This article has been corrected. See "Erratum: Treatment and Classification of Nevus of Ota: A Seven-Year Review of a Single Institution's Experience" in Volume 29 on page 666.
Abstract
Background
Nevus of Ota (NO) is a relatively common pigmentary disorder in Asians. Tanino's classification is an old but tacit consensus to delineate the disease. Various treatment options have been presented. However, a few studies have been conducted on available laser options and current treatment strategies or the classification of NO.
Objective
To investigate current laser options and their effectiveness for the treatment of NO, contributing factors to clinical outcomes, and verification of classification.
Methods
A retrospective study of NO was conducted by reviewing medical charts and photographs of sixty-seven patients. Statistical analysis was used to compare excellent and poor outcomes and determine contributing factors.
Results
The median age of onset was below the age of 1 (interquartile range [IQR], 0~1). Tanino's and PUMCH classification systems failed to classify patients in 24 (35.8%) and 6 (9.0%) of patients, respectively. A 1,064 nm Q-switched Nd:YAG laser without additional lasers was used most frequently in 42 patients (62.7%). The frequency of treatment was 19.0 (IQR, 10.0~23.0) in the cured group defined as subjects showing 95% improvement or above, compared to 10.0 (IQR, 6.25~13.75) in the unattained group defined as subjects showing less than 95% improvement (p=0.001).
Conclusion
A 1,064 nm Q-switched Nd:YAG laser is a reliable treatment armamentarium, functioning as a single infallible modality as well as a combination treatment modality for NO. Repetitive laser treatments without interruption seems to be the most suitable in clearing NO. The current classification systems of NO are defective. Thus, a new classification should be developed.
Nevus of Ota (NO), or oculodermal melanocytosis, affects about 0.02%~0.8% of Asians. However, it is rarely present in white populations12. Pathologically, it is a dermal melanocytic hamartoma that presents with unilateral or bilateral, brown or blue discoloration on the facial skin innervated by the trigeminal nerve23. To date, a variety of treatments for this ‘infamous’ patch on the face have been introduced4. In the early phase, cryosurgery, surgical excision, skin grafting and dermabrasion are typically employed5. Since the development of laser technology, several lasers have been introduced into the treatment of benign pigmentary lesions. Notably, Q-switched (QS) laser systems have gained popularity in the treatment of NO as they produce less scarring and better outcomes6. Nonetheless, the introduction of various treatment options for NO have made it difficult for dermatologists to choose the best solution in practice.
Tanino's classification has been widely accepted by dermatologists to classify NO. It was coined by Tanino in 1939, who observed several patients with NO and divided these cases into types by the extent of skin involvement7. Until now, many studies concerning NO were performed and discussed using Tanino's classificaition289. However, several studies have demonstrated that Tanino's classification leaves a considerable portion of patients unexplained1011. Variants unclassified by conventional classification have been reported and therefore have revealed the weaknesses of the original version of Tanino's classifications. Several new classifications have been suggested, but have not drawn much attention yet1112. In this context, we attempted to present an overview of our experience concerning laser modalities for the treatment of NO, clinical outcomes, and factors affecting the results. In addition, we analyzed the current classification systems in a literature review.
From 2009 to 2015, 67 patients were retrospectively identified who had visited Kangbuk Samsung Hospital, Seoul, South Korea for the treatment of NO. The study also included the participants who were involved in the authors' previous reports613. Compared to our previous studies, which chose patients treated with a single laser modality only, patients treated with multiple different laser modalities were included since the aim of our present research was to extend our knowledge of what types of lasers are used in a real practice and to investigate the difference in prognosis between laser systems. The study protocol was approved by the institutional review board of Kangbuk Samsung Hospital (KBSMC IRB 2015-08-023).
A retrospective review was conducted by two dermatologists, who were not informed of the clinical details regarding the treatment or the patients. Electronic medical charts and photographs taken at each visit were reviewed. The following recorded characteristics were evaluated: sex, age at first treatment, age of onset, color of the NO, involvement of the eyelid and treatment modalities other than laser therapy. Also, laser treatment related factors included in the assessment were the number of laser modalities used and the number of treatment sessions. Objective clinical assessments were performed by two dermatologists who evaluated the photographs taken at the first visit and last visit and classified as follows: cured or excellent, 95%~100% improvement; good, 75%~94% improvement; fair, 50%~74% improvement; poor, 25%~49% improvement; no change, 0%~24% improvement. Given the patients' satisfaction with the treatment and the physicians' aim to cure a disease in a real practice, greater than 95% improvement was considered to be a reasonable treatment end point.
Study participants were sorted by three different classification methods: Tanino's classification, in which NO was divided into 7 types according to the skin involvement area: Type Ia, eyelids, periorbital and temporal area; Type Ib, zygomatic area, nasolabial fold and the lower eyelid; Type Ic, forehead area; Type Id, nostril area; Type II, upper and lower eyelids, zygomatic area, cheek, temple area; Type III, scalp, forehead, eyebrow, and nose; Type IV, bilateral8, and the Peking Union Medical College Hospital (PUMCH) classification, a new system developed by a Chinese group in 2013, in which NO was distributed into 5 large categories and 15 subdivisions according to the extent of involvement in innervated areas of the trigeminal nerve branches: Type I, pigmentation involving one branch of the trigeminal nerve; Type II, pigmentation involving two branches of the trigeminal nerve; Type III, pigmentation involving all three branches of the trigeminal nerve; Type IV, bilateral type; Type V, NO accompanied by other cutaneous complications11. For convenience, the authors used a three-point severity scale based on the proportion of the NO on the half face as follows: mild, ≤one third of the half face; moderate, >one third, ≤two thirds and severe, >two thirds.
According to the physicians' personal experience, available equipment and preference, several laser modalities were used including QS neodymium-doped yttrium aluminium garnet (Nd:YAG) lasers (Spectra VRMIII™; Spectra XT™; Lutronic Corp., Goyang, Korea or Pastelle™; Won Tech., Daejeon, Korea), dual pulsed Nd:YAG laser (Pastelle™-photoacoustic twin pulse mode; Won Tech.), picosecond-domain Nd:YAG laser (PNY) (Enlighten™; Cutera, Brisbane, CA, USA), 532 nm potassium-titanylphosphate (KTP) and 1,064 nm long-pulsed Nd:YAG laser (Gemini™; Laserscope Corp., San Jose, CA, USA), 755 nm Alexandrite (AL) and 1,064 nm long-pulsed Nd:YAG laser (Clarity™; Lutronic Corp.), 660 nm QS Nd:YAG laser (660NY) (Spectra XT™-Ruvy Touch mode; Lutronic Corp.), quasi-long-pulsed (190 µsec) Nd:YAG laser (QLNY) (Spectra XT™-Spectra mode; Lutronic Corp.), erbium-doped yttrium aluminium garnet (Er:YAG) laser (AVVIO™; Won Tech.), and intense pulsed light (IPL) (RPL™; Ahwon Medi Instrument, Bucheon, Korea).
Three different QS Nd:YAG laser devices were simultaneously used were considered as a single device as they had similar outcomes. Specific modes in the same laser platform were categorized as different laser systems (e.g., photoacoustic twin pulse mode, PTP; Spectra XT™-Spectra mode). PTP mode refers to a dual-pulse method, in which the pulse is divided into two half-fluence pulses with a 140-µs interval14. With the exception of the laser systems mentioned above, lasers or chemical substances used in irrelevant areas or side effects following laser treatment were excluded.
Statistical analyses were conducted with IBM SPSS Statistics ver. 19.0 for Windows (IBM Co., Armonk, NY, USA). Categorical variables were presented as percentages and compared by using the χ2 and Fisher's exact tests. Mann-Whitney U-test was applied to compare two groups with continuous data in a non-normal distribution. A p-value <0.05 was set as the point of significance.
Among the 67 enrolled patients, gender was almost equally distributed; 30 were males and 37 were females. The median age at diagnosis was 6 years (interquartile range [IQR], 2.8~20.0). The majority of patients had documented NO that had occurred before 1 year of age. Various colors were present on the face although blue and blue brown were slightly dominant. The median number of times that the patients visited our clinic for treatment was 11 sessions (IQR, 7~19; Table 1).
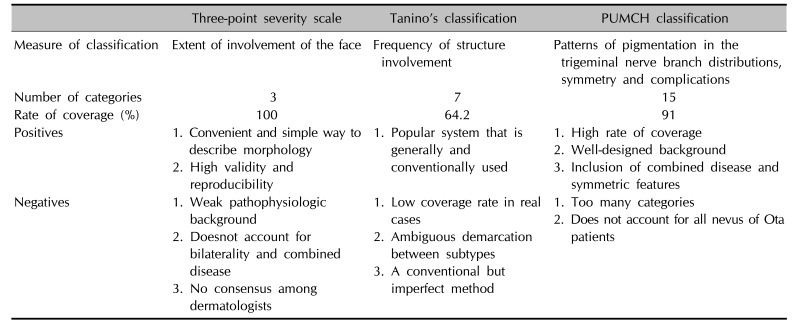
Based on the three-point severity scale, 86.6% of patients demonstrated mild and moderate severity, occupying less than two thirds of the half face (Fig. 1). Tanino's classification was able to classify only 64.2% of patients. However, the PUMCH classification was able to classify 91% of patients. In other words, 18 patients who were not specified with Tanino's classification were able to be sorted by the PUMCH classification (Fig. 2). Six (9.0%) patients remained unspecified when considering both Tanino's and the PUMCH classification (Table 2, Fig. 3). There was no significant association between Tanino's classification, the three-point severity scale or the PUMCH classification and the frequency of an excellent outcome (p=0.295, p=0.493 and p=0.462, respectively).
In our study, the 1,064 nm Q-switched Nd:YAG laser (1,064 QSNY) was a mainstay of treatment for NO as all 67 patients were treated by a 1,064 QSNY more than once. Among the 10 different laser systems, the PTP mode in a 1,064 nm Nd:YAG laser and a 1,064 nm PNY were the two popular types used in combination with a 1,064 QSNY (Fig. 4). For most of our patients, however, a 1,064 QSNY alone (62.7%) was the single most useful modality, as previously described (Table 3)1516.
All patients were treated with appropriate fluences and spot sizes depending on the system used: 1,064 nm QSNY at a 2- to 8-mm spot-size and 0.4~6.0 J/cm2, QLNY at a 7- to 8-mm spot-size and 3.4~4.0 J/cm2, 1,064 nm PTP mode at a 4- to 7-mm spot-size and 4.0~8.6 J/cm2, 532 nm QSNY at a 1.3- to 4.2-mm spot-size and 0.65~1.4 J/cm2, 660 nm QSNY at a 3-mm spot-size and 0.9~1.2 J/cm2, PNY with a pulse duration of 750 picoseconds, using a 6- to 8-mm spot-size and 1.0~3.0 J/cm2, IPL with a fluence of 11.5 or 13.0, or 14.5 J/cm2, 560 nm filters, single or double pulses, 3~4 milliseconds pulse duration and 25~40 milliseconds pulse delay, 755 nm AL with a pulse duration of 0.5 milliseconds, using a 10-mm spot-size and 16 J/cm2, 532 nm KTP with a pulse duration of 19 milliseconds or 25 milliseconds, using 6.0 or 8.0 J/cm2 and Er:YAG at a 4.5-mm spot-size and 5.0 J/cm2.
For adjuvant therapy, cryotherapy and topical hydroquinone were used although only three patients (4.5%) underwent cryotherapy. There were no statistically significant differences between the cryotherapy-treated group and the others. Previously, topical hydroquinone has also been shown to not have significant benefits6.
Patients were sorted into two groups based on the clinical outcomes: the cured group was defined as subjects with excellent or cured results, and the unattained group was defined as all other subjects. Between two groups, the difference in number of treatment sessions was statistically significant, and the cured group required more laser treatment sessions than the unattained group (p=0.001). The cured group (mean, 1.0) was more frequently treated with a single laser modality, such as 1,064 QSNY, compared to the unattained group (mean, 2.0) although this was not statistically significant (p=0.084). The age at the first treatment and eyelid involvement were also not significant, but the cured group was slightly younger and had less eyelid involvement compared to the other group (p=0.682 and p=0.258, respectively). There was no statistically significant difference in severity observed between the cured and unattained groups (p=0.493, Table 4).
A NO is composed of melanocytes distributed between the collagen fibers in the dermis17. Relatively little is known about the underlying mechanism of the treatment of NO with lasers. Theoretically, extremely short bursts emitted by QS lasers are absorbed by melanosomes at a sufficient energy to break down tissue with the lowest collateral thermal damage, referred to as selective photothermolysis5. Our study validates the usefulness of QS lasers as a single effective treatment modality for NO as the results reveal a significant improvement in patients treated with a 1,064 QSNY laser. In addition, laser treatments may not only stimulate laser-induced pigmentary destruction, but also, dermal regeneration of collagen fibers. Thus dermal fibrosis as well as the disappearance of pigmentation following laser irradiation might deter the residual pigment particles from being noticable18. In our study, long pulsed and quasi-long-pulsed laser systems were included as a treatment modality. Despite the small number of cases and inconsistent schedules, we expected that long pulsed lasers would work by stimulating collagen remodeling through combined mechanical and thermal effects19. The IPL with a 560 nm filter also performed based on the suggested mechanism, in which diffuse epidermal necrosis occurs through energy distribution20. The latest 1,064 nm picosecond laser was used with expectations that the shortest pulse duration may facilitate the removal of pigmentation without lateral heat damage. The novel QS 660 nm Nd:YAG laser was thought to function similar to a conventional QS ruby laser. Lastly, an Er:YAG laser was used for only two patients as they seemed to have superficial skin changes over the NO. Notably, 18 patients (26.8%) exhibited a bumpy skin surface to varying degrees. In this regard, it is recommended that improving pigmentation as well as skin roughness should be taken into consideration in the treatment of NO. Unlike other researchers, our study included all the patients treated with multiple laser modalities, which demonstrated the possibilities of various combinations with QS lasers.
Since 1939, Tanino's classification has been used to describe NO7. Basically, the classification is based on the severity of the disease according to arbitrarily divided areas of the face. The flaws of Tanino's method included ambiguity of the body parts, low coverage rate and acceptance without consensus. A few authors have attempted to define a new standard12. Huang et al.11 recently discovered that 19.74% of patients with a NO were not sorted with Tanino's classification, which is less than 35.8% in our study. The study added the innervated area of the trigeminal nerve to the existing classification. It also took into account the symmetry of pigmentation and NO related complications, such as hemangiomas and vitiligo11. Although all 1,139 patients in the study were able to be organized with the new classification, referred to as the PUMCH classification, six patients (9.0%) were still not able to be classified with the PUMCH classification. In addition, 15 subtypes may seem excessive and, therefore, another drawback. Tanino's and PUMCH classification systems are also not correlated with clinical outcomes, as the severity scale is. At this point, there is no ideal classification system (Table 5).
The possible factors that influence the results of the study were identified in the current literature: eyelid lesions, Tanino's classification, number of treatment sessions, a bilateral nevus, skin phototype, color of the lesion, and age at the first treatment261618. Our results revealed that the frequency of treatments was the key factor, which confirmed that more treatments would result in better outcomes, which is in agreement with other studies216. On the other hand, no significant correlation was revealed between the presence of an eyelid lesion and the severity or classification and clinical outcomes. These results can be corroborated by Zong and Lin's finding9, in which Tanino's classification had no relationship with the cure rate, although Wang et al.2 found that eyelid lesions and Tanino's classification were correlated with clinical outcomes.
In addition, the present analysis did not show any significant difference between age at the first treatment and clinical results, which is not consistent with the results of our previous study6. It was speculated that various laser combinations without homogeneity may affect the results and attenuate significance. Also, our treatment standard was set high at 95% or above improvement, to meet the patients' and clinicians' satisfaction in a real practice26. For better cosmetic outcomes, various lasers were selected, but this did not lead to significant differences in outcomes in this study. Even with this slight non-alignment, the results revealed that NO is curable with consistent and repetitive laser treatment.
In most studies, transient pigmentary changes were identified, ranging from 8% to 25.1%, which were consistent with that of 15.0% in our study. Only two (3.0%) patients experienced atrophic scarring, which showed gradual improvements with time.
This project was limited in that it was a retrospective and uncontrolled study, including irregular and unequal treatment intervals as well as variable parameters. Second, the recurrence rate was not able to be analyzed because long term follow-up was not feasible. Third, a small sample size may result in a lack of association with the classifications and outcomes. Lastly, skin biopsies were not performed in most of NO patients; thus, we couldn't evaluate the histopathogical aspects of NO.
Since the aforementioned shortcomings existed in this study, a long-term, controlled prospective study with a large study population is required to determine a new classification system that reflects the pathogenesis and clinical prognosis of NO and to determine the best treatment methods for NO.
Our study confirmed that a 1,064 nm QSNY is an effective modality in the treatment of NO, which can function as a single infallible as well as a combination treatment modality. Various treatment sessions are crucial in order to achieve successful and satisfactory results. Existing clinical classifications are not well suited for real-world application. A new clinical classification system should be developed. Fig. 6. A 3-year-old female patient classified as “moderate” (A) before treatment, and (B) at the final visit after 30 treatments (excellent outcome).
Notes
References
1. Ho SG, Chan HH. The Asian dermatologic patient: review of common pigmentary disorders and cutaneous diseases. Am J Clin Dermatol. 2009; 10:153–168. PMID: 19354330.
2. Wang HW, Liu YH, Zhang GK, Jin HZ, Zuo YG, Jiang GT, et al. Analysis of 602 Chinese cases of nevus of Ota and the treatment results treated by Q-switched alexandrite laser. Dermatol Surg. 2007; 33:455–460. PMID: 17430380.

3. Radmanesh M. Naevus of Ota treatment with cryotherapy. J Dermatolog Treat. 2001; 12:205–209. PMID: 12241629.

4. Kouba DJ, Fincher EF, Moy RL. Nevus of Ota successfully treated by fractional photothermolysis using a fractionated 1440-nm Nd:YAG laser. Arch Dermatol. 2008; 144:156–158. PMID: 18283171.

5. Ono I, Tateshita T. Efficacy of the ruby laser in the treatment of Ota's nevus previously treated using other therapeutic modalities. Plast Reconstr Surg. 1998; 102:2352–2357. PMID: 9858169.

6. Seo HM, Choi CW, Kim WS. Beneficial effects of early treatment of nevus of Ota with low-fluence 1,064-nm Q-switched Nd:YAG laser. Dermatol Surg. 2015; 41:142–148. PMID: 25485806.
7. Ota M, Tanino H. Nevus fusco-caeruleus ophthalmo-maxillaris. Tokyo Med J. 1939; 63:1243–1245.
8. Choi JE, Lee JB, Park KB, Kim BS, Yeo UC, Huh CH, et al. A retrospective analysis of the clinical efficacies of Q-switched Alexandrite and Q-switched Nd:YAG lasers in the treatment of nevus of Ota in Korean patients. J Dermatolog Treat. 2015; 26:240–245. PMID: 24888365.

9. Zong W, Lin T. A retrospective study on laser treatment of nevus of Ota in Chinese children--a seven-year follow-up. J Cosmet Laser Ther. 2014; 16:156–160. PMID: 24684590.

10. Guledgud MV, Patil K, Srivathsa SH, Malleshi SN. Report of rare palatal expression of Nevus of Ota with amendment of Tanino's classification. Indian J Dent Res. 2011; 22:850–852. PMID: 22484884.

11. Huang WH, Wang HW, Sun QN, Jin HZ, Liu YH, Ma DL, et al. A new classification of nevus of Ota. Chin Med J (Engl). 2013; 126:3910–3914. PMID: 24157155.
12. Chan HH, Lam LK, Wong DS, Leung RS, Ying SY, Lai CF, et al. Nevus of Ota: a new classification based on the response to laser treatment. Lasers Surg Med. 2001; 28:267–272. PMID: 11295763.

13. Choi CW, Kim HJ, Lee HJ, Kim YH, Kim WS. Treatment of nevus of Ota using low fluence Q-switched Nd:YAG laser. Int J Dermatol. 2014; 53:861–865. PMID: 23834371.

14. Yoo MG, So BJ, Lee JM, Kim DH, Park HC, Ryu HJ, et al. Influence of pulse type on subcellular selective photothermolysis of melanosomes in adult zebrafish skin following 1,064-nm, Q-switched, Nd:YAG laser irradiation: a pilot study. Ann Dermatol. 2015; 27:230–232. PMID: 25834374.

15. Aurangabadkar S. QYAG5 Q-switched Nd:YAG laser treatment of nevus of Ota: an Indian study of 50 patients. J Cutan Aesthet Surg. 2008; 1:80–84. PMID: 20300349.

16. Kar HK, Gupta L. 1064 nm Q switched Nd: YAG laser treatment of nevus of Ota: an Indian open label prospective study of 50 patients. Indian J Dermatol Venereol Leprol. 2011; 77:565–570. PMID: 21860154.

17. Suh DH, Hwang JH, Lee HS, Youn JI, Kim PM. Clinical features of Ota's naevus in Koreans and its treatment with Q-switched alexandrite laser. Clin Exp Dermatol. 2000; 25:269–273. PMID: 10971482.

18. Ueda S, Isoda M, Imayama S. Response of naevus of Ota to Q-switched ruby laser treatment according to lesion colour. Br J Dermatol. 2000; 142:77–83. PMID: 10651698.

19. Lee YB, Shin JY, Cheon MS, Oh ST, Cho BK, Park HJ. Photorejuvenation using long-pulsed alexandrite and long-pulsed neodymium:yttrium-aluminum-garnet lasers: a pilot study of clinical outcome and patients' satisfaction in Koreans. J Dermatol. 2012; 39:425–429. PMID: 22220934.

20. Wang CC, Sue YM, Yang CH, Chen CK. A comparison of Q-switched alexandrite laser and intense pulsed light for the treatment of freckles and lentigines in Asian persons: a randomized, physician-blinded, split-face comparative trial. J Am Acad Dermatol. 2006; 54:804–810. PMID: 16635661.

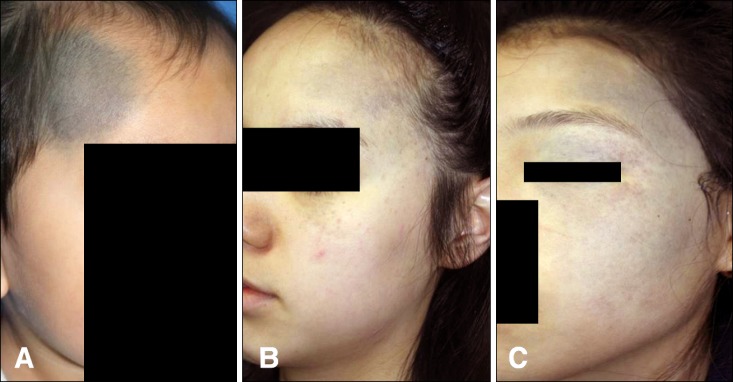
Fig. 2
Clinical images of (A) a 14-month-old male patient and (B) a 12-year-old female patient not specified with Tanino's classification, but specified with the Peking Union Medical College Hospital (PUMCH) classification type IIb and type Ib2, respectively.
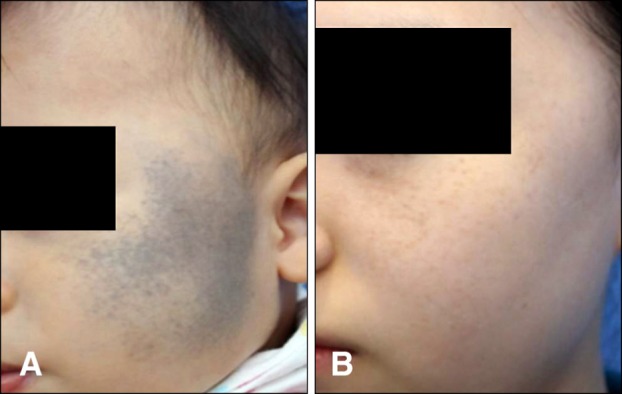
Fig. 3
Clinical images of (A) a 14-month-old male patient and (B) a 6-year-old female patient not specified with both Tanino's and the Peking Union Medical College Hospital (PUMCH) classification.
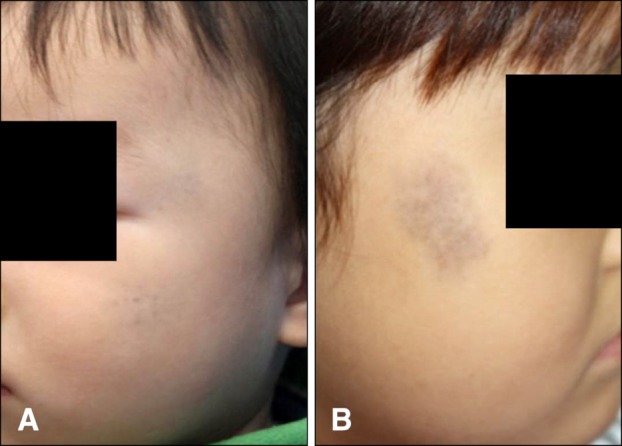
Fig. 4
Common laser combinations in proportion. 1,064 QSNY: 1,064 nm Q-switched neodymium-doped yttrium aluminium garnet (Nd:YAG) laser, 1,064 PTP: 1,064 nm photoacoustic twin pulse mode Nd:YAG laser, 1,064 Pico: 1,064 nm picoseconddomain Nd:YAG laser.
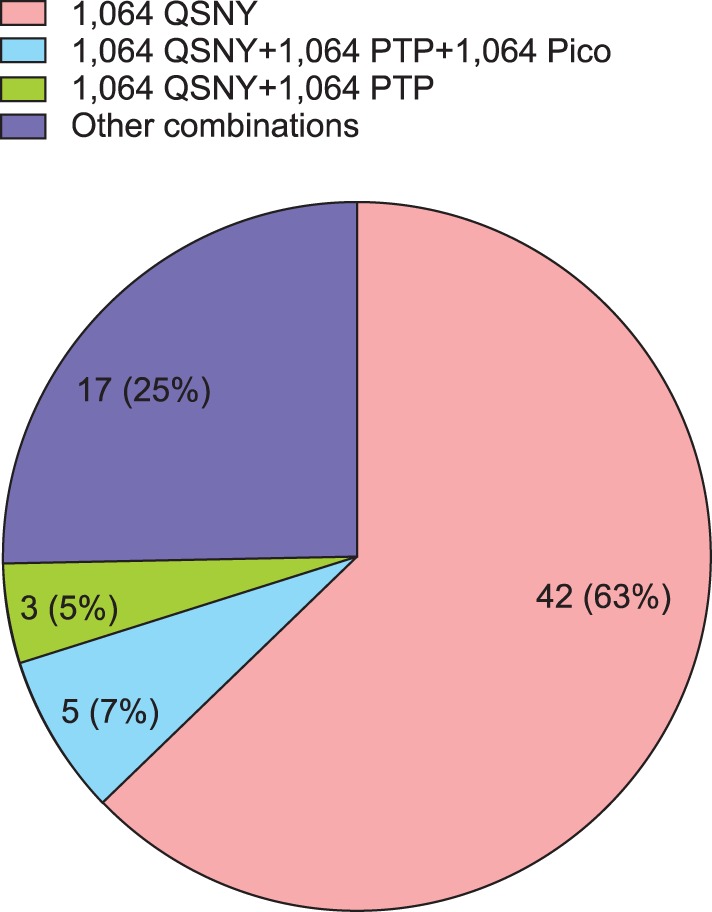
Fig. 5
A 5-year-old male patient classified as “mild” (A) before treatment, and (B) at the final visit after 26 treatments (excellent outcome).
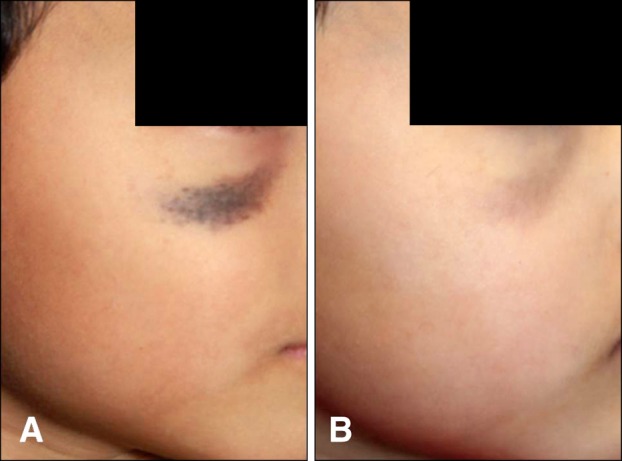
Fig. 6
A 3-year-old female patient classified as “moderate” (A) before treatment, and (B) at the final visit after 30 treatments (excellent outcome).
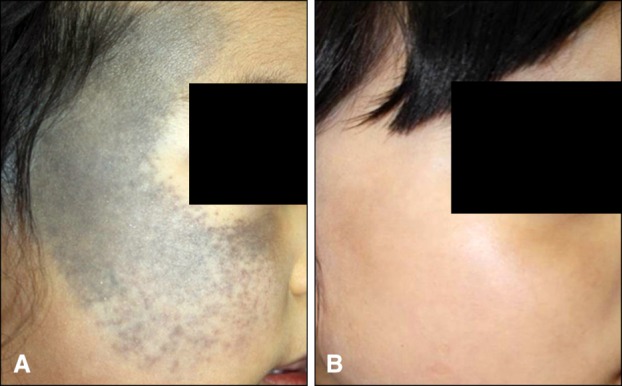
Fig. 7
A 40-year-old male patient classified as “severe” (A) before treatment, and (B) at the final visit after 14 treatments (excellent outcome).
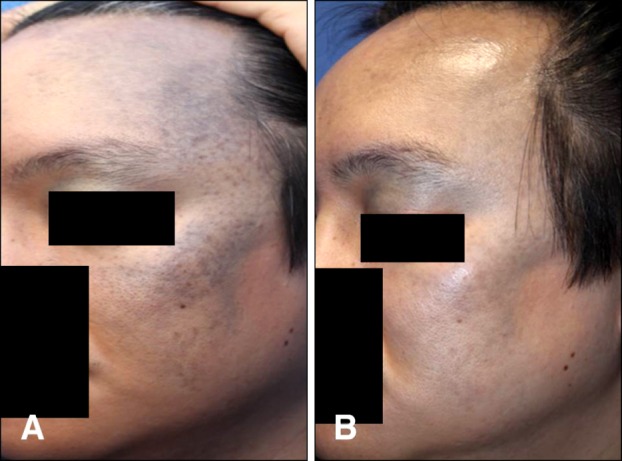
Table 1
Characteristics of the study population (n=67)
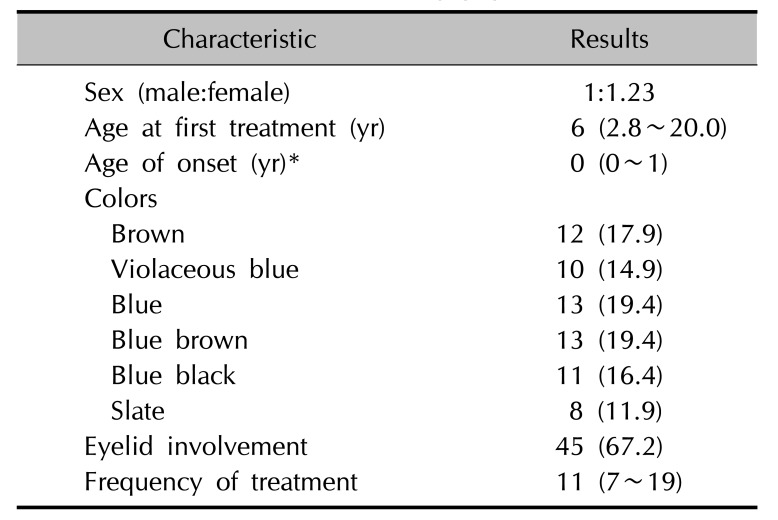
Table 2
Classification of patients by the three-point severity scale, Tanino's classification, and PUMCH classification (n=67)
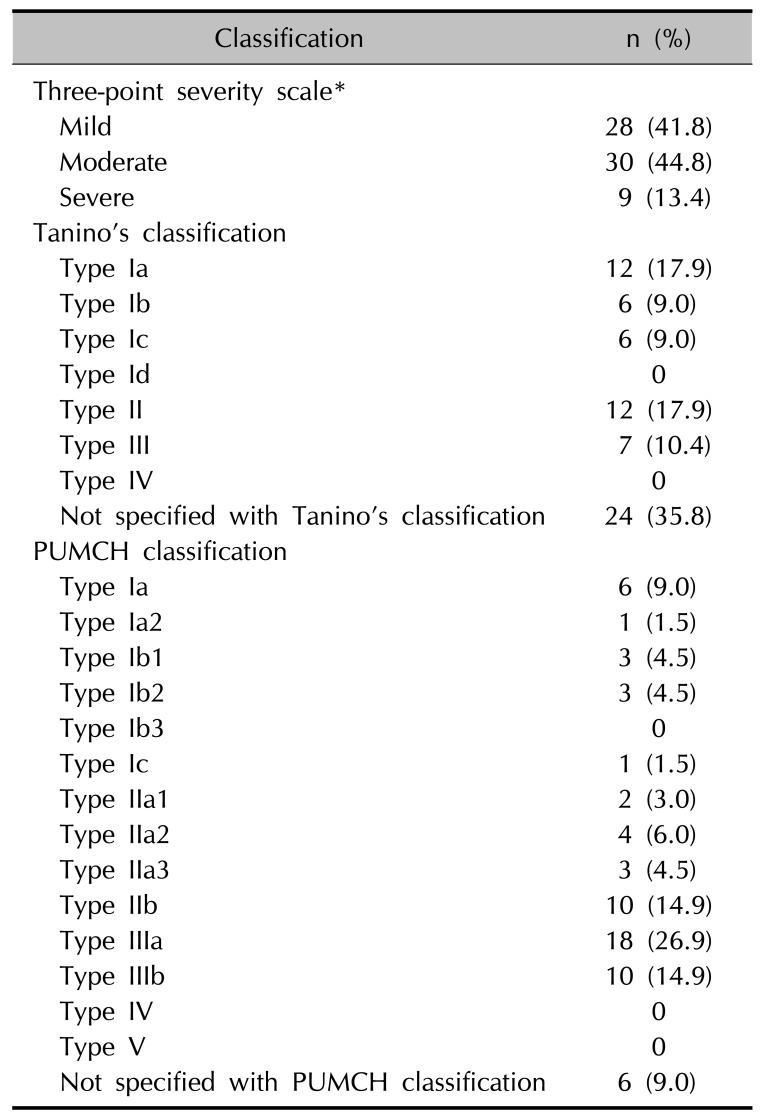
Table 3
Detailed information of patients according to laser combination
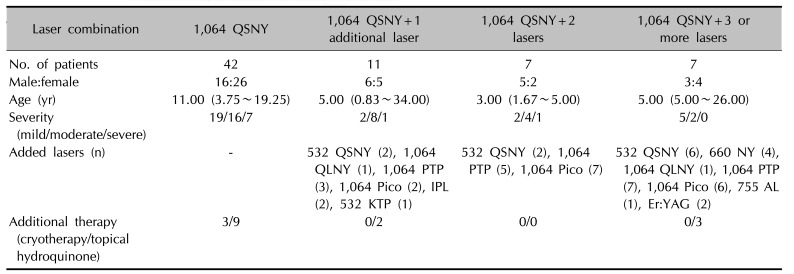
Values are presented as number only or median (interquartile range). 1,064 QSNY: 1,064 nm Q-switched (QS) neodymium-doped yttrium aluminium garnet (Nd:YAG) laser, 532 QSNY: 532 nmQS Nd:YAG laser, 1,064 QLNY: 1,064 nm quasi-long-pulsed Nd:YAG laser, 1,064 PTP: 1,064 nm photoacoustic twin pulse mode Nd:YAG laser, 1064 Pico: 1,064 nm picosecond-domain Nd:YAG laser, IPL: intense pulsed light, 532 KTP: 532 nm potassium-titanyl-phosphate laser, 660 NY: 660 nm QS Nd:YAG laser, 755 AL: 755 nm alexandrite laser, Er:YAG: erbium-doped yttrium aluminium garnet laser.
Table 4
Comparison between the cured (n=27) and unattained groups (n=40)
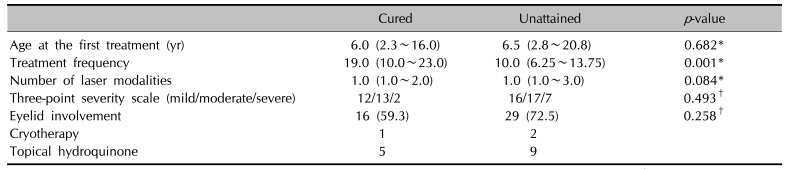
Table 5
Comparison of the nevus of Ota classification methodology




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download