: A case report and review of the literature. Eur J Gastroenterol Hepatol. 2000. 12:955–959.

32. Njoku DB, Shrestha S, Soloway R, Duray PR, Tsokos M, Abu-Asab MS, et al. Subcellular localization of trifluoroacetylated liver proteins in association with hepatitis following isoflurane. Anesthesiology. 2002. 96:757–761.

33. Jones RM, Koblin DD, Cashman JN, Eger EI II, Johnson BH, Damask MC. Biotransformation and hepato-renal function in volunteers after exposure to desflurane (I-653). Br J Anaesth. 1990. 68:482–487.
34. Wrigley SR, Fairfield JE, Jones RM, Black AE. Induction and recovery characteristics of desflurane in day case patients: A comparison with propofol. Anaesthesia. 1991. 46:615–622.

35. Eger EI II, Johnson BH, Strum DP, Ferrell LD. Studies of the toxicity of I-653, halothane, and isoflurane in enzyme induced, hypoxic rat. Anesth Analg. 1987. 66:1227–1229.
36. Martin JL, Plevak DJ, Flannery KD, Charlton M, Poterucha JJ, Humphreys CE, et al. Hepatotoxicity after desflurane anesthesia. Anesthesiology. 1995. 83:1125–1129.

37. Berghaus TM, Baron A, Geier A, Lamerz R, Paumgartner G. Hepatotoxicity following desflurane anesthesia. Hepatology. 1999. 29:613–614.

38. Gonsowiski CT, Laster MJ, Eger EI II, Ferrell LD, Kerschmann RL. Toxicity of compound A in rats. Anesthesiology. 1994. 80:556–565.

39. Keller KA, Callan C, Prokocimer P, Delgado-Herrera L, Friedman MB, Hoffman GM, et al. Inhalation toxicity study of a haloalkene degradant of sevoflurane, compound A (PIFE), in Sprague-Dawley rats. Anesthesiology. 1995. 83:1220–1232.

40. Goldberg ME, Cantillo J, Gratz I, Deal E, Vekeman D, McDougall R, et al. Dose of compound A, not sevoflurane, determines changes in the biochemical markers of renal injury in healthy volunteers. Anesth Analg. 1999. 88:437–445.

41. Ebert TJ, Messana LD, Uhrich TD, Staacke TS. Absence of renal and hepatic toxicity after four hours of 1.25 minimum alveolar anesthetic concentration sevoflurane anesthesia in volunteers. Anesth Analg. 1998. 86:662–667.

42. Watanabe K, Hatakenaka S, Ikemune K, Chigyo Y, Kubozone T, Arai T. A case of suspected liver dysfunction induced by sevoflurane anesthesia. Masui. 1993. 42:902–905.
43. Shichinohe Y, Masuda Y, Takahashi H, Kotaki M, Omoto T, Shichinohe M, et al. A case of postoperative hepatic injury after sevoflurane anesthesia. Masui. 1992. 41:1802–1805.
44. Bruun LS, Elkjaer S, Bitsch-Larsen D, Andersen O. Hepatic failure in a child after acetaminophen and sevoflurane exposure. Anesth Analg. 2001. 92:1446–1448.

45. Frink EJ Jr, Ghantous H, Malan TP, Morgan S, Fernando J, Gandolfi AJ, et al. Plasma inorganic fluoride with sevoflurane anesthesia: Correlation with indices of hepatic and renal function. Anesth Analg. 1992. 74:231–235.
46. Ray DC, Bomont R, Mizushima A, Kugimiya T, Forbes Howie A, Beckett GJ. Effect of sevoflurane anesthesia on plasma concentrations of glutathione S-transferase. Br J Anaesth. 1996. 77:404–407.

47. Taivainen T, Tiainen P, Meretoja OA, Raiha L, Rosenberg PH. Comparison of the effects of sevoflurane and halothane on the quality of anaesthesia and serum glutathione transferase alpha and fluoride in paediatric patients. Br J Anaesth. 1994. 73:590–595.

48. Lynch S, Martis L, Woods E. Evaluation of hepatotoxic potential of sevoflurane in rats. Pharmacologist. 1979. 21:221.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download