Abstract
Non-traumatic exertional rhabdomyolysis (exRML) occurs in individuals with normal muscles when the energy supplied to the muscle is insufficient. Here, we report 11 cases of spinning-induced rhabdomyolysis and review related literature. Spinning is a kind of indoor bicycle sport. The 11 patients who were diagnosed with exRML and admitted to CHA Bundang Medical Center were female and their ages ranged from 15 to 46 years. Two to three days prior to the presentation, the patients had attended a spinning class for the first time. All the patients had been otherwise healthy without any known medical illnesses. They were successfully treated without any complications, except mild non-symptomatic hypocalcemia. However, in the literature, severe complications such as compartment syndrome or acute kidney injury had been reported in relation to exRML including spinning-induced rhabdomyolysis. This spinning exercise needs prior guidelines and specific warnings to prevent exertional rhabdomyolysis.
Rhabdomyolysis is a clinical syndrome characterized by muscle necrosis and the release of intracellular muscle constituents into the circulation. It can be caused by burns, shock, acidosis, infections, crush trauma, immobility, malignancy, toxins, drugs, and muscle diseases1). Among the various types of rhabdomyolysis, non-traumatic exertional rhabdomyolysis (exRML) occurs in individuals with normal muscles and appears when the energy supplied to the muscle is insufficient23). ExRML related to military training, marathon running, weight training, and other forms of strenuous exercise have been reported4).
Spinning is a group indoor cycling exercise, which has become popular recently over the past few years. This stationary cycling program is composed of five core movements and riders may synchronize their pedaling to the rhythm of the music while they are exercising5).
We observed that recently there has been an increasing number of patients who were diagnosed with exRML at CHA Bundang Medical Center after attending a spinning class. Here, we introduced the clinical cases of spinning induced rhabdomyolysis and review the related literature.
We found 11 cases of exRML patients who were admitted to CHA Bundang Medical Center between July 1, 2014 and March 31, 2015. All of the patients were female and their mean age was 23.2±8.3 years. Their mean body mass index (BMI) was 23.9±2.6 kg/m2 (ranged from 19.6 to 28.0). Their common chief complaints were dark urine and thigh soreness. Two to three days prior to the presentation, the patients had attended a spinning class for the first time. Nine of the patients had brown-colored urine within two days and another two patients noticed that their urine had become darker three days after their first spinning class. None of the patients had any significant past medical history and were not on any medication.
All of the patients were afebrile with normal vital signs upon presentation. Their thighs were moderately firm and warm to the touch, with reduced range of movement and strength. Complete blood-count, urea, creatinine, and electrolyte values were within normal ranges at the initial blood analysis. However, their serum creatinine phosphokinase (CPK) level was over 11,000 U/L (normal range: 38-160). Additionally, other serum levels of muscle enzymes (creatine kinase-MB type, lactate dehydrogenase, alanine aminotransferase, aspartate aminotransferase, and myoglobin) were significantly elevated (Table 1). Serum BUN and creatinine levels stayed within the normal range and no acute kidney injury (AKI) had developed during treatment. Dipstick testing of the urine was positive (3+) for blood; however, subsequent microscopy revealed less than four red blood cells under high power field (HPF) microscopy. A bone scan study showed diffuse type of soft tissue uptakes in the damaged muscles including rectus femoris, sartorius, vastus medialis, vastus lateralis, and pectineus (Fig. 1).
A diagnosis of rhabdomyolysis was made and the patients were treated with a combination of bed rest and aggressive intravenous fluid (normal saline) to maintain a urine output of 200 to 300mL/hour. When the urine pH was less than 6.0, sodium bicarbonate (mixed with 5% dextrose water) was used for urine akalinization. Although eight of the patients had mild hypocalcemia, calcium supplementation was unnecessary because no hypocalcemic symptoms were observed (Table 1).
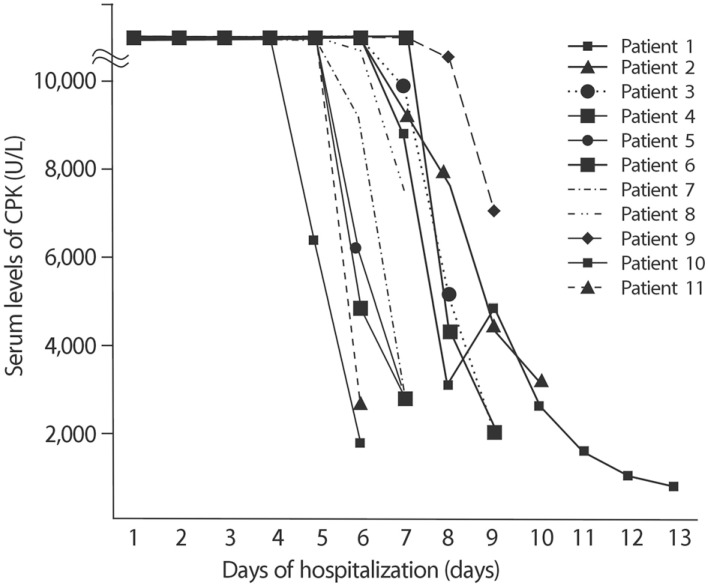
In a span of 6-12 days, the CPK level dropped to below 5,000 U/L (Fig. 2). Also, other serum muscle enzymes decreased. The mean hospital stay was 7.6±1.9 days (Table 1). One patient (number 1) was hospitalized for an additional 4 days after her CPK level was markedly reduced (4,820 U/L) on the 8th day along with her complaints of thigh myalgia. All the patients were discharged in good condition and with no complications.
ExRML has been defined by a combination of findings, including exercise-associated muscle pain, swelling, dark urine, and increased CPK level to at least five times the upper limit of normal, and myoglobinuria6). It should be noted that our patients had CPK levels of nearly 70 times the upper limit of normal (Table 1). Also, a urine dipstick that is positive for blood but shows few red blood cells is suggestive of myoglobinuria7).
In the pathogenesis of exercise-induced rhabdomyolysis, calcium(Ca2+) has been suggested as an important key factor3). During exercise, a decreased amount of adenosine triphosphate (ATP) could cause dysfunction of Na+-K+ ATPase and an increased level of Na+ in the cells, resulting in the reverse activation of Na+-Ca2+ exchanger mode3). Consequently, the increased intracellular calcium leads to the activation of proteases, skeletal muscle cell contraction, mitochondrial dysfunction, reactive oxygen species production, and eventual skeletal muscle cell death23).
Treatment of rhabdomyolysis involves stopping the continued breakdown of the muscle fibers and preventing the development of AKI. The rapid and aggressive infusion of intravenous crystalloid is used to obtain a urinary output of 200-300mL/hour. Myoglobin is toxic in acidic urine, and most experts advocate the use of intravenous sodium bicarbonate to maintain a urinary pH of 6.5 or greater67). Loop diuretics may be given to patients who develop volume overload complications such as pulmonary edema. Calcium supplementation should be given only for symptomatic hypocalcemia or severe hyperkalemia. The initiation of renal replacement therapy in clinical practice depends on the status of renal impairment, with complications such as life-threatening hyperkalemia, anuria, metabolic acidosis, or hyperhydration without response to diuretic therapy89). It is reported that both continuous venovenous hemofiltration with a high permeability membrane and high cutoff membrane hemodiafiltration are effective in removing serum myoglobin (17kDa)1011). Although successful treatment with plasmapheresis to remove serum myoglobin in statin-induced rhabdomyolysis have been reported, its use seems still controversial9).
Most of the related articles mentioned that the majority of spinning-induced rhabdomyolysis patients were discharged without any complication when they were treated early and aggressively with intravenous fluids7). However, in rare cases, some patients demonstrated severe complications, such as compartment syndrome and AKI4). AKI in rhabdomyolysis may occur due to renal vasoconstriction, formation of intratubular casts, and direct myoglobin toxicity caused by accumulation of myoglobin in the renal tubules19). Compartment syndrome may occur in the leg or forearm due to the edema caused by muscle injury and tissue damage4). Compartment pressures greater than 30-45mmHg typically necessitate surgical intervention. Cardiac dysrhythmias via electrolyte abnormalities and disseminated intravascular coagulopathy are other possible complications of exRML4).
Known risk factors of exRML are the exercise experience, intensities or types of exercises37). Other possible causes were hyperthermal environments, electrolyte imbalance, malnutrition, creatine supplements and alcohol drinking3). Influenza virus infection and genetic deficiency of metabolic factors can be risk factors as well3). It has been reported that men are vulnerable to exRML because estrogen plays a protective role1213). Interestingly, all 11 spinning-induced rhabdomyolysis cases in this article occurred in females. It is unclear whether they were malnourished by their diet plan or had little exercise experience and thus were at higher risk of spinning induced rhabdomyolysis.
There are specific guidelines to prevent exRML3). First, sufficient amount of time to warmup and cooldown should be considered. Second, standard education on exercise-induced rhabdomyolysis is also important. Coaches and athletes should understand the danger, symptoms, and signs of exRML. Third, exercise should be modified or abstained in the presence of evitable risk factors such as influenza. Lastly, sufficient hydration and nutrition support can be effective.
In our cases, all 11 patients were treated early and properly without any complication, except a mild non-symptomatic hypocalcemia. However, considering the possibility of severe complications of exRML as aforementioned, and the medical expenses of hospital stay, information and guidelines for preventing spinning-induced rhabdomyolysis have to be provided prior to starting the exercise.
References
1. Melli G, Chaudhry V, Cornblath DR. Rhabdomyolysis: an evaluation of 475 hospitalized patients. Medicine (Baltimore). 2005; 84:377–385. PMID: 16267412.
2. Giannoglou GD, Chatzizisis YS, Misirli G. The syndrome of rhabdomyolysis: Pathophysiology and diagnosis. Eur J Intern Med. 2007; 18:90–100. PMID: 17338959.

3. Kim J, Lee J, Kim S, Ryu HY, Cha KS, Sung DJ. Exerciseinduced rhabdomyolysis mechanisms and prevention: A literature review. J Sport Health Sci. 2015; 1–11.

4. DeFilippis EM, Kleiman DA, Derman PB, DiFelice GS, Eachempati SR. [Primary care] Spinning-induced rhabdomyolysis and the risk of compartment syndrome and acute kidney injury: Two cases and a Review of the Literature. Sports Health. 2014; 6:333–335. PMID: 24982706.
5. Walter C, Tannander AB. Complete idiot's guide to fitness. 1st ed. New York: Alpha Books;2000. p. 148–149.
7. Young IM, Thomson K. Spinning-induced rhabdomyolysis: a case report. Eur J Emerg Med. 2004; 11:358–359. PMID: 15542997.

9. Petejova N, Martinek A. Acute kidney injury due to rhabdomyolysis and renal replacement therapy: a critical review. Crit Care. 2014; 18:224. PMID: 25043142.

10. Heyne N, Guthoff M, Krieger J, Haap M, Häring HU. High cut-off renal replacement therapy for removal of myoglobin in severe rhabdomyolysis and acute kidney injury: a case series. Nephron Clin Pract. 2012; 121:c159–c164. PMID: 23327834.

11. Amyot SL, Leblanc M, Thibeault Y, Geadah D, Cardinal J. Myoglobin clearance and removal during continuous venovenous hemofiltration. Intensive Care Med. 1999; 25:1169–1172. PMID: 10551978.

12. Clarkson PM, Hubal MJ. Are women less susceptible to exercise-induced muscle damage. Curr Opin Clin Nutr Metab Care. 2001; 4:527–531. PMID: 11706288.

13. Tiidus PM, Deller M, Bombardier E, Gül M, Liu XL. Estrogen supplementation failed to attenuate biochemical indices of neutrophil infiltration or damage in rat skeletal muscles following ischemia. Biol Res. 2005; 38:213–223. PMID: 16238100.

Fig. 1
Bone scan image of a spinning-induced rhabdomyolysis patient. Diffuse type of soft tissue uptake was observed in both thigh muscles (Case No.11, age: 24, Female).
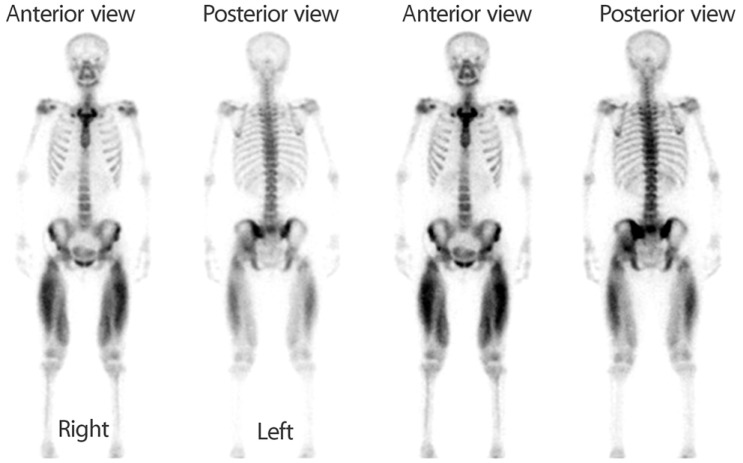
Table 1
Profile of patients and initial laboratory data
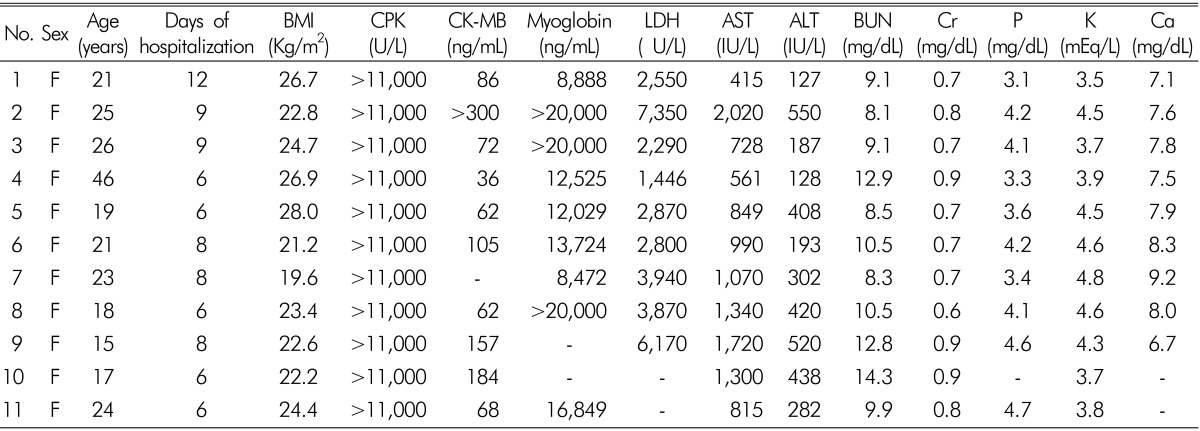
F: female, BMI: body mass index, CPK: serum creatine phosphokinase, CK-MB: serum creatine kinase -MB type, LDH: lactate dehydro- genase, AST: alanine aminotransferase, ALT: aspartate aminotransferase, BUN: serum blood urea nitrogen, Cr: serum creatinine, P: serum phosphorus, K: serum potassium, Ca: serum calcium




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download