Abstract
Background
Allergic contact dermatitis (ACD), which is accelerated by interferon (IFN)-γ and suppressed by interleukin (IL)-10 as regulators, is generally self-limited after removal of the contact allergen. Adipose tissue-derived multipotent mesenchymal stem cells (ASCs) potentially exert immunomodulatory effects. Considering that subcutaneous adipose tissue is located close to the site of ACD and includes mesenchymal stem cells (MSCs), the MSCs in adipose tissue could contribute to the self-limiting course of ACD.
Objective
The aims of the present study were to elucidate the effects of MSCs in adipose tissue on ACD and to examine any cytokine-mediated mechanisms involved.
Methods
Ear thickness in a C57BL/6 mouse model of ACD using contact hypersensitivity (CHS) elicited by 2,4,6-trinitro-1-chlorobenzene was evaluated as a marker of inflammation level. Five and nine mice were injected with ASCs and phosphate-buffered saline (PBS), respectively. After ASC or PBS injection, real-time reverse transcription-polymerase chain reaction and enzyme-linked immunosorbent assay were performed.
Results
Histology showed that CHS was self-limited and ear thickness was suppressed by ASCs in a dose-dependent manner. IFN-γ expression in the elicited skin site and regional lymph nodes was significantly lower in ASC-treated mice than in control mice. IL-10 expression did not differ between treated and control mice. The suppressive effects of ASCs on CHS response did not differ between IL-10 knock-out C57BL/6 mice and wild-type mice.
Allergic contact dermatitis (ACD) is a manifestation of a type IV delayed hypersensitivity response due to contact with an immune-stimulating substance1. ACD is a type of eczematous dermatitis characterized by clinical findings that include erythema, papules, vesicles, pustules, crusting and scale; the histopathological findings include spongiosis, dermal edema and inflammatory cell infiltration into the dermis. This response reaches a peak 24~48 h after elicitation and is generally self-limited; it attenuates within 2~4 weeks after removal of contact allergens1.
Contact hypersensitivity (CHS) is an in vivo assay in which delayed-type hypersensitive reaction is caused by exposure of epidermal cells to exogenous haptens2. This assay contributes to elucidating constitutive mechanisms in the ACD pathogenesis. ACD is classified into two phases: an induction phase and an elicitation phase1,3. In the induction phase, hapten-protein conjugates are internalized by antigen-presenting cells such as Langerhans cells, transported to the skin-draining lymph nodes, and presented to T-cells. These T-cells subsequently recognize the antigen epitope, clonally divide, and differentiate into effector cells such as interferon (IFN)-γ-producing CD8+ cytotoxic T-cells (Tc1). In the elicitation phase, local antigen-presenting cells recognize the antigen/major histcompatibility complex complexes when the allergen is in contact with the skin. In the early stage, tumor necrosis factor (TNF)-α, secreted mainly from effector T-cells, induces various cytokines/chemokines, including interleukin (IL)-8 and chemokine (C-C motif) ligand 5 from inflammatory cells. In the later stage, IFN-γ, secreted mainly from effector cells, recruits various types of inflammatory cells4.
In the suppressive regulation of the CHS response, regulatory T cells (T-regs) are known to play pivotal roles5. T-regs are basically classified into two distinct subsets: 1) antigen-specific T-regs, including Tr1 cells secreting IL-10 and Th3 cells secreting transforming growth factor (TGF)-β1 and 2) naturally occurring CD4+CD25+ T-regs. Notably, Cavani et al.6 have reported that IL-10 is a main major factor in the self-limitation of the CHS response.
Mesenchymal stem cells (MSCs) are prototypical adult stem cells with a capacity for self-renewal and differentiation into various tissues7. The International Society for Cell Therapy has proposed the following criteria for human MSCs: 1) adherence to plastic under standard culture conditions; 2) expression of CD73, CD90, and CD105 surface molecules in the absence of surface molecules of CD45, CD34, CD14 or CD11b, CD79α or CD19 and human leukocyte antigen; and 3) capacity for differentiation into osteoblasts, adipocytes, and chondroblasts in vitro8.
However, this uniform definition seems unwieldy because 1) these criteria may not apply uniformly to other species, and 2) no unique cell surface markers have yet been identified that unequivocally distinguish MSCs from other hematopoietic stem cells7. Despite such ambiguities in the current definition of MSC, adipose tissue-derived MSCs (ASCs) developed by an established isolation and culture system are widely investigated and used9. The literature investigating these ASCs has described the immune-suppressive effects of ASCs as follows: ASCs improve autoimmune hearing loss in a mouse model10 and prevent acute graft versus host disease1112.
Because subcutaneous adipose tissue is located close to the site of ACD and includes MSCs with potential immunomodulatory effects, MSCs in adipose tissue could contribute to the self-limiting course of ACD. However, the effects of MSCs in adipose tissue on ACD have not been the subject of detailed investigation. The present study examined the effects of MSCs in adipose tissue on ACD.
Female C57BL/6 wild-type mice were purchased from Charles River Japan (Kanagawa, Japan). IL-10-knockout C57BL/6 mice (B6.129P2-Il10tm1Cgn/J, IL-10−/−) were purchased from the Jackson Laboratory (Bar Harbor, ME, USA). Mice were 8~10 weeks old and were housed in a specific pathogen-free barrier facility. All protocols and procedures were approved by the Animal Committees of the National Center for Global Health and Medicine.
Inguinal adipose tissue was isolated from 6- to 8-week-old female wild-type C57BL/6 mice. The tissue was minced into 2- to 3-mm pieces in Dulbecco's modified Eagle's medium (WAKO, Osaka, Japan) containing 10% fetal bovine serum and incubated at 37℃ in a 5% CO2 incubator for 30 min. The suspension was centrifuged at 1,000 rpm for 5 min at room temperature. To dissociate cells, the suspension was treated with 0.12% collagenase type I solution and incubated at 37℃ for 30 min, then centrifuged at 1,000 rpm for 5 min at room temperature. The cells were cultured in Dulbecco's modified Eagle's medium containing 10% fetal bovine serum, 10 units of penicillin, and 10 µg/ml streptomycin (GIBCO, Grand Island, NY, USA) in a CO2 incubator at 37℃. These cells were cultured for fewer than 4 passages and used for the cell transplantation experiments.
C57BL/6 and IL-10−/− mice were sensitized by epicutaneous application of 5 µl of 7% 2,4,6-trinitro-1-chlorobenzene (TNCB; Tokyo Kasei, Tokyo, Japan) onto shaved abdominal skin on day 0. On day 6 after sensitization, the right ear was elicited by applying a volume of 20 µl 1% TNCB. Five hours later, cultured ASCs and phosphate-buffered saline (PBS) or were injected into the tail veins of 5 mice and 9 mice, respectively. Ear thickness was measured for each mouse before elicitation and at 24, 48, 72, and 96 h after elicitation.
Total RNA was isolated from homogenized skin tissue using ISOGEN Reagent (Nippon Gene, Tokyo, Japan) according to the instructions from the manufacturer. Two micrograms of RNA were used for synthesis of cDNA with a cDNA synthesis kit (Applied Biosystems, Foster, CA, USA). Real-time reverse transcription-polymerase chain reaction (RT-PCR) was performed for skin and lymph node tis™sues with Fast SYBR Green Master Mix in a StepOne real time qPCR system (Applied Biosystems) according to the manufacturer's instructions. The quantity of mRNA for each gene was normalized with that of the housekeeping gene ornithine decarboxylase antizyme-1 (Oaz1). The primer sequences and PCR conditions for each of the genes Ifng, Tnf, Il10, Tgfb1, Cd29, Cd90, Cd105 and Oaz1 are described in Table 1.
Protein levels of IFN-γ, TNF-α, IL-10 and TGF-β1 in the blood of mice with CHS injected with ASCs or PBS were determined at 24 h after elicitation by enzyme-linked immunosorbent assay (ELISA) with a Quantikine ELISA kit (R&D Systems, Minneapolis, MN, USA) according to the instructions from the manufacturer. Luminescence intensity was quantified using a plate reader (PerkinElmer, Waltham, MA, USA) at an optical density of 560 nm.
Ear tissues were fixed in paraformaldehyde after euthanasia. Fixed tissues were randomly selected for further evaluation. Tissues were processed by routine methods and embedded in paraffin wax. After deparaffinization, sections (5 µm) were stained with hematoxylin and eosin or toluidine blue (pH 7.0).
For CD4 and CD8α immunohistochemical assays, the frozen samples were cut into 5-µm sections on a cryostat, air-dried for 30 min, fixed in acetone, and blocked in 1.5% rabbit serum. Sections were incubated with rat anti-mouse CD4 monoclonal antibody (R&D Systems) or rat anti-mouse CD8α monoclonal antibody (R&D Systems) overnight at 4℃. Both primary antibodies were detected by biotin-conjugated rabbit anti-rat monoclonal antibody (Vector Lab, Burlingame, CA, USA). After incubation with streptavidin-alkaline phosphatase (Vector Lab), staining was performed using new alkaline phosphatase substrate (Vector Lab). Finally, sections were stained with Meyer's hematoxylin. As a negative control, sections were incubated with blocking buffer without primary antibody; as an isotype control, they were incubated with normal rat IgG instead of primary antibody.
To confirm the self-limiting course of CHS, TNCB-induced ear swelling in C57BL/6 wild-type mice was examined histopathologically. The CHS response was induced by epicutaneous application of TNCB in the ears of C57BL/6 mice previously sensitized with TNCB. Edema and inflammatory cell infiltration in the dermis were distinct at day 2 after elicitation and decreased at day 7, indicating that this CHS offers a reasonable model of ACD with a self-limiting course (Supplementary Fig. 1).
To confirm that our ASCs possess the surface phenotype of MSCs, mRNA expressions of MSC markers of CD29, CD90, and CD105 in the ASCs were examined. The examination revealed that expressions of CD29, CD90, and CD105 in the ASCs are increased compared to those in control tissues (Fig. 1A).
To confirm that MSCs are recruited into the CHS, mRNA expressions of the MSC markers were examined. The results revealed that expressions of CD29, CD90, and CD105 are increased in post-elicitation compared to pre-elicitation (Fig. 1B).
To elucidate the effects of ASCs on CHS, each ASC dose was injected intravenously into a tail vein 5 h after TNCB elicitation on the ear. Ear thicknesses were measured at 24 and 48 h after elicitation, when ACD inflammation generally peaks, and the change in ear thickness was calculated as the value of the pre-elicitation thickness subtracted from that at the examined time point. Mean change values were 169±4 µm in PBS-treated mice, 114±24 µm in 5.0×105 ASC-treated mice and 91±14 µm in 1.0×106 ASC-treated mice at 24 h, and 198±4 µm in PBS-treated mice, 138±19 µm in 5.0×105 ASC-treated mice and 127±9 µm in 1.0×106 ASC at 48 h (Fig. 2A). The examination showed that ASCs dose-dependently suppressed CHS response in vivo. All the mice injected with >1.0×106 ASCs died immediately after ASC injection.
To confirm the suppressive effects of ASCs on the CHS, histopathological examinations for T cells and mast cells were performed (Supplementary Fig. 2). Anti-CD4 and -CD8α antibodies reacted to some inflammatory cells in the elicited skin site of PBS-treated mice and to few inflammatory cells in the elicited skin site of ASC-treated mice. Metachromatic staining was seen in some inflammatory cells in the elicited skin site of PBS-treated mice and in few inflammatory cells in the elicited skin site of ASC-treated mice.
To elucidate the continuity of ASC effects on CHS, 1.0×106 of ASCs or the same volume of PBS was injected intravenously into a tail vein at 5 h after TNCB elicitation on the ear. The change in ear thickness was calculated as the value of the pre-elicitation thickness subtracted from that at the examined time point. Mean change values were 169±4 µm and 91±14 µm in PBS- and ASC-treated mice, respectively, at 24 h, 198±4 µm and 127±9 µm at 48 h, 184±10 µm and 128±10 µm at 72 h, and 163±15 µm and 101±10 µm at 96 h (Fig. 2). This examination showed that ASCs continuously suppressed CHS response in vivo for at least 96 h after elicitation (Fig. 2B).
To clarify the mechanisms underlying the ASC-suppressive effects on CHS, expression analyses of representative pro-inflammatory cytokines (including IFN-γ and TNF-α) and representative anti-inflammatory cytokines (including IL-10 and TGF-β1) were performed.
IFN-γ mRNA expression in the elicited skin site was significantly decreased in ASC-treated mice compared to PBS-treated mice at 8 and 11 h after elicitation and was suppressed in both ACS- and PBS-treated mice at 24 h (Fig. 3A). The differences in mRNA expressions between ASC- and PBS-treated mice at 8 and 11 h after elicitation were confirmed by ELISA. The examination showed that serum levels of IFN-γ were decreased in ASC-treated mice compared to those in PBS-treated mice at 24 h after elicitation (Fig. 3B). To confirm the effects of ASCs on the suppression of IFN-γ in CHS, mRNA expression of IFN-γ in the regional lymph nodes was analyzed. The examination showed that IFN-γ expression in regional lymph nodes was decreased in ASC-treated mice compared to PBS-treated mice at 8 and 11 h after elicitation (Fig. 3C). This suppression of IFN-γ in regional lymph nodes broadly corresponded to that at the elicited skin site.
TGF-β1 mRNA expression at the elicited skin site differed little between ASC- and PBS-treated mice (Fig. 3A). Serum levels of TGF-β1 were increased at 24 h after elicitation in ASC-treated mice compared to those in PBS-treated mice (Fig. 3B).
TNF-α mRNA expression at the elicited skin site and serum levels of TNF-α differed little between ASC- and PBS-treated mice (Fig. 3A, B). IL-10 mRNA expression at the elicited skin site did not indicate any clear tendency (value in ASC-treated mice <value in PBS-treated mice at 11 h; value in ASC-treated mice >value in PBS-treated mice at 24 h) (Fig. 3A), and serum levels of IL-10 showed differed little between ASC- and PBS-treated mice (Fig. 3B).
Because IL-10, as the proposed key molecule for the self-limiting course of ACD, did not show any distinct change in expression levels with ASC treatment, the effects of ASCs in IL-10−/− mice were examined to confirm the absence of a relationship between IL-10 and the suppressive effects of ASCs on CHS response. Change rates in ear thickness for wild-type and IL-10−/− mice were −46.1% and −53.4% at 24 h after elicitation, −35.9% and −43.4% at 48 h, −30.3% and −31.4% at 72 h, and −38.0% and −25.9% at 96 h, respectively (Fig. 4). Statistical analyses revealed equivalence between wild-type and IL-10−/− mice at each examined time point in the change rates representing the suppressive effects of ASCs on CHS response (p>0.05 at each time point).
The present study demonstrated for the first time that ASCs dose-dependently and continuously suppress CHS response in vivo. Since ASCs and CHS represent MSCs in adipose tissue and ACD, respectively, the results suggest that MSCs in adipose tissue may act to suppress ACD.
IFN-γ mRNA expression at 8 and 11 h after elicitation in the elicited skin site and regional lymph nodes and protein expression level at 24 h in blood were decreased in ASC-treated mice compared to control mice. Considering that IFN-γ is an important factor in the elicitation phase4, the suppressive effects of ASCs on CHS response are suggested to depend on inhibition of IFN-γ expression. In our model that was self-limited in harmony with typical ACD with a self-limiting course, IFN-γ mRNA expression was decreased in control mice as well as ASC-treated mice at 24 h after elicitation. This indicates that: 1) the decreased IFN-γ expression is deeply associated with the self-limiting course of ACD without any intervention, as well as with the course with the intervention of ASC treatment; and 2) ASC intervention enhances the mechanisms leading to the self-limiting course by more rapidly decreasing IFN-γ expression.
The present study showed that: 1) IL-10 mRNA expression levels at the elicited skin site did not show any clear changes; 2) IL-10 protein expression levels in blood differed little between ASC- and PBS-treated mice; and 3) the suppressive effects of ASCs on CHS response were equivalent between wild-type and IL-10−/− mice. The mechanisms by which MSCs in adipose tissue suppress ACD may not be associated with IL-10. On the other hand, IL-10 is reported to be a natural suppressant of cutaneous inflammatory responses, based on examinations using CHS of C57BL/6 mice13. IL-10 might thus be associated with ACD suppression through mechanisms other than MSCs in adipose tissue.
The present study showed a marked up-regulation of TGF-β1 protein expression in response to ASC treatment, although mRNA expression levels did not show clear changes. Bobr et al.14 reported that TGF-β1 inhibits inflammation-induced migration of Langerhans cells. Up-regulation of TGF-β1 protein expression by ASCs might thus result in impaired antigen presentation to T cells by inhibiting migration of Langerhans cells. On the other hand, neither RT-PCR nor ELISA showed distinct changes to TNF-α expression levels with elicitation and ASC treatment. Sebastiani et al.4 reported that TNF-α plays important roles in the early stage of ACD. Because TNF-α expression did not change with either elicitation or ASC treatment, TNF-α might not be associated with either the anti-inflammation mechanism or the pro-inflammation mechanism, at least in this CHS response. This might represent a limitation of our model.
Histopathological examination revealed that CD4+ T cells, CD8+ T cells, and mast cells were decreased in elicited skin sites of ASCs treated mice compared to PBS-treated mice. Such decreases in Th1 cells (CD4+ T cells) and IFN-γ-producing CD8+ T cells may contribute to suppression of IFN-γ in ASC-treated mice. Mast cells possess a variety of chemical mediators associated with vascular permeability, including histamine, proteases and prostaglandins15. Ear thickness is deeply associated with tissue edema. Therefore, a decrease in mast cells may contribute to the inhibition of ear thickness in ASC-treated mice.
C57BL/6 and BALB/c mice are prototypical mouse strains with Th1- and Th2-type predominant responses, respectively16. Considering the possibility that the Th1-type response of ACD elicited with TNCB may be more prominently induced in C57BL/6 mice than in BALB/c mice17, we selected C57BL/6 stimulated with TNCB as a model of ACD.Because the CHS response peaks 24~48 h after elicitation, inflammation-related protein expressions were examined at 24 h and the mRNA expressions were examined before protein expression analyses. The resulting data between mRNA expressions and protein expressions for each molecule were broadly compatible, except for TGF-β1.
A limitation to the present study must be considered. To elucidate the effects of MSCs, a large quantity of ASCs was administered to the mice. In practical terms, relatively few MSCs may reside in the tissue compared to the number of ASCs administered. The effects of MSCs on ACD in the actual tissue might thus be less than suggested by this study.
In conclusion, the present study suggests that MSCs in adipose tissue may contribute to the self-limiting course of ACD through suppressive regulation. The suppressive effects of MSCs in adipose tissue on ACD are likely attributable to mechanisms mediated by IFN-γ and TGF-β1, but not by IL-10.
Figures and Tables
Fig. 1
Increased levels of mesenchymal stem cell (MSC) markers in the adipose tissue-derived multipotent MSCs (ASCs) and contact hypersensitivity. (A) Expressions of CD29, CD90, and CD105 in the ASCs were examined with real-time reverse transcription-polymerase chain reaction (RT-PCR). Vertical axis indicates expression levels standardized with OAZ1 expression. Mouse ear tissues were used as controls. (B) Expression of CD29, CD90, and CD105 in the ASCs were examined with RT-PCR. Values are presented as means±standard error of the mean. Vertical and horizontal axes indicate expression levels standardized with OAZ1 expression and 0, 5, and 29 h after elicitation, respectively.

Fig. 2
Suppressive effects of adipose tissue-derived multipotent mesenchymal stem cells (ASCs) on contact hypersensitivity (CHS) response. Values are presented as mean change and standard error of the mean. Each treatment group included ≥5 C57BL/6 mice sensitized with 2,4,6-trinitro-1-chlorobenzene (TNCB). The change in ear thickness was determined as the pre-treatment thickness subtracted from that at the examined time point. Significant differences between samples are indicated: *p<0.05, **p<0.01. (A) Dose-dependent effects of ASCs on CHS response. Mean changes in ear thicknesses of mice injected with 0, 5×105, or 1×106 ASCs at 24 and 48 h after elicitation. Vertical and horizontal axes indicate changes in ear thickness (µm) and ASC dose, respectively. (B) Continuous effects of ASCs on CHS response. Mean changes in ear thickness of mice injected with 1×106 ASCs or phosphate-buffered saline (PBS) at 0, 24, 48, 72, and 96 h after elicitation. Vertical and horizontal axes indicate changes in ear thickness (µm) and examined time points, respectively. Circle symbol and dotted line indicate values for PBS-treated mice. Triangle symbol and solid line indicate values for ASC-treated mice.

Fig. 3
Change of cytokine expression with adipose tissue-derived multipotent mesenchymal stem cell (ASC) treatment. (A) Expressions of interferon (IFN)-γ, tumor necrosis factor (TNF)-α, interleukin (IL)-10 and transforming growth factor (TGF)-β1 mRNA in the elicited skin sites were examined with real-time reverse transcription-polymerase chain reaction (RT-PCR). Vertical and horizontal axes indicate expression levels standardized with OAZ1 expression and time points (hours) with treatment of ASC(+) or phosphate-buffered saline (PBS)(−), respectively. Values are presented as means±standard error of the mean (SEM). Each treatment group included ≥3 C57BL/6 mice sensitized with 2,4,6-trinitro-1-chlorobenzene (TNCB). (B) Serum levels of IFN-γ, TNF-α, IL-10, and TGF-β1 were examined with enzyme-linked immunosorbent assay. Vertical and horizontal axes indicate concentration level and treatment as ASC(+) or PBS(−), respectively. Each treatment group included ≥3 C57BL/6 mice sensitized with TNCB. (C) mRNA expression of IFN-γ in regional lymph nodes was examined with RT-PCR. Vertical and horizontal axes indicate expression levels standardized with OAZ1 expression and time points with the treatment as ASC(+) or PBS(−), respectively. Values are presented as means±SEM. Each treatment group included ≥3 C57BL/6 mice sensitized with TNCB.

Fig. 4
Comparison between wild-type and interleukin-10−/− mice in adipose tissue-derived multipotent mesenchymal stem cell (ASC) effects on contact hypersensitivity. Change rates in ear thicknesses in wild-type (WT) and interleukin-10-knockout (KO) mice treated by ASCs are indicated. The change rate was defined as the difference between average ear thickness of ASC-treated mice and that of phosphate-buffered saline (PBS)-treated mice divided by average ear thickness of the PBS-treated mice. Equivalence between WT and KO at each examined time point was tested using the chi-square statistics. Each treatment group included ≥10 C57BL/6 mice sensitized with 2,4,6-trinitro-1-chlorobenzene (TNCB). Standard error of the mean was not given, because change rate was calculated using average values in every treatment group.
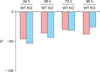
Table 1
Primers for RT-PCR

ACKNOWLEDGMENT
We would like to thank Satsuki Fukuda, Fujie Takeda, and Kiyoko Nashiro from the Department of Regenerative Medicine at the National Center for Global Health and Medicine, for their invaluable technical assistance. We are grateful to Dr. Barbara Lee Smith Pierce (University of Maryland University College) for editorial work in the preparation of this manuscript.
References
1. Saint-Mezard P, Rosieres A, Krasteva M, Berard F, Dubois B, Kaiserlian D, et al. Allergic contact dermatitis. Eur J Dermatol. 2004; 14:284–295.

3. Tončić RJ, Lipozenčić J, Martinac I, Gregurić S. Immunology of allergic contact dermatitis. Acta Dermatovenerol Croat. 2011; 19:51–68.
4. Sebastiani S, Albanesi C, De PO, Puddu P, Cavani A, Girolomoni G. The role of chemokines in allergic contact dermatitis. Arch Dermatol Res. 2002; 293:552–559.

5. Cavani A, Albanesi C, Traidl C, Sebastiani S, Girolomoni G. Effector and regulatory T cells in allergic contact dermatitis. Trends Immunol. 2001; 22:118–120.

6. Cavani A, Nasorri F, Prezzi C, Sebastiani S, Albanesi C, Girolomoni G. Human CD4+ T lymphocytes with remarkable regulatory functions on dendritic cells and nickel-specific Th1 immune responses. J Invest Dermatol. 2000; 114:295–302.

7. Williams AR, Hare JM. Mesenchymal stem cells: biology, pathophysiology, translational findings, and therapeutic implications for cardiac disease. Circ Res. 2011; 109:923–940.
8. Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The international society for cellular therapy position statement. Cytotherapy. 2006; 8:315–317.

9. Konno M, Hamazaki TS, Fukuda S, Tokuhara M, Uchiyama H, Okazawa H, et al. Efficiently differentiating vascular endothelial cells from adipose tissue-derived mesenchymal stem cells in serum-free culture. Biochem Biophys Res Commun. 2010; 400:461–465.

10. Zhou Y, Yuan J, Zhou B, Lee AJ, Lee AJ, Ghawji M Jr, et al. The therapeutic efficacy of human adipose tissue-derived mesenchymal stem cells on experimental autoimmune hearing loss in mice. Immunology. 2011; 133:133–140.

11. Lin CS, Lin G, Lue TF. Allogeneic and xenogeneic transplantation of adipose-derived stem cells in immunocompetent recipients without immunosuppressants. Stem Cells Dev. 2012; 21:2770–2778.

12. Fang B, Song Y, Liao L, Zhang Y, Zhao RC. Favorable response to human adipose tissue-derived mesenchymal stem cells in steroid-refractory acute graft-versus-host disease. Transplant Proc. 2007; 39:3358–3362.

13. Berg DJ, Leach MW, Kühn R, Rajewsky K, Müller W, Davidson NJ, et al. Interleukin 10 but not interleukin 4 is a natural suppressant of cutaneous inflammatory responses. J Exp Med. 1995; 182:99–108.

14. Bobr A, Igyarto BZ, Haley KM, Li MO, Flavell RA, Kaplan DH. Autocrine/paracrine TGF-β1 inhibits Langerhans cell migration. Proc Natl Acad Sci U S A. 2012; 109:10492–10497.

15. Wernersson S, Pejler G. Mast cell secretory granules: armed for battle. Nat Rev Immunol. 2014; 14:478–494.

SUPPLEMENTARY MATERIALS
Supplementary data can be found via https://anndermatol.org/src/sm/ad-29-391-s001.pdf.
Supplementary Fig. 1
Histopathological findings for contact hypersensitivity. Histopathological examination with H&E stain was performed for the elicited skin site on mice. Figures show representative images before elicitation (A), 2 days after elicitation (B), and 7 days after elicitation (C). Horizontal bar indicates 500 µm.
Supplementary Fig. 2
Immunohistochemical analysis of contact hypersensitivity. Histopathological examinations using anti-CD4 antibodies, anti-CD8 antibodies, and toluidine blue staining were performed for the elicited skin site on mice. Figures show representative images of the elicited skin sites in adipose tissue-derived multipotent mesenchymal stem cell (ASC)-treated and phosphate-buffered saline (PBS)-treated mice 24 h after the elicitation. Horizontal bar indicates 100 µm.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download