This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
The purpose of this retrospective study was to investigate the relationships of types of dental insurance coverage in Korea with sociodemographic characteristics and the prevalence of systemic and oral diseases, as well as to evaluate the socioeconomic impact of Korean dental insurance policies.
Methods
Sample cohort data from 2006 to 2015 were obtained from the National Health Insurance Service. Patients were divided into 2 groups. The exposed group comprised patients who received insurance benefits for complete dentures, removable partial dentures, and implant care, while the control group comprised patients who did not receive these benefits. The type of insurance coverage and the prevalence of systemic and oral diseases were compared between the 2 groups.
Results
Patients who received benefits in the form of complete dentures, removable partial dentures, and implants had similar sociodemographic characteristics in terms of sex, age, income quintile, and type of insurance coverage to the control group. The prevalence of hypertension, anemia, renal disease, rheumatoid arthritis, osteoporosis, asthma, and cerebral infarction was higher in the exposed group than in the control group (P<0.05). The prevalence of periodontal diseases and dental caries was also higher in the exposed group.
Conclusions
Korean dental health insurance policy has been beneficial for the medical expenses of low-income and elderly people suffering from a cost burden due to systemic diseases. However, since there is a tendency to avoid invasive interventions in older patients due to the high risk of systemic diseases, insurance coverage of dentures may be more helpful from a socioeconomic perspective than coverage of dental implant treatments.
Keywords: Dentures, Dental implants, Health insurance, Insurance benefits, Health services for the aged
INTRODUCTION
Population aging due to increases in life expectancy and low birth rates is a major social issue in South Korea. Growing concerns about poverty and illness among the elderly prompted the Ministry of Health and Welfare to implement long-term-care insurance for the elderly in 2009, and various welfare and health policy studies have been conducted to assess the effects of those policy changes [
12].
The socioeconomic cost of dental expenses is steadily increasing due to the aging population. The number of Korean patients treated for periodontal disease reached 14 million in 2017, with total costs of medical care exceeding 1.1 trillion Korean won [
3]. In addition, 5.9 million people received medical care for dental caries, at a total cost of about 590 billion Korean won. Untreated dental caries or periodontal disease can lead to the loss of teeth, which can adversely affect nutrition and the socioeconomic activities of the elderly, thereby threatening the health of the entire body [
4]. Oral reconstruction is therefore a prerequisite for improving quality of life in the elderly and ensuring that they remain healthy. However, this is associated with a large cost burden, which makes it especially difficult to implement in elderly patients.
The Korean National Health Insurance Service (NHIS) now provides insurance for oral reconstruction procedures including complete dentures, removable partial dentures, and dental implants. Complete denture insurance coverage has been provided for edentulous patients older than 75 years since July 1, 2012, and insurance coverage for removable partial dentures was introduced in July 2013. The scope of the insurance policy was expanded to include dental implants in July 2014. Elderly people older than 70 years were included in July 2015, and people older than 65 years were included in July 2016. Moreover, the copayments for dentures and implants were reduced from 50% to 30% in November 2017 and July 2018, respectively [
34]. These policy changes are expected to reduce the socioeconomic burden of dental treatment on the elderly population and to help prevent simple dental diseases in South Korea. However, there are some limitations of this policy. In cases of complete and removable partial dentures, the insurance does not cover the reworking of dentures for 7 years after the first procedure, so that patients are required to pay the entire cost for the reworking of dentures if the dentures break or if remaining teeth are extracted within 7 years after receiving the first benefit. The insurance benefit for dental implants only covers up to 2 implants during an individual's lifetime. This means that patients with more than 2 missing teeth do not receive sufficient support from the policy.
This study used sample cohort data from the NHIS to investigate the relationships of types of dental insurance coverage in Korea with sociodemographic characteristics and the prevalence of systemic and oral diseases, as well as to evaluate the socioeconomic impact of Korean dental insurance policies.
MATERIALS AND METHODS
This retrospective cohort study evaluated data from sample subjects in the NHIS database in South Korea. Patients aged ≥65 years who received insurance benefits between 2006 and 2015 were extracted as the exposed group from the database using the procedure codes for complete dentures, removable partial dentures, and dental implants. The control group comprised randomly extracted patients aged ≥65 years who did not receive insurance benefits. The sample subjects represented all enrollees in the NHIS, which consisted of 2 sex groups, 18 age groups, and 41 groups of South Korean citizens categorized by insurance type and income quintile. The insurance type was divided into Medical Aid, employee-insured, and self-employed insured, and a distinction was made between heads of household and dependents. Income quintiles were defined according to quarterly income, with the first quintile corresponding to the lowest income level and higher quintiles including higher income levels.
The analyzed data included sex, age, insurance type, income quintile, systemic diseases, and oral diseases. Systemic diseases and oral diseases were identified based on diagnostic codes, with oral diseases including periodontal diseases and dental caries. Some diseases, such as dementia, were not identified in order to ensure the privacy of the subjects.
The exposed group was divided into 3 separate exposed groups according to whether they received complete dentures, removable partial dentures, or dental implants. In order to confirm the sociodemographic relevance of the control group, the frequencies of claims differentiated according to sex, age, income quintile, and insurance type were determined. The sociodemographic characteristics of the control group were not analyzed, because the sample subjects were extracted from groups evenly divided according to sex, age, insurance type and income quintile. The prevalence systemic diseases and oral diseases were compared between the exposed groups and the control group using the chi-square test. The criterion for statistical significance was P<0.05. All analyses were performed using SAS software (version 9.4, SAS Institute, Cary, NC, USA).
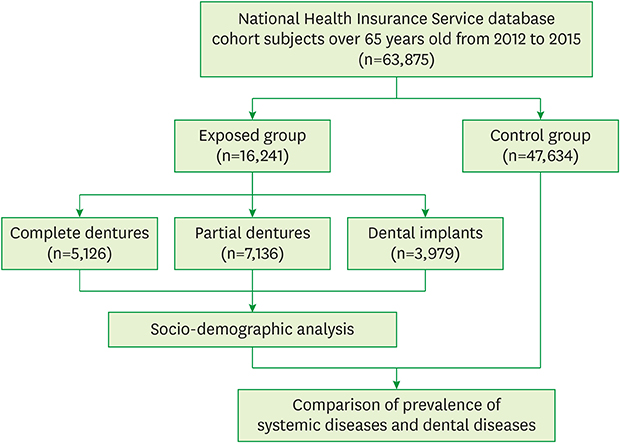
The overall flowchart of this study is presented in
Figure 1.
Figure 1
Flowchart of the selection and analysis of patients from the National Health Insurance Service database.

The study protocol was reviewed and approved by the Institutional Review Board of National Health Insurance Service Ilsan Hospital, South Korea (NHIMC IRB No. 2017-01-010).
RESULTS
From 2012 to 2015, there were 63,875 patients older than 65 years in the sample cohort, comprising 23,505 men and 40,370 women. Insurance benefits related to dental prostheses was provided to 16,241 patients, covering complete dentures in 5,126 patients, removable partial dentures in 7,136, and implants in 3,979.
Figure 2 shows the number of patients who received insurance benefits over 6-month intervals. Insurance coverage for complete resin dentures, removable partial dentures, and dental implants was introduced in July 2012, July 2013, and July 2014, respectively. The subjects were initially restricted to those older than 75 years, but in July 2015 coverage was extended to patients older than 65 years for complete and removable partial dentures, and to patients older than 70 years for dental implants. There were fewer patients receiving insurance benefits for complete dentures than for removable partial dentures at each time point, and the number decreased significantly as the age limit for dental implant coverage decreased. The number of patients receiving insurance benefits for dental implants in the second half of 2015 was 3.7-fold higher than that in the first half of 2015.
Figure 2
Numbers of patients receiving insurance benefits for oral rehabilitation.
Table 1 presents the sociodemographic characteristics of the exposed groups. Fewer male than female patients received complete and removable partial denture coverage, but there was no significant difference by sex. There was no significant difference in the number of male and female patients in the dental implant group.
Table 1
Sociodemographic characteristics of the exposed groups (n = 16,241)

|
Sociodemographic characteristic |
Complete dentures (n=5,126) |
Partial dentures (n=7,136) |
Dental implants (n=3,979) |
|
No. (%) |
P
|
No. (%) |
P
|
No. (%) |
P
|
|
Sex |
|
0.5284 |
|
0.2388 |
|
0.3756 |
|
Male |
1,945 (37.95) |
2,814 (39.43) |
1,945 (48.88) |
|
Female |
3,181 (62.06) |
4,322 (60.56) |
2,034 (51.12) |
|
Age (yr) |
|
<0.0001 |
|
<0.0001 |
|
<0.0001 |
|
70–75 |
142 (2.77) |
1,073 (15.04) |
1,639 (41.19) |
|
75–80 |
4,914 (95.86) |
6,028 (84.47) |
2,339 (58.78) |
|
80 or older |
70 (1.37) |
35 (0.49) |
1 (0.03) |
|
Income quintile |
|
0.0782 |
|
0.0032 |
|
0.0716 |
|
First |
647 (12.62) |
893 (12.51) |
465 (11.69) |
|
Second |
471 (9.18) |
636 (8.92) |
270 (6.79) |
|
Third |
626 (12.21) |
846 (11.86) |
426 (10.71) |
|
Fourth |
924 (18.03) |
1,306 (18.30) |
770 (19.35) |
|
Fifth |
1,899 (37.04) |
2,801 (39.25) |
1,911 (48.03) |
|
Missing |
559 (10.91) |
654 (9.16) |
137 (3.44) |
|
Social security type |
|
0.0048 |
|
<0.0001 |
|
0.0436 |
|
Medical Aid Head of household (Medical Aid beneficiaries) |
861 (16.80) |
1,158 (16.23) |
816 (20.51) |
|
Dependents of Medical Aid beneficiaries |
486 (9.48) |
552 (7.73) |
318 (7.99) |
|
Employee-insured |
73 (1.42) |
186 (2.61) |
316 (7.94) |
|
Dependents of the insured employee |
3,192 (62.28) |
4,652 (65.19) |
2,407 (60.49) |
|
Self-employed insured |
461 (8.99) |
531 (7.44) |
97 (2.44) |
|
Dependents of the self-employed insured |
53 (1.03) |
57 (0.80) |
25 (0.63) |
The insurance benefits for each type of prosthetic treatment were provided most frequently to patients between 75 and 80 years of age, and the number of patients receiving insurance benefits differed significantly among the 3 age groups in all exposed groups. Patients aged 70–75 years received insurance coverage more often for dental implants than for complete dentures.
A trend was observed for higher income levels to be associated with more patients receiving insurance benefits. Patients in the fifth income quintile accounted for 48.03% of those in the dental implant group. However, the difference was statistically significant only in the removable partial denture group.
Heads of household who were Medical Aid beneficiaries received more benefits than their dependents, the dependents of insured employees received more benefits than the heads of households, and the self-employed insured received more benefits than their dependents.
Table 2 lists the prevalence, odds ratios (ORs), and significance levels (
P values) of systemic diseases in the exposed and control groups.
Table 2
Prevalence of systemic diseases in the exposed and control groups

|
Systemic disease |
Complete dentures |
Partial dentures |
Dental implants |
Control group (%) |
P
|
|
% |
OR |
P
|
% |
OR |
P
|
% |
OR |
P
|
|
Hypertension |
71.9 |
1.32 |
<0.0001 |
72.0 |
1.32 |
<0.0001 |
66.7 |
1.03 |
0.4106 |
66.1 |
<0.0001 |
|
Diabetes |
35.0 |
0.99 |
0.7884 |
38.0 |
1.13 |
<0.0001 |
38.1 |
1.13 |
0.0002 |
35.2 |
0.0010 |
|
Anemia |
15.6 |
1.37 |
<0.0001 |
13.6 |
1.18 |
<0.0001 |
11.1 |
0.93 |
0.1471 |
11.8 |
<0.0001 |
|
Renal disease |
5.3 |
1.23 |
0.0015 |
4.9 |
1.14 |
0.0248 |
3.8 |
0.86 |
0.0738 |
4.4 |
0.0023 |
|
Hepatic disease |
21.1 |
0.91 |
0.0101 |
23.5 |
1.05 |
0.0841 |
26.6 |
1.24 |
<0.0001 |
22.6 |
<0.0001 |
|
Rheumatoid arthritis |
7.6 |
1.16 |
0.0053 |
7.8 |
1.19 |
0.0001 |
7.7 |
1.18 |
0.0060 |
6.6 |
0.9359 |
|
Osteoporosis |
38.9 |
1.41 |
<0.0001 |
39.5 |
1.45 |
<0.0001 |
34.9 |
1.18 |
<0.0001 |
31.1 |
<0.0001 |
|
Asthma |
32.0 |
1.33 |
<0.0001 |
31.4 |
1.30 |
<0.0001 |
29.2 |
1.17 |
<0.0001 |
26.1 |
0.0124 |
|
Cerebral infarction |
79.8 |
20.71 |
<0.0001 |
17.9 |
1.14 |
<0.0001 |
12.0 |
0.71 |
<0.0001 |
16.1 |
<0.0001 |
|
Angina pectoris |
18.5 |
1.24 |
<0.0001 |
19.5 |
1.33 |
<0.0001 |
18.3 |
1.23 |
<0.0001 |
15.4 |
0.1967 |
|
Myocardial infarction |
3.0 |
1.40 |
<0.0001 |
2.5 |
1.15 |
0.0699 |
1.3 |
0.57 |
<0.0001 |
2.2 |
<0.0001 |
|
Pneumonia |
23.6 |
1.34 |
<0.0001 |
19.9 |
1.07 |
0.0210 |
15.5 |
0.79 |
<0.0001 |
18.8 |
<0.0001 |
The prevalence of hypertension, anemia, renal disease, hepatic disease, rheumatoid arthritis, osteoporosis, asthma, cerebral infarction, angina pectoris, myocardial infarction, and pneumonia was significantly higher in the complete denture group than in the control group (P<0.05). Cerebral infarction had the highest prevalence in the complete denture group (P<0.05), with an OR of 20.71 relative to the control group. The prevalence of diabetes did not differ significantly between the complete denture and control groups.
The prevalence of hypertension, diabetes, anemia, renal disease, rheumatoid arthritis, osteoporosis, asthma, cerebral infarction, angina pectoris, and pneumonia was significantly higher in the removable partial denture group than in the control group (P<0.05). However, the prevalence of hepatic disease and myocardial infarction did not differ significantly between these 2 groups.
The prevalence of diabetes, hepatic disease, rheumatoid arthritis, osteoporosis, asthma, and angina pectoris was significantly higher in the dental implant group than in the control group (P<0.05), while that of cerebral infarction, myocardial infarction, and pneumonia was significantly lower (P<0.05). The prevalence of hypertension, anemia, and renal disease did not differ significantly between the dental implant and control groups.
The prevalence of the abovementioned diseases, other than rheumatoid arthritis and angina pectoris, differed significantly among the 3 exposed groups (P<0.05).
Table 3 presents the prevalence, ORs, and significance levels of oral diseases in the exposed and control groups. The prevalence of periodontal disease was significantly higher in the complete denture, removable partial denture, and dental implant groups than in the control group (
P<0.05). Among the 3 exposed groups, the dental implant group showed the highest prevalence of periodontal disease (
P<0.05), with an OR of 23.46 relative to the control group. The prevalence of dental caries was significantly higher in the removable partial denture and dental implant groups than in the control group (
P<0.05), while it was significantly lower in the complete denture group than in the control group (
P<0.05). Among the 3 exposed groups, the dental implant group showed the highest prevalence of dental caries (
P<0.05).
Table 3
Prevalence of oral diseases in the exposed and control groups

|
Oral disease |
Complete denture |
Partial denture |
Dental implant |
Control group (%) |
P
|
|
% |
OR |
P
|
% |
OR |
P
|
% |
OR |
P
|
|
Periodontal disease |
69.7 |
1.67 |
<0.0001 |
89.4 |
6.10 |
<0.0001 |
97.0 |
23.46 |
<0.0001 |
58.0 |
<0.0001 |
|
Dental caries |
16.0 |
0.66 |
<0.0001 |
39.1 |
2.24 |
<0.0001 |
47.4 |
3.15 |
<0.0001 |
22.2 |
<0.0001 |
DISCUSSION
The present study evaluated the sociodemographic effects of Korean dental health insurance policies, which were developed to reduce the socioeconomic burden of oral reconstruction procedures. The cost for oral reconstruction procedures is especially burdensome for patients with systemic diseases that are costly to treat throughout their lifetime. According to the Health Data 2016 published by the Organization for Economic Co-operation and Development (OECD), public expenditures covered an average of 73.6% of the national healthcare expenditures across OECD countries in 2014 [
5], while in South Korea the proportion was only 58.8% [
6]. In addition, the out-of-pocket spending ratio for health care in South Korea is high for low-income patients with chronic diseases [
7], and the economic burden associated with severe diseases has increased [
89]. This indicates that efforts are needed to increase the available public finances and strengthen the coverage of health insurance in South Korea.
Many previous authors have pointed out that the high cost of dental treatment is the most common reason for delaying or not receiving dental care [
1011]. Although oral reconstruction is a prerequisite for enhancing the quality of life and general health of the elderly, its application is sometimes restricted by the dental health insurance coverage, income, financial status, and oral health status of those older than 65 years [
1213].
Efforts have been made to reduce the expenses of dental care for Korean patients. Health insurance coverage for complete dentures was implemented for patients older than 75 years in July 2012, after which the age limit for covered subjects has been reduced and the proportion of the costs covered by health insurance has been increased. In other countries that started to apply insurance benefits for dental prostheses earlier than Korea, such as Japan and Sweden, the national health insurance programs have guaranteed full coverage benefits for dentures [
4]. Insurance coverage for dental implants is currently only available in Sweden and Korea. However, the insurance benefits only cover up to 2 implants in Korea, while in Sweden there is no limit to the number of implants.
Many studies have investigated the necessity of health insurance coverage of prostheses for treating teeth loss, which has been prompted by the increasing elderly population in South Korea [
14151617]. These studies have mainly focused on the prosthodontic condition of the elderly and their requirements for prostheses. After the implementation of the new health insurance policy in Korea, the focus turned to questionnaires about perceptions of insurance coverage of dentures and implants within the elderly population [
181920]. However, there is a lack of research into the effectiveness of policy implementation utilizing objective data sources.
The present study analyzed patients who received insurance benefits categorized by sex, age, income quintile, and type of insurance coverage. This analysis revealed that the insurance benefits for dentures were paid more frequently to female patients than to male patients, and in terms of different age groups, most frequently to patients aged 75–80 years. Among patients aged 70–75 years, insurance coverage was applied more often for dental implants than for complete dentures, meaning that they had a higher number of missing teeth. These results are consistent with previous reports, which have found higher frequencies of periodontal disease and tooth loss among women than among men and in older subjects [
2122].
This study also found that the dependents of the workplace subscribers or the dependents of the local subscribers received insurance benefits for complete dentures or removable partial dentures more frequently than for dental implants. The subjects in these groups were very likely to have lost economic productivity, but they required oral reconstruction procedure due to the loss of multiple teeth. In such cases, dentures may be more closely aligned with the goals of Korean dental health policy than dental implants, which have a limitation that the insurance benefit for dental implants covers only up to 2 implants during the lifetime.
The analysis of income by quintile in this study revealed that the number of patients receiving benefits increased with the income quintile, but the differences were not statistically significant across all comparisons of the income quintiles. However, a comparison of the lowest and highest income quintiles revealed that the benefits received for complete dentures, removable partial dentures, and implants were 2.9-, 3.1-, and 4.1-fold higher, respectively, for those in the fifth quintile than those in the first quintile. This contrasts with reports that low-income patients require more support from the government due to their higher rate of tooth loss. This implies that the current policies for insurance coverage are more likely to benefit the middle-income elderly than those living in poverty. It has been reported previously that higher-income patients receive more benefits [
4], and this issue requires greater attention in order to improve the current system so that it provides better support to those in lower income brackets.
The prevalence of hypertension, anemia, renal disease, rheumatoid arthritis, osteoporosis, asthma, cerebral infarction, and angina was higher in the exposed group than in the control group. In particular, the prevalence of cerebral infarction was about 20 times higher in the complete denture group than in the control group, and it was found that patients with cerebral infarction were more likely to also be edentulous, need a complete denture, and receive more benefits. The relationships among cerebral infarction, oral health, and periodontal disease have been studied extensively through case studies and case-control studies, with results suggesting that tooth loss due to periodontal disease is very closely related to cerebral infarction [
232425]. Additionally, a study conducted in Korea reported a positive correlation between tooth loss and the risks of hypertension and cerebral infarction [
26]. Although those authors were unable to demonstrate a temporal relationship, they suggested that intracardiac thrombosis and periodontal disease share a common pathogenesis. In addition, the patients with cerebral infarction often have paralysis of the unilateral upper and lower limbs, making it difficult for them to perform oral hygiene activities, such as tooth brushing or interdental flossing. Poor oral hygiene is a risk factor for periodontal disease, which leads to the loss of teeth.
In contrast, the prevalence of hypertension, renal disease, cerebral infarction, and myocardial infarction was lower in the dental implant group than in the complete denture group. This means that patients with the above-listed diseases may prefer to receive noninvasive interventions such as complete or removable partial dentures rather than an invasive intervention such as dental implantation for oral rehabilitation, since these patients often take antiplatelet agents [
27], which can increase the risk of bleeding [
28], and the installation of dental implants can produce bacteremia [
29]. These factors can result in such patients and their dentists preferring treatment options with a low risk of bleeding.
The prevalence of periodontal diseases and dental caries was higher in the exposed group than in the control group in this study. Periodontal disease was more prevalent than dental caries in all 3 exposed groups. This is consistent with previous studies finding that tooth loss in the elderly is related more closely to periodontal disease than to dental caries, and there are many patients who choose tooth replacement over implant treatment for periodontal disease [
2130]. Because periodontitis is a chronic disease and can occur in multiple teeth, elderly patients with periodontal disease are likely to suffer from multiple tooth loss. This means that the limitation of insurance coverage in Korea for dental implants should be modified, and it is also necessary to expand insurance coverage to include continuing management, treatment, and education after completing the production of a prosthesis.
The use of sample cohort data in this study made it possible to confirm temporal changes in the exposed group. However, it is difficult to confirm the actual tooth loss rate and the underlying causal relationship only by comparing the prevalence of systemic and oral diseases. Follow-up studies are needed on lifestyle-related diseases such as hypertension, diabetes, anemia, renal disease, rheumatoid arthritis, osteoporosis, asthma, cerebral infarction, angina pectoris, and myocardial infarction, and on pneumonia, periodontal disease, the tooth loss rate, and prosthodontic requirements.
Despite the limitations associated with using sample cohort data, the present study is the first to confirm the effectiveness of expanding the health insurance policy to cover dental prostheses based on an analysis of representative and reliable NHIS data. In addition, this study is significant in being the only Korean study to confirm the correlation between systemic diseases and oral diseases by comparing patients who received actual insurance benefits and those who did not. In the future it will be necessary to expand universal healthcare protection through continuous downsizing of dental care and the reduction of nondental items.
In conclusion, the impacts of the Korean dental health insurance policy was different according to age and income quintile. There is a tendency to avoid dental implantation when certain systemic diseases are present, but it is likely that patients with systemic disease actually have a higher need for prosthetic treatments than do healthy individuals. The prevalence of periodontal disease and dental caries was higher in subjects who received dental insurance benefits than in healthy subjects. In addition, dentures may be more helpful from a socioeconomic perspective than dental implant treatments. The Korean dental health insurance policy appears to have been beneficial to the elderly, especially people suffering from an economic burden due to systemic diseases.
ACKNOWLEDGEMENTS
This study used a national sample cohort data of the National Health Insurance Service (NHIS-2017-1-109).
References
1. Kim NS, Park EJ, Jun J, Seo JH, Jeong Y, Lee YJ, et al. 5-1. Diagnosis and tasks. Health status and integrated care for elderly people: focused on healthcare. Research No. 17-37-01. Sejong: Korea Institute for Health and Social Affairs;2017. p. 437–454.
2. Sunwoo D, Lee SY, Kim DJ, Kim CW, Yoon JL, Nam HJ. 6. Policy suggestions and conclusion. Current situations of health care service system for older persons and its policy issues. Research No. 2014-22-9-1. Sejong: Korea Institute for Health and Social Affairs;2014. p. 173–178.
3. Health Insurance Review & Assessment Service. Healthcare bigdata hub [Internet]. Wonju: Health Insurance Review & Assessment Service;2016. cited 2017 Aug 13. Available from:
https://opendata.hira.or.kr.
4. Yun HK, Lee JH, Lee SH. Partial denture prosthesis implant and necessity thereof in Korean elderly: analysis of the data from the 5th National Health Nutrition Survey (2010–2012). J Digit Converg. 2014; 12:467–479.

7. Ruger JP, Kim HJ. Out-of-pocket healthcare spending by the poor and chronically ill in the Republic of Korea. Am J Public Health. 2007; 97:804–811.

8. Lee KS, Chang HS, Lee SM, Park EC. Economic burden of cancer in Korea during 2000–2010. Cancer Res Treat. 2015; 47:387–398.

9. Kim J, Lee E, Lee T, Sohn A. Economic burden of acute coronary syndrome in South Korea: a national survey. BMC Cardiovasc Disord. 2013; 13:55.

10. Listl S. Cost-related dental non-attendance in older adulthood: evidence from eleven European countries and Israel. Gerodontology. 2016; 33:253–259.

11. Rapalo DM, Davis JL, Burtner P, Bouldin ED. Cost as a barrier to dental care among people with disabilities: a report from the Florida behavioral risk factor surveillance system. Spec Care Dentist. 2010; 30:133–139.

12. Davidson T, Rohlin M, Hultin M, Jemt T, Nilner K, Sunnegårdh-Grönberg K, et al. Reimbursement systems influence prosthodontic treatment of adult patients. Acta Odontol Scand. 2015; 73:414–420.

13. Manski RJ, Hyde JS, Chen H, Moeller JF. Differences among older adults in the types of dental services used in the United States. Inquiry. 2016; 53:0046958016652523.

14. Kim YJ, Shin SC. The financing estimation and denture medical charge study for the Korean elderly's denture service under the National Health Insurance coverage. J Korean Acad Dent Health. 1997; 21:3–4.
15. Shin SC, Kim YJ, Kim JB. Study on an actuarial budget of insurance payment for denture service of Korean geriatric patients. J Korean Acad Dent Health. 1998; 22:333–346.
16. Kwon HG, Kim YN, Jeong GH, Song GB, Park DY. The financing estimation study for the Korean elderly's denture service under the National Health Insurance coverage. J Korean Acad Dent Health. 2003; 27:347–356.
17. Jung SH, Park KW, Kim CS. The financing estimation study about the National Health Insurance coverage for Korean elderly's removable denture service. J Korean Acad Dent Insur. 2010; 1:1–7.
18. Ryu HG. Knowledge of the dental health insurance standard in the dental hygienists: based on the elderly denture. J Korean Soc Dent Hyg. 2016; 16:61–67.

19. Kim HJ, Lee SM, Ahn SY, Kim CH. Knowledge, attitude, and recognition of health insurance coverage in tooth implant. J Korean Soc Dent Hyg. 2016; 16:195–204.

20. Lee YH, Chun JH, Lee JH. Oral health-related quality of life improvements and satisfaction in South Korea: results from the National Health Insurance Coverage Denture Project for the Elderly. J Korean Acad Oral Health. 2015; 39:37–42.

21. Nilsson H, Berglund JS, Renvert S. Periodontitis, tooth loss and cognitive functions among older adults. Clin Oral Investig. 2018; 22:2103–2109.

22. Russell SL, Gordon S, Lukacs JR, Kaste LM. Sex/Gender differences in tooth loss and edentulism: historical perspectives, biological factors, and sociologic reasons. Dent Clin North Am. 2013; 57:317–337.
23. Joshipura KJ, Hung HC, Rimm EB, Willett WC, Ascherio A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke. 2003; 34:47–52.

24. Minn YK, Suk SH, Park H, Cheong JS, Yang H, Lee S, et al. Tooth loss is associated with brain white matter change and silent infarction among adults without dementia and stroke. J Korean Med Sci. 2013; 28:929–933.

25. Taguchi A, Miki M, Muto A, Kubokawa K, Migita K, Higashi Y, et al. Association between oral health and the risk of lacunar infarction in Japanese adults. Gerontology. 2013; 59:499–506.

26. Choe H, Kim YH, Park JW, Kim SY, Lee SY, Jee SH. Tooth loss, hypertension and risk for stroke in a Korean population. Atherosclerosis. 2009; 203:550–556.

27. Simmons BB, Yeo A, Fung K. American Heart Association. American Stroke Association. Current guidelines on antiplatelet agents for secondary prevention of noncardiogenic stroke: an evidence-based review. Postgrad Med. 2010; 122:49–53.

28. Nathan AS, Sen S, Yeh RW. The risk of bleeding with the use of antiplatelet agents for the treatment of cardiovascular disease. Expert Opin Drug Saf. 2017; 16:561–572.

29. Bölükbaşı N, Özdemir T, Öksüz L, Gürler N. Bacteremia following dental implant surgery: preliminary results. Med Oral Patol Oral Cir Bucal. 2012; 17:e69–e75.
30. Nibali L, Farias BC, Vajgel A, Tu YK, Donos N. Tooth loss in aggressive periodontitis: a systematic review. J Dent Res. 2013; 92:868–875.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download