Abstract
Eccrine squamous syringometaplasia (ESS) is a histologically distinctive skin eruption occurring predominantly in acral or intertriginous areas presenting as erythematous macules, papules or patches. The etiology of ESS remains unclear, but it is usually reported in patients receiving chemotherapy for various malignant neoplasms. To date, only two cases of ESS associated with non-steroidal anti-inflammatory drugs (NSAIDs), which has distinctive clinical features and pathogenesis, have been reported in the literature. Herein, we report a rare and interesting case of ESS associated with pelubiprofen, a recently developed NSAID, which appeared after pelubiprofen therapy and resolved spontaneously after discontinuing the medication.
Metaplasia is a process in which one cell type is transformed into another in an adaptive cellular mechanism in response to various stimuli. One of the common metaplasia in the skin is eccrine squamous syringometaplasia (ESS)1. ESS is histologically defined as metaplasia of the normal eccrine duct epithelium into two or more layers of squamous epithelial cells2. It has been described in patients receiving chemotherapeutic agents for various malignant neoplasms, however, several infectious, neoplastic and inflammatory skin diseases have been found to induce ESS as well3. To date, there has been only two reported cases of ESS associated with non-steroidal anti-inflammatory drugs (NSAIDs) in the literature4. Herein, an unusual case of ESS associated with pelubiprofen, a recently developed NSAID, is presented.
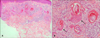
An 83-year-old woman presented with multiple erythematous papules on the neck, forehead and hair line of scalp, which abruptly appeared and grew in size (Fig. 1). The lesion was mildly pruritic and lasted for 10 days. She underwent a surgical repair of femur neck fracture 15 days prior, and pelubiprofen was administered 5 days before skin eruption. She had no other general symptoms such as fever, chills, or malaise and no other remarkable medical history except hypertension with calcium channel blocker since 2009. Biopsy specimens were taken from the forehead and neck lesions with the impression of syringoma, and histopathologic evaluation showed numerous tubular structures and cellular infiltrations in the superficial dermis. The structures consisted of several layers of cells with uniform ductal epithelial proliferation and somewhat large squamous cells with round or oval nuclei and abundant eosinophilic cytoplasm with neither mitosis nor atypia. Relatively sparse inflammatory infiltrates containing lymphocytes, histiocytes, and a few neutrophils were noted around and within ductal structures (Fig. 2). These histopathological changes were consistent with ESS. Pelubiprofen therapy was discontinued immediately, and all the lesions resolved spontaneously over the following 4 weeks (Fig. 3).
ESS has been described in association with various conditions and drugs, particularly in patients receiving chemotherapy3. It typically presents as multiple, pruritic, erythematous papules, plaques, or vesicles usually on the axillae and groin234. Histological features of ESS associated with chemotherapy show both typical findings of ESS and epidermal changes of chemotherapy such as epidermal dystrophy, neutrophil eccrine hidradenitis, and necrosis of eccrine ducts2. Although the pathogenesis of ESS remains unclear, it might represent a nonspecific reaction by damaged epithelial dermal ducts. In cases associated with drugs, the concentration and excretion of drugs in the eccrine duct are believed to trigger the toxic reaction in the ductal epithelium. This can be explained by the localization of these lesions in areas rich in eccrine glands5678.
In 1987, two cases of ESS associated with benoxaprofen, one of NSAIDs which was withdrawn from the market in 1982 after a few reports of fatal cholestatic hepatitis, were published in the literature4. Present case is the first case of ESS induced by pelubiprofen. Pelubiprofen is a propionic acid-derived NSAID that is related both structurally and pharmacologically to ibuprofen. The Korean Ministry of Food and Drug Safety approved pelubiprofen for relieving the symptoms of osteoarthritis in 2007 and approved expanded indications for the relief of back pain in 2010. In these three cases of NSAIDs-associated ESS including present case, in contrast to chemotherapy-associated ESS, the lesions were distributed in sun-exposed areas such as face and neck, but not flexural areas, and epidermal changes such as erosion or necrosis were not observed, which implies that the reaction was not due to non-specific toxic damage of medication9. Several NSAIDs are known to have phototoxic reaction. Among these NSAIDs classes, propionic acid-derivatives such as ibuprofen, ketoprofen, benoxaprofen and pelubiprofen are the most potent phototoxic agents10. Lerner et al.4 postulated that benoxaprofen is secreted in sweat, causing selectively elevated drug levels in eccrine keratinocytes and hence, increased phototoxicity of these cells. Our case supports this postulation that NSAIDs-associated ESS is due to metaplasia possibly caused by phototoxic mechanism.
In conclusion, this is the third case of ESS associated with NSAIDs. We suggest that the pathogenesis of NSAIDs-associated ESS is a phototoxic reaction and although there had not been many reports of phototoxicity, clinicians should be aware that frequently prescribed NSAIDs, in particular derivatives of propionic acids, can induce phototoxic reaction, ESS, as an unusual clinical presentation.
Figures and Tables
References
1. King DT, Barr RJ. Syringometaplasia: mucinous and squamous variants. J Cutan Pathol. 1979; 6:284–291.

2. Kim J, Kim SH, Lee MG, Chung KY, Kim DS. Eccrine squamous syringometaplasia of underlying syringoma associated with Tegafur/Gimeracil/Oteracil (TS-1). Acta Derm Venereol. 2015; 95:999–1000.

3. Martorell-Calatayud A, Sanmartín O, Botella-Estrada R, Balmer NN, Serra-Guillén C, Gomez-Moyano E, et al. Chemotherapy-related bilateral dermatitis associated with eccrine squamous syringometaplasia: reappraisal of epidemiological, clinical, and pathological features. J Am Acad Dermatol. 2011; 64:1092–1103.

4. Lerner TH, Barr RJ, Dolezal JF, Stagnone JJ. Syringomatous hyperplasia and eccrine squamous syringometaplasia associated with benoxaprofen therapy. Arch Dermatol. 1987; 123:1202–1204.

5. Gallo E, Llamas-Velasco M, Navarro R, Fraga J, García-Diez A. Eccrine squamous syringometaplasia secondary to cutaneous extravasation of docetaxel: report of three cases. J Cutan Pathol. 2013; 40:326–329.

6. Moreno de Vega MJ, Dauden E, Abajo P, Bartolome B, Fraga J, Garcia-Diez A. Skin necrosis from extravasation of vinorelbine. J Eur Acad Dermatol Venereol. 2002; 16:488–490.

8. El-Fidawi G, Akel R, Abbas O. Eccrine squamous syringometaplasia in a patient with plaque-type morphea. J Cutan Pathol. 2014; 41:548–549.

9. Han KD, Oh CW, Yoon TJ, Kim TH. A case of phototoxicity due to hydrochlorothiazide. Ann Dermatol. 1998; 10:289–292.

10. Ljunggren B. Propionic acid-derived non-steroidal antiinflammatory drugs are phototoxic in vitro. Photodermatol. 1985; 2:3–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download