Dear Editor:
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare, highly aggressive hematopoietic malignancy which is derived from the precursors of plasmacytoid dendritic cells1. It was recently classified in the 2008 World Health Organization classification2. BPDCN can be characterized by a marked predilection for cutaneous involvement in the initial phase, and later develops leukemic dissemination3.
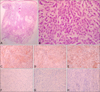
A previously healthy 43-year-old woman presented with 3-week history of nodular eruptions on the face. She had no systemic symptoms. Physical examination did not reveal any abnormalities, except for the skin lesions. Skin examination revealed multiple various-sized erythematous plaques and nodules on the face (Fig. 1). We obtained informed consent for using the photos from the patient. Histopathologic findings showed a diffuse cellular infiltrate in the entire dermis (Fig. 2A). The cells were monomorphic medium sized atypical lymphocytes containing irregular round or indented nuclei with pale cytoplasm (Fig. 2B). Immunohistochemical stains were positive for CD4 (Fig. 2C), CD56 (Fig. 2D), and CD123 (Fig. 2E) and negative for CD3 (Fig. 2F), CD20 (Fig. 2G), myeloperoxidase (Fig. 2H), and terminal deoxynucleotidyl transferase. Microscopic examination of peripheral blood failed to detect neoplastic cells. Abdominal computed tomography scan disclosed wall thickening of gallbladder (GB). After cholecystectomy, GB involvement of BPDCN was identified by biopsy. Bone marrow biopsy with immunohistochemical stain also revealed anaplastic cells. Thus, BPDCN with skin, GB and bone marrow involvement was diagnosed. The patient received chemotherapy after lymphoblastic lymphoma-type induction protocol. She subsequently underwent allogeneic bone marrow transplantation. There has been no disease progression following 12 months.
BPDCN is a rare hematologic malignancy typically affects older males4. In majority of cases, skin is affected at the initial presentation as bruise-like tumefaction or an erythematous nodule15. BPDCN is often accompanied by extracutaneous involvement, including bone marrow, lymph node, and peripheral blood but practically any organ can be affected1. Our patient presented with multiple erythematous nodules on the face, which is a rare pattern in BPDCN to the best of our knowledge15. After review of the literature, we believe that the GB involvement described herein has not been documented before.
Pathologic evaluation and immunophenotyping play an important role in the diagnosis of BPDCN, which are characterized by a diffuse monomorphic infiltrate of medium-sized plasmacytoid cells and the expression of CD4, CD56, and CD123 in the absence of CD3, CD20, or myeloperoxidase34.
The clinical course of BPDCN is aggressive with a median survival of 12~14 months15. However, there is no standardized therapeutic strategy. High-dose chemotherapy followed by allogeneic stem cell transplantation can provide durable disease control like our patient1. Several factors, including relatively young age and undergoing stem cell transplantation may contribute to more favorable prognosis in this case.
In conclusion, BPDCN may demonstrate various clinical presentations, which could be quite confusing for the dermatologist to diagnose. Thus histopathologic evaluation of skin biopsy is important to confirm diagnosis. We believe that this case demonstrates a rare cutaneous and extracutaneous presentation of BPDCN and emphasizes the importance of being aware of this rare disease in order to provide effective treatment.
Figures and Tables
Fig. 2
(A) The tumor is composed of diffuse cellular infiltrate in the entire dermis and subcutis, with an overlying Grenz zone (H&E, ×40). (B) The cells were monomorphic medium sized atypical lymphocytes containing irregular round or indented nuclei with pale cytoplasm (H&E, ×400). Immunohistochemical stains were positive for (C) CD4 (×100), (D) CD56 (×100), and (E) CD123 (×100) and negative for (F) CD3 (×100), (G) CD20 (×100), and (H) myeloperoxidase (×100).
References
1. Kim JH, Park HY, Lee JH, Lee DY, Lee JH, Yang JM. Blastic plasmacytoid dendritic cell neoplasm: analysis of clinicopathological feature and treatment outcome of seven cases. Ann Dermatol. 2015; 27:727–737.

2. Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005; 105:3768–3785.

3. Gera S, Dekmezian MS, Duvic M, Tschen JA, Vega F, Cho-Vega JH. Blastic plasmacytoid dendritic cell neoplasm: evolving insights in an aggressive hematopoietic malignancy with a predilection of skin involvement. Am J Dermatopathol. 2014; 36:244–251.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download