INTRODUCTION
Solar lentigines are a typical form of epidermal pigmentation and represent early signs of photoaging. They increase in number and prevalence with age and tend to vary in size and color
1. In East Asians, solar lentigines are most common in middle and old age and are considered a major cosmetic problem. For that reason, many treatment options exist, including laser treatments
2. Solar lentigines, like other epidermal pigmentary problems, are associated with increased deposition of melanosomes, which are the main target structure of dermatological treatments. The thermal relaxation time (TRT) of melanosomes for selective damage is approximately 50~250 ns, so 532 nm Q-switched lasers operating in nanoseconds (5~100 ns) are the lasers of choice for the treatment of solar lentigines
3. Among various Q-switched lasers, 532 nm Q-switched neodymium:yttrium-aluminum-garnet (QSND) lasers are most commonly used for treating solar lentigines
4. However, post-inflammatory hyperpigmentation (PIH) after 532 nm QSND laser treatment is very common, reported to occur in 10 to 47 percent of cases
45. Recently, lasers with picosecond (PS) pulse duration have become more widely used in the aesthetic field. The first use of PS lasers was for tattoo removal, but the applications of PS lasers are extending to the treatment of various forms of pigmentation, scarring, and aged skin. PS lasers emit shorter pulses (300~900 picoseconds), which create a greater photomechanical effect and less unwanted heat diffusion into surrounding structures
6. Considering these characteristics of PS lasers, more effective results and reduced PIH are expected after their use
78. Nevertheless, to date, few objective studies have been performed to clarify the effectiveness of PS laser treatment of solar lentigines. To the best of our knowledge, this is the first split-faced comparison between 532 nm QSND laser and 532 nm PS laser treatment, allowing the clinical effects of both lasers on solar lentigines to be more accurately evaluated.
MATERIALS AND METHODS
This was a prospective, randomized, split-face, controlled trial study. The study protocol was approved by the Institutional Review Board of the Kangbuk Samsung Hospital (IRB no. KBSMC 2017-8-025-001).
Patients
We enrolled 20 females (27~72 years) with Fitzpatrick skin types III~V and more than 5 clinically obvious solar lentigines observed on both sides of the face for inclusion in this study. The faces of the enrollees were divided into halves (right and left sides with a line down the middle) with the halves randomly allocated for 532 nm PS laser or 532 nm QSND laser treatment in a 1:1 fashion using SAS (ver. 9.3; SAS Institute, Cary, NC, USA).
Treatment protocol
Each patient made a total of five visits for treatment and evaluation. All patients received one laser treatment and with results evaluated at 2, 4, 8, and 12 weeks after treatment. A 532 nm PS laser (Picocare; Wonteck Co., Ltd., Daejeon, Korea) with 450 picosecond pulse duration, 3~4 mm spot size, 0.3~0.5 J/cm2 fluence, and 2 Hz frequency was used for treating one side of the face, and a 532 nm QSND laser (Pastelle; Wonteck Co., Ltd., Daejeon, Korea) with 10 nanosecond pulse duration, 3~4 mm spot size, 0.6~0.8 J/cm2 fluence, and 2 Hz frequency was used for treating the other side. The endpoint of treatment was slight whitening immediately after laser irradiation.
Evaluation
Photographic images were obtained pretreatment, 2 weeks, 4 weeks, 8 weeks, and 12 weeks post-treatment. A digital camera and specialized imaging system (Dermavision 1; Optobiomed Inc., Gangwon, Korea) were used to record full face images to assist in the evaluation and assessment of skin pigmentation. We received the patient's consent form about publishing all photographic materials. The overall facial pigmentation of each patient before and after treatment was assessed by three dermatologists who were blinded to the treatment specifics and operated independently of this study. The quartile improvement scale (QIS) was used to assess clearance in the treated areas 12 weeks after treatment: no improvement (0%, score 0), poor (1%~25%, score 1), fair (26%~50%, score 2), good (51%~75%, score 3), or excellent (76%~100%, score 4). Subjective satisfaction was scored using a questionnaire with answers given on a 5-point scale (0=very unsatisfied, 5=very satisfied). Assessments of pain during laser treatment were conducted with an 11-point numeric pain scale (0=no pain, 10=intolerable pain). Additional details about the methods are available at
Supplementary Materials 1, and
Supplementary Table 1.
Safety assessments
All adverse effects after treatment and PIH were observed and recorded throughout the study, and the occurrence of PIH was evaluated at 12 weeks post-treatment.
Statistical analysis
All data were analyzed by the Mann–Whitney test and Fisher's exact test. All p-values were at a significance level of 0.05 (two-tailed) for all analyses, which were performed using SAS software.
RESULTS
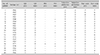
A total of 20 patients were enrolled and completed the study protocol (
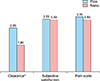
Table 1). The 5-point QIS assessed by three blinded dermatologists 12 weeks after treatment resulted in a mean QIS for the 532 nm PS laser group of 2.95 and a mean QIS for the 532 nm QSND laser group of 1.8 (
p<0.05). In subgroup analysis of 14 patients who did not develop PIH in both left and right faces, the mean QIS was 3.14 in the PS laser group and 2.21 in the QSND laser group (
p<0.05). Subjective satisfaction, which was scored on a 5-point scale 12 weeks after treatment, resulted in mean scores of 3.55 for the 532 nm PS laser group and 3.5 for the 532 nm QSND laser group. The 11-point numeric pain scale measured immediately after the treatment yielded a mean score of 3.7 for the 532 nm PS-laser group and 3.5 for the 532 nm QSND laser group. Mean values of QIS, subjective satisfaction, and pain scale are presented in
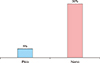
Fig. 1. PIH, which was assessed 4 weeks after treatment, developed 5% of cases in the 532 nm PS laser group and 30% in the 532 nm QSND laser group (
p=0.057) (
Fig. 2).
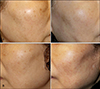
Fig. 3 and
Fig. 4 show representative photographs of patients evaluated in this study. We observed no clinically meaningful adverse effects during the treatment and follow-up period.
DISCUSSION
This prospective split-face study was designed to compare the efficacy and adverse effects of 532 nm PS laser and 532 nm QSND laser treatment of solar lentigines in Korean patients. Recently, some studies reported the clinical effectiveness (excellent clearance and less PIH) of 532 nm PS lasers for treating solar lentigines. However, there were no well-designed prospective comparisons between 532 nm PS laser and QSND laser treatment.
There are many treatment options available for solar lentigines, which can be categorized into non-laser and laser treatments. Examples of non-laser treatments include bleaching creams, cryotherapy, and chemical peels. These treatments suffer from unsatisfactory success rates, long treatment duration, and frequent skin irritation
910. Among laser treatment options, nanosecond Q-switched lasers with various wavelengths (532, 694, 755, 1,064 mn), some long pulsed lasers, and intense pulsed light are commonly used. Among these, 532 nm QSND lasers are typically used because they offer high absorption by melanin pigment
45.
The 532 nm QSND laser, when used in light-skinned patients, results in minimal complications. However, in darker-skinned individuals with melanin rich epidermis, the risk of PIH is greater (10%~25%). High risk of PIH after 532 nm QSND laser treatment is thought to be due to the combination of photothermal and photomechanical effects caused by short bursts of high energy nanosecond radiation, which not only targets melanin, but induces damage to surrounding oxyhemoglobin and melanin as well, resulting in inflammation of superficial vessels, altered activity of melanocytes, and subsequent PIH
11.
Because of the high incidence of PIH after treatment by QSND lasers, alternative lasers have been tried. Some previous studies showed that intense pulsed light or long pulsed alexandrite lasers led to better results and less PIH in the treatment of solar lentigines
1213. However, these studies were not objective and suffer from too many limitations to uncritically accept their results. The PS laser was first introduced as an effective treatment for tattoo removal, with a very short pulse duration that allows the selective destruction of small tattoo ink particles and a TRT of less than 1 nanosecond. Although the TRT of melanosomes is not less than 1 ns, strong photomechanical effects and heat confinement abilities of PS lasers have led some to expect better clinical results of PS laser treatment for pigmentation, leading to numerous clinical trials exploring PS laser use for treating pigmentation
14. Since 2004, studies have indicated promising efficacy of PS laser use for the treatment of pigmentary disorders including café-au-lait spots, dermal pigmentation, and dark circles
15. These studies showed that fewer treatment sessions and lower energy fluence may be required to achieve similar clinical outcomes to QSND laser treatment
15. Regarding solar lentigines treatment, Guss et al.
7 reported that the 532 nm PS laser showed more than 50% improvement of solar lentigines after only 1 session in 83% of patients. In similar study, Negishi et al.
8 reported that the 532 nm PS laser showed more than 75% clearance with only a single treatment in 93.02% of lesions. No severe or unexpected events occurred during both studies
78. PIH occurred 0.8%
7 and 4.65%
8 of lesions respectively. As evidenced in previous studies, PIH is rare in lentiginous lesions treated with 532 nm PS lasers, even in darker-skinned patients
78. Recently, a study of solar lentigines demonstrated destruction of melanosomes and damage to surrounding structures after 532 nm QSND laser treatment, but no obvious damage to other structures after 532 nm PS laser treatment. These results demonstrated precise, controlled damage confined to pigmented areas in the actual skin tissue. Therefore, we hypothesized that PS laser treatment would minimize inflammation and the incidence of PIH
8.
In this study, we found that both 532 nm QSND laser and 532 nm PS laser resulted in good treatment effects. Subjective satisfaction was similar for both treatments. However, the clearance rates for 532 nm QSND laser and 532 nm PS laser treatment were significantly different, corresponding to 2.95 and 1.8 at 12 week follow-up, respectively. This difference may be due to the fact that subjective satisfaction is generally higher than objective measurement, and because objective assessments were performed by dermatologists using photographs and a skin analyzer, allowing for more accurate evaluation. PIH occurred in 5% of cases treated by 532 nm PS laser, and 30% of cases treated by 532 nm QSND laser. Unfortunately, we were unable to obtain statistically significant results for the comparison of PIH incidence, probably because PIH incidence was too low. However, the PIH incidence observed in the present study is similar to those of previous studies, in which 0.8%~4.7% of patients experienced PIH after PS laser treatment
78. Regarding safety and patient compliance, pain was transient and mostly minimal in treatments with both lasers. There was no significant difference in median pain scores between lasers. Topical anesthetic application under occlusion for 30~45 minutes was usually sufficient for controlling pain during treatment. No significant adverse problems were reported during this study. Limitations of this study include (1) the small number of subjects, (2) clinical diagnosis of solar lentigines without skin biopsy, and (3) the possibility of unequal distribution of solar lentigines on both facial sides. Despite these limitations, this study is the first direct prospective split-face comparison of 532 nm PS and QSND laser treatments of facial solar lentigines in dark-skinned Korean patients. We found that the 532 nm PS laser is a promising treatment option for solar lentigines.
Based on the results of this study, we conclude that 532 nm PS laser treatment removes solar lentigines more effectively than 532 nm QSND laser treatment, a conclusion that was statistically clarified by objective assessment. However, the subjective satisfaction of patients was not significant different between the treatment groups, perhaps reflecting the fact that subjective satisfaction is generally higher than objective measurements of efficacy. PIH incidence was lower in cases treated with the 532 nm PS laser, but the difference was not statistically significant, possibly because the incidence of PIH was too low for demonstrating statistical significance.
In conclusion, both the 532 nm PS laser and QSND laser are safe and effective for the treatment of solar lentigines. However, considering differences in clearance rate and incidence of PIH, the 532 nm PS laser seems to be the more effective and safer treatment.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download