INTRODUCTION
The structures beneath the maxillary sinus consist of the alveolar ridge and the maxillary posterior teeth [
1]. Lack of sufficient alveolar bone height has long been a common deterrent to implant placement in the posterior maxilla. The lack of height may be the result of alveolar bone loss following tooth loss, periodontal disease, pneumatization of the maxillary sinus, or a combination of the above [
12]. Grafting the floor of the maxillary sinus is a means of correcting this deficiency.
Currently, 2 main augmentation procedures are used: the transcrestal and lateral window approaches [
2345]. Indications for the transcrestal approach include a moderately resorbed ridge, a relatively flat sinus floor, and a single implant. In contrast, the lateral window approach is commonly reserved for severely resorbed ridges and multiple implants [
6].
Stability of the graft material in the sinus and changes in the height of the graft material over time have been important issues. Wanschitz et al. [
7] found a resorption rate of graft material of 10%–13.9% after bone grafting in the sinus. It was reported that progressive sinus pneumatization occurred after augmentation with a 2:1 autogenous bone/xenograft mixture, and the long-term stability of sinus graft height represents an important factor for implant success [
8].
Anteriorly, the sinus generally extends to the canine and premolar region. Sharper angles and less width have often been observed in the premolar region, and septa have been more commonly found in the premolar region than in the molar region [
9]. The Schneiderian membrane, which lines the maxillary sinus, is adherent to the underlying bone and is at risk of being perforated during sinus augmentation procedures [
210]. If it is too small or too large, the mediolateral dimension of the maxillary sinus can present difficulties for sinus lifting procedures and can have negative effects on maintenance of the graft material in the maxillary sinus [
11]. Therefore, it can be assumed that the position of implant installation might affect the difficulty of the sinus lift procedure, thereby influencing the stability of the graft materials [
12].
Few studies have evaluated the maintenance of sinus graft height according to the surgical method and tooth type. The aims of the present study were to assess the amount of graft height change after sinus lift procedures and to analyze the factors influencing graft height changes, including the residual bone height before surgery, surgical approach, and tooth type.
MATERIALS AND METHODS
Patient selection
All the study participants provided informed consent, and this retrospective study was approved by the Institutional Review Board committee at Wonkwang University Daejeon Dental Hospital in 2016 (W1611/001-001). The study population comprised patients who had been treated with first-stage implant surgery with a simultaneous sinus elevation procedure on the maxillary posterior area of the edentulous region at the Department of Periodontology between 2009 and 2012.
The selected patients were examined to determine whether there were any signs or symptoms of oral disease before conducting sinus elevation. Patients who had absolute contraindications for implant surgery, such as uncontrolled diabetes, cardiovascular disease, and hematologic disorder were excluded.
The current study only included patients who had panoramic radiographs taken immediately after implant installation and at 3 months, 6 months, 1 year, 2 years, and 3 years after implant installation. Therefore, only 39 implants in 27 patients met the inclusion criteria. The patients ranged in age from 41 to 67 years (average, 54.5 years). All patients were non-smokers.
Surgical procedure
The sinus lift procedure was performed at the same time as implant placement. One periodontal surgeon performed all surgical procedures. The sinus was filled with deproteinized bovine bone mineral (OCS-B®, Nibec, Seoul, Korea).
The transcrestal approach (20 implants) was performed using the bone-added osteotome sinus floor elevation technique, which adds bone graft material to the site of the osteotome procedure, as described by Summers [
5]. The lateral window approach (19 implants) was performed as described by Kent and Block [
13]. In brief, the posterior part of the maxilla was exposed via a crestal incision and elevation of a mucoperiosteal flap. Implant sites were marked using surgical stain, and osteotomy was performed at the lateral aspect of the sinus wall. The sinus mucosa was carefully lifted and the bone graft materials were grafted into the sinus. The mucoperiosteal flap was repositioned and sutured.
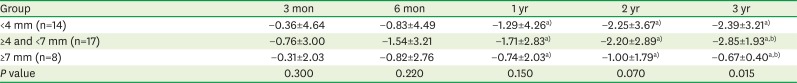
Radiographic measurements of graft height changes
We measured the implant length, residual bone height, and the distance between the implant platform and the base of the grafted sinus floor at 3 sides (the mesial, middle, and distal sides of the implant platform) to evaluate changes in graft height using INFINITT
® (Infinitt Healthcare, Seoul, Korea) software to the nearest 1/100 mm. These distances were abbreviated as MeGH, MiGH, and DiGH, respectively (
Figure 1). All measurements were made by 1 examiner, and the intra-examiner agreement was calculated to be 0.92 by the kappa test.
Figure 1
Radiographic measurements of graft height change using a panoramic radiograph. Lower dotted line and upper dotted line mean implant platform and grafted sinus floor, respectively.
a: The distance from the implant platform to the base of grafted sinus floor at the mesial side of the implant, b: The distance from the implant platform to the base of the grafted sinus floor at the middle side of the implant, c: The distance from the implant platform to the base of the grafted sinus floor at the distal side of the implant.
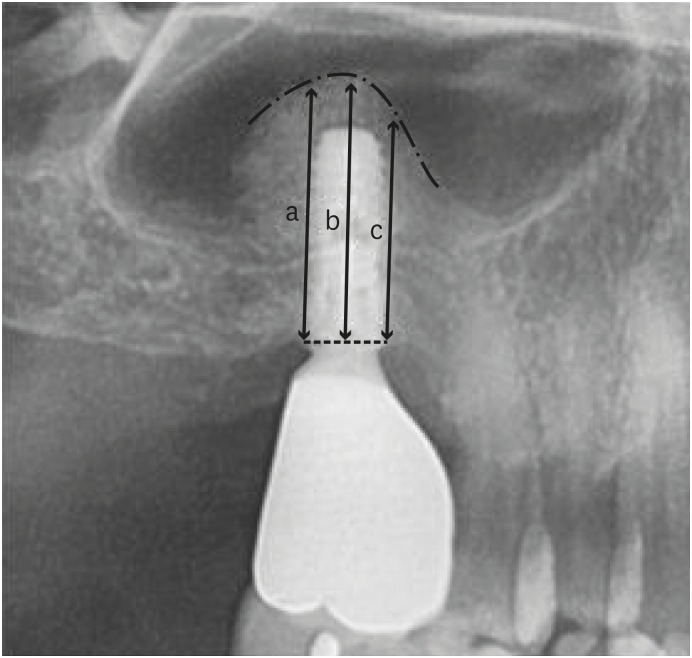
To correct for distortion of the obtained panoramic radiographs, we measured the distance from the implant platform to the apex (implant length) on each image and revised the values using the actual length of the implant. The mean values of the graft height at the mesial, middle, and distal sides of the implants were calculated and compared according to several factors, including the residual bone height before surgery, surgical approach, and tooth type. The current study did not consider other variables, such as the type of prosthesis, implant surface modifications, and the diameter and length of the implants.
Statistical analysis
One-way analysis of variance (ANOVA) was used to assess the decrease in graft height over time compared to baseline in each group. Differences in graft height changes between the groups according to the influencing variables at each observation point (or period) were evaluated using ANOVA for repeated measures. The Bonferroni test for post hoc analysis was utilized. Statistically significant differences were considered to be present at P<0.05. All statistical measurements were performed using SPSS version 17 (SPSS Inc., Chicago, IL, USA).
DISCUSSION
It is difficult to gain a sufficiently large amount of bone for implant placement when alveolar bone loss occurs after the extraction of maxillary posterior teeth and severe pneumatization. In situations where the alveolar bone has poor quality and short height, a sinus lift procedure should be the first option for treatment [
14]. Although researchers have tried to compare different alloplastic and allograft materials, debate continues as to the best graft material and the proper criteria for ideal indications. Recently, it has been suggested that deproteinized bovine bone and tricalcium phosphate appear to be as effective as autogenous bone for augmentation of the maxillary sinus [
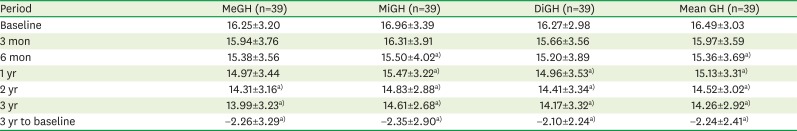
1516]. From a biological viewpoint, slow resorption and degradation of a biomaterial is attractive. We used deproteinized bovine bone mineral for sinus lift procedures on the basis of those recent studies and then analyzed graft height changes during 3 years after surgery. The mean graft height change was −2.24±2.41 mm at 3 years after surgery, and these changes became significant compared to baseline at 2 years after surgery.
Pneumatization may be caused by positive intrasinus air pressure due to respiration [
17], and this pressure might promote resorption and pneumatization after sinus augmentation [
18]. Pressure-induced degradation and resorption in the grafted sinus floor may lead to loss of vertical bone height. Listrom and Symington [
19] reported that there were no changes in length and width from 3 months to 10 years after sinus floor grafting, but there was a significant decrease in height of approximately 10%–15% between 3 months and 2 years and 3 months and 10 years. In the present study, there was a significant decrease in height of approximately 13.52% during 3 years after surgery. Hatano et al. [
8] reported that the overall height of the bone graft decreased during the first 2–3 years after augmentation and that only minor changes occurred thereafter, but the graft height remained higher than that observed before sinus augmentation for up to 96 months after augmentation. A long-term study investigating graft height changes after sinus augmentation seems to be necessary.
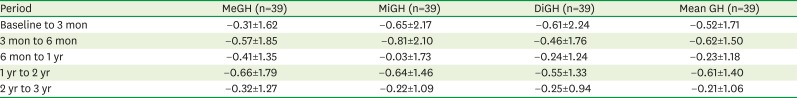
Although this trend was not statistically significant, a greater mean change was observed in the period before 6 months than between 6 and 12 months after surgery. We delivered the implant prosthesis at least 6 months after the simultaneous sinus augmentation and implant insertion procedure. We thus interpret these findings as supporting the proposal that implant loading may exert a stabilizing effect on the maintenance of bone graft height, consistent with the findings of Listrom and Symington [
19].
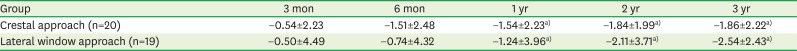
It was reported that the amount of native bone did not have a significant effect on the change in mean graft height over 3 years, although the least amount of graft height loss was found in patients with the greatest amount of preoperative residual bone height [
20]. In our study, there was a significant difference between the patients with residual bone height of ≥4 but <7 mm and the patients with residual bone height of ≥7 mm in terms of the graft height change after 3 years, but there was no proportional relationship of graft height change according to residual bone height. The least amount of height change at 3 years after augmentation was 0.67 mm in the patients with residual bone height of ≥7 mm. The stability of the graft height in those patients might have resulted from the technical simplicity of augmentation and the use of a relatively small amount of graft material.
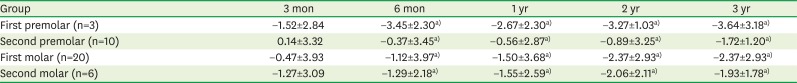
Cho and Kim [
21] reported that sinus graft height decreased significantly in the first 12 months after both the lateral window approach and crestal approach, consistent with our findings. Moreover, patients in whom the grafted sinus floor was above the implant apex showed a decrease over time, and this tendency was stronger in patients who underwent a procedure using the crestal approach than in those in whom the lateral window approach was used. However, there was no significant difference between the 2 surgical approaches in our study.
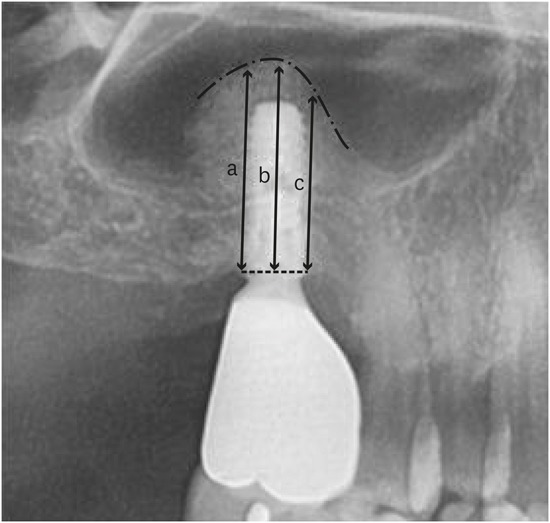
We analyzed graft height changes according to tooth type. We found that the first premolar sites showed the greatest changes of graft height, but the difference was not statistically significant. Sharper angles and less width have often been observed at premolar sites, so we assumed that the challenging sinus anatomy around the first premolar might have had a negative effect on the sinus lift procedures [
1112]. The limitations of this study in this regard include the considerably smaller sample size of the first premolar group (n=3). Obtaining fewer samples for the first premolar group was inevitable because molars are more commonly lost due to periodontitis and caries than premolars [
22]. In addition, the preoperative residual bone height at the first premolar site is usually adequate to insert an implant fixture without the need for a sinus lift procedure.
It was difficult to assess the position of the maxillary sinus floor accurately on 2-dimensional panoramic radiographs due to poor visualization [
23]. Therefore, we could not directly measure the length of the augmented sinus membrane, but instead indirectly measured graft height changes. To correct for the distortion of obtained panoramic radiographs, we revised the values using the actual length of the implants. This was done because we only included patients who had received first-stage implant surgery with a simultaneous sinus elevation procedure in this study. Computed tomography (CT) scans can be used to calculate the volume, not just the height, of graft materials in the sinus; however, multiple CT scans are not always justifiable and patient cooperation may be limited.
In conclusion, graft height after sinus lift procedures decreased over time, and the decrease was statistically significant starting at 2 years. There was no statistically significant difference in graft height change according to the surgical approach or tooth type. For residual bone height, significantly greater height change was detected in patients with residual bone height of ≥4 and <7 mm than in those with residual bone height of ≥7 mm (P<0.05).
Further studies are underway to determine whether the above trends are also found for other graft materials and other barrier membranes. Since the present study was conducted retrospectively without consideration of the type of graft material, implant surface modifications, diameter and length of the implants, or sinus anatomy, further studies with controlled variables should be done. More precisely designed prospective studies with 3-dimensional images will be also needed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download