Abstract
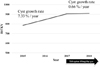
A 22-year-old male patient was diagnosed with autosomal dominant polycystic kidney disease (ADPKD). He received conservative treatment with an angiotensin-converting enzyme inhibitor. Two years later, oral therapy, consisting of 60 mg tolvaptan per day, was initiated. Compared with height-adjusted total kidney volume, the rate of kidney growth reduced significantly from 7.33% to 0.66% annually, since commencement of the tolvaptan therapy. The liver enzyme profile and serum sodium level and osmolality were constantly within normal ranges. In Korea, this is the first reported case of a patient with ADPKD who received tolvaptan treatment for more than 1 year. This case demonstrates that long-term tolvaptan treatment appears to be safe, well tolerated, and effective for ADPKD.
Autosomal dominant polycystic kidney disease (ADPKD) is a common genetic disorder, but there are no effective treatments till date. Tolvaptan, a V2 receptor antagonist, is known to be beneficial in the inhibition of cystic growth in patients with ADPKD. Tolvaptan was approved as a treatment modality for ADPKD in Korea; however, its long-term use in clinical practice is rare because of its high cost. Herein, we describe a case of a 22-year-old male ADPKD patient who was treated with tolvaptan for 1 year.
A 22-year-old male patient visited the renal department of Chonnam National University Hospital for evaluation of an abnormal computed tomography (CT) finding. His height was 179 cm, body weight was 58 kg, and body mass index was 18 kg/m2. There was no history of any underlying disease and, at the time, he was not taking any medication. His family history was non-specific. Initial laboratory findings were all within normal range. Laboratory investigations showed leukocyte count, 9,500 cells/mL; hemoglobin, 13.0 g/dL; platelet count, 340,000 cells/mL; blood urea nitrogen level, 16.1 mg/dL; creatinine, 0.75 mg/dL; estimated glomerular filtration rate, 130.2 mL/min/1.73 m2 (which was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula: mL/min/1.73 m2=141 × minimum(creatinine/k, 1)α × maximum (creatinine/k, 1)−1.209 × 0.993age × 1.018 (if female) × 1.159 (if black), where κ is 0.7 for women and 0.9 for men, and α is −0.329 for women and −0.411 for men1); sodium level, 138 mEq/L; potassium level, 4.0 mEq/L; chloride level, 114 mEq/L; magnesium level, 2.0 mg/dL; total calcium level, 8.4 mg/dL; and serum osmolality, 290 mOsmol/kg. Urine analysis showed the following values: urine osmolality, 312 mOsmol/kg; random urine sodium, 120 mEq/L; random urine potassium, 30.4 mEq/L; random urine chloride, 61 mEq/L; and urinary pH, 7.0. Urine analysis did not show any proteinuria, hematuria, or glucosuria. Contrast-enhanced CT of the abdomen (Fig. 1A) was performed. Over 20 cysts were detected in both kidneys and in the liver. The right kidney size was 171.30mm (length) × 120.29 mm(width) × 65.80 mm(depth), and the left kidney size was 163.42 mm(length) × 101.88 mm(width) × 79.86mm(depth).
Genetic analysis was performed using Sanger's method. Direct sequencing revealed that the 22nd intron had translocated from G to A, which was previously reported as a pathogenic variant, but the change in amino acid was unknown (Fig. 2)2).
An angiotensin-converting enzyme inhibitor treatment was started and a follow-up CT was performed after 2 years (Fig. 1B). The volume of each kidney was as follows: right kidney volume, 828 mL; left kidney volume, 791 mL; total kidney volume (TKV), 1,620 mL; and height-adjusted total kidney volume (HtTKV), 905 mL/m. The CT showed that the growth rate of the HtTKV was 7.33% per year.
From May 2017, tolvaptan therapy was initiated at a dose of 60 mg per day, with morning and afternoon doses at 45 mg and 15mg, respectively. Monthly checks of the body weight, blood pressure, and laboratory tests including complete blood count, renal function test, electrolyte text, liver function test, random urine electrolytes, and osmolality were performed. Further clinical course was uneventful and the electrolyte levels remained unremarkable. The patient did not report any specific side effects of the tolvaptan therapy, except polyuria and polydipsia. The liver enzyme profile and serum sodium level and osmolality remained within normal range. The serum creatinine was 0.97 mg/dL after 1 year of the tolvaptan therapy (Fig. 3). The urine osmolality decreased to less than 300 mOsmol/kg and urine sodium was less than 100 mOsmol/kg.
Another follow-up abdominal CT was performed 11 months after commencement of tolvaptan therapy (Fig. 1C). The size of each kidney was as follows: right kidney volume, 837 mL; left kidney volume, 792 mL; TKV, 1,629 mL; and HtTKV, 910 mL/m. The growth rate of HtTKV decreased from 7.33% to 0.66%(Fig. 4). Till the foreseeable future, the plan is to maintain the current tolvaptan therapy with its same dosage, unless a specific problem occurs.
ADPKD is a genetic disorder characterized by the growth of multiple, variable-sized cysts in the kidneys. ADPKD is often accompanied by abnormalities in two major intracellular messengers: calcium and 3′,5′-cyclic adenosine monophosphate (cAMP). Proteins polycystin 1 and polycystin 2 regulate intracellular calcium levels, and intracellular calcium plays a role in inhibiting cyclic AMP; increased cAMP plays a significant role in cyst growth345). In addition, adenylyl cyclase 6 regulates inner medullary cAMP formation and aquaporin-2 phosphorylation and expression. Vasopressin V2 receptor (V2R) mediates the activation of adenylyl cyclase 6 and cAMP-enhanced phosphorylation of aquaporin-26). Therefore, a V2 receptor antagonist inhibits the progression of ADPKD by reducing intracellular cAMP and adenylyl cyclase 6. The TEMPO clinical trial7) and the recent REPRISE clinical trial7) demonstrated higher impediment of cyst growth and preservation of the estimated glomerular filtration rate in the tolvaptan-treated group than in the control group. Because of the risk of liver-enzyme level elevation, this clinical trial suggested that a regular checkup of liver function is required.
In our case, tolvaptan was administered at 60mg per day for about 1 year. After taking tolvaptan for the first time, the patient complained of aquaresis-related symptoms such as polyuria (>5 L) and polydipsia but his weight remained constant. There were no specific side effects including elevation of liver-enzyme levels.
Abdominal CT was performed 3 times: at baseline, 2 years after conservative treatment, and 11 months after commencement of tolvaptan therapy. The TKV indicates the progression of renal insufficiency in patients with ADPKD; thus, qualifying it as a predictive biomarker is important910). The radiologist in Chonnam National University Hospital measured the kidney's width, depth, and length each time. The TKV was measured using the ellipsoid method and adjusted with the height10). When comparing the TKV before and after tolvaptan therapy, it is seen that the cyst growth rate decreased from 7.33% to 0.66%, and this suggests that the tolvaptan treatment was effective in slowing cyst growth.
Figures and Tables
Fig. 1
Abdominal computed tomography at January 2015, April 2017, and April 2018. A) Right kidney: length, 171.30 mm; width, 120.29 mm; depth, 65.80 mm. Left kidney: length, 163.42 mm; width, 101.88 mm; depth, 79.86 mm. B) Right kidney: length, 183.88 mm; width, 122.46 mm; depth, 70.25 mm. Left kidney: length, 170.62 mm; width, 102.77 mm; depth, 86.24 mm. C) Right kidney: length, 183.90 mm; width, 126.06 mm; depth, 68.77 mm. Left kidney: length, 164.02 mm; width, 106.24 mm; depth, 86.75 mm.

Fig. 2
Genetic analysis using Sanger's method. Direct sequencing revealed that the 22nd intron had translocated from G to A.

Acknowledgement
This research was assisted by two grants from Chonnam National University Hospital Biomedical Research Institute (CRI18015-1 & CRI16015-1).
References
1. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine. 2009; 150:604–612.

3. Gattone VH, 2nd , Wang X, Harris PC, Torres VE. Inhibition of renal cystic disease development and progression by a vasopressin V2 receptor antagonist. Nat Med. 2003; 9:1323–1326.

5. Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007; 369:1287–1301.

6. Rieg T, Tang T, Murray F, et al. Adenylate cyclase 6 determines cAMP formation and aquaporin-2 phosphorylation and trafficking in inner medulla. J Am Soc Nephrol. 2010; 21:2059–2068.

7. Torres VE, Chapman AB, Devuyst O, et al. Investigators: Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2012; 367:2407–2418.

8. Torres VE, Chapman AB, Devuyst O, et al. Investigators: Tolvaptan in Later-Stage Autosomal Dominant Polycystic Kidney Disease. N Engl J Med. 2017; 377:1930–1942.

9. Grantham JJ, Torres VE, Chapman AB, et al. Investigators: Volume progression in polycystic kidney disease. N Engl J Med. 2006; 354:2122–2130.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download