Abstract
Leiomyosarcomas are uncommon malignant smooth muscle tumors, mainly derived from vessels or viscera. Superficial leiomyosarcomas are a rare soft tissue sarcoma arising from the dermis or subcutaneous tissue in the skin. According to tumor origin and location, they are divided into cutaneous and subcutaneous leiomyosarcoma. They have distinctly different histologic and prognostic features from each other. Superficial leiomyosarcomas show a predilection for the proximal extremities and tend to be slow growing. We report one rare case of superficial cutaneous leiomyosarcoma on the right temporal area of face, which showed an extremely rapid growing mass within 3 months.
Leiomyosarcomas account for 7% of soft tissue sarcomas, predominantly of visceral location such as the uterus, the gastrointestinal tract or the retroperitoneal space1. Of those, superficial leiomyosarcomas are rare, malignant smooth muscle neoplasms that arise in the dermis or subcutaneous tissue. They account for only 3% of all soft tissue sarcomas and are subdivided in two subtypes depending on their origin and location2. Generally, superficial leiomyosarcomas occur as a solitary, slowly-enlarging lesion most commonly on the extensor surface of the proximal extremities, which coincide with the hair bearing areas. We report a case of superficial cutaneous leiomyosarcoma which occurs on the right temporal area of the face and gets abruptly larger to 2~3 cm in diameter within 3 months.
A 73-year-old Korean woman presented with a painless nodule on the right temporal area of the face. Before she fell down on the street and acquired an abrasion wound on the right temporal area of her face, she and her family members demonstrated that she had unremarkable skin findings. Then, a nodule grew larger very rapidly within 3 months. She had been treated with a wound dressing in local clinics, but it had been worsening continuously.
Her past history demonstrated that she had hypertension, diabetes, and iatrogenic Cushing's syndrome. Physical examination revealed a 2×3 cm, well-demarcated, soft erythematous nodule with central ulceration and bleeding (Fig. 1), and was otherwise unremarkable. Routine laboratory evaluations, including complete blood count, blood chemistry and urinalysis, showed normal findings. Also, chest X-ray and electrocardiography were within normal limits, too.
Squamous cell carcinoma was suspected clinically and biopsy was done. Histopathologic examination showed a lesion predominantly located in the dermis and interlacing fascicles of spindle-shaped cells with varying degrees of intermingled collagen. Spindle cells had elongated blunt-ended nuclei with mitotic figures and pleomorphic hyperchromatic nuclei (Fig. 2). Immunohistochemically, the cells were positive for actin, vimentin and desmin, while CD-34, epithelial membrane antigen, cytokeratin (CK), Factor VIII, and S-100 were negative (Fig. 3). On positron emission tomography-computed tomography scanning, there were no specific signs of internal source and metastasis to other sites, except for a hypermetabolic image on the right temporal lesion (Fig. 4). Based on the above findings, she was diagnosed with superficial leiomyosarcoma of the cutaneous type.
The lesion was removed by wide surgical excision, and a full-thickness skin graft was performed. There has not been any clinical recurrence for 6 months after the operation.
Superficial leiomyosarcomas have two subdivisions, cutaneous and subcutaneous forms due to their different original, clinical and prognostic implications1. The lesions usually occur on the legs (50~75%)2, and well-known predisposing factors are precursor leiomyomas, trauma, radiation, chemicals and sunlight3,4. Cutaneous leimyosarcoma originates from the arrector pili muscles or genital dartoric muscles, and presents as small, single or several intradermal nodules3,5. Sometimes it shows ulceration due to fixation to the epidermis. Subcutaneous leiomyosarcoma originates from the blood vessels of smooth muscles and presents as a larger movable mass in the subcutis without epidermal change. Overlying skin discoloration occurs more frequently in the cutaneous leiomyosarcoma than in the subcutaneous leiomyosarcoma6. In both types, spontaneous pain or tenderness was reported. Besides, other common symptoms such as pruritus, bleeding, and a burning sensation were noted1. Cutaneous leiomyosarcomas grow slowly and have a better prognosis than subcutaneous leiomyosarcomas. The metastatic potential is 5 to 10 percent for the cutaneous form compared with 30 to 60 percent for the subcutaneous form6. Our case occurred on the face (1~5%)6, and although we could not find the exact cause, trauma was thought to be a possible factor. Furthermore, the lesion increased suddenly in size within 3 months, so we think that our case differs from a typical superficial leiomyosarcoma.
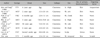
Histologically, the tumor is composed of interlacing fascicles of elongated spindle-shaped cells with eosinophilic cytoplasm and blunt-tipped nuclei, which have hyperchromatic pleomorphic bizarre cells and mitoses including atypical forms in the vast majority of cases. The less differentiated areas show more pleomorphic nuclei and atypical giant cells. In cutaneous leiomyosarcoma, these changes are localized in the dermis and may extend into subcutaneous tissue, but in subcutaneous leiomyosarcoma, they are localized predominantly in the subcutaneous tissues1. Histological findings may lead to confusion with other cutaneous spindle cell tumors. The differential diagnosis of histology includes atypical fibroxanthoma, dermatofibrosarcoma protuberans, angiosarcoma and spindle cell squamous cell carcinoma (Table 1)5,7. Superficial leiomyosarcoma expresses vimentin and smooth muscle actin in 100% of cases; however, desmin expression is seen in only about 60% of cases. CK and S-100 stains may sparsely be positive. Smooth muscle actin and desmin may assist in differentiating leiomyosarcoma from atypical fibroxanthoma and dermatofibrosarcoma protuberans which stain negatively with them. Additionally, CK and S-100 stains may be helpful in differentiating leiomyosarcoma from other spindle cell neoplasms as squamous cell carcinoma and malignant melanoma8.
Treatment of superficial leiomyosarcomas consists mainly of wide local excision including a 2~5 cm excision margin with a depth including the subcutaneous tissue9. Chemotherapy may only be considered for preoperative tumor volume reduction, but is not therapeutic. Moreover, radiotherapy is contraindicated due to the causative factor itself9. Recently, Mohs micrographic surgery has been utilized for the removal of various sarcomas, especially superficial leiomyosarcoma1.
Superficial leiomyosarcomas are usually characterized as slow growing. Actually, Fields and Helwig10 suggested that the median duration from onset to diagnosis was 2 years in 47 cutaneous leiomyosarcomas. In the Korean dermatologic literature, 7 cases of superficial cutaneous leiomyosarcomas have been reported. Duration until the time of diagnosis after occurring of the lesion is 2.5 years on average, so it was similar to the period reported by Fields and Helwig10. In all cases, only one case occured in the face, and cases which had possible triggering factors were just one (Table 2)11-17. But, in our case superficial leiomyosarcoma was located on the right temporal area of the face, and the duration of development after trauma is very short, about 3 months. Furthermore, this is the first report that is recognized following trauma. So, we believe our case showing the rapid growth of superficial leiomyosarcoma of the face is very rare.
In conclusion, if a tumor of similar aspect occurs from the head and neck, we will consider the possibility of the leiomyosarcomas and a careful approach is thought to be necessary.
Figures and Tables
Fig. 1
Solitary 2×3 cm, well-demarcated, soft erythematous nodule with ulceration and bleeding on right temporal area of face.

Fig. 2
Histopathologic findings of the lesion revealed interlacing fascicles of spindle-shaped cells with varying degrees of intermingled collagen. Spindle cells had elongated blunt-ended nuclei with mitosis and hyperchromatic nuclei (H&E stain; A: ×100, B: ×200).

Fig. 3
Results of immunohistochemical staining showed a positive reaction of actin (A), vimentin (B), and desmin (C), and a negative reaction of CD-34 (D), epithelial membrane antigen (EMA) (E), cytokeratin (F), factor VIII (G), and S-100 (H) (A~H: ×100).

Fig. 4
Positron emission tomography-computed tomography showed a hypermetabolic lesion (arrow) on the right temporal area of the head.
ACKNOWLEDGMENT
This study was supported by research fund and laboratory equipments from Chosun University in 2012.
References
1. Holst VA, Junkins-Hopkins JM, Elenitsas R. Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol. 2002. 46:477–490.

2. Torres T, Oliveira A, Sanches M, Selores M. Superficial cutaneous leiomyosarcoma of the face: report of three cases. J Dermatol. 2011. 38:373–376.

3. De Giorgi V, Sestini S, Massi D, Papi F, Alfaioli B, Lotti T. Superficial cutaneous leiomyosarcoma: a rare, misleading tumor. Am J Clin Dermatol. 2008. 9:185–187.
5. Blaise G, Nikkels AF, Quatresooz P, Hermanns-Lê T, Piérard GE. Childhood cutaneous leiomyosarcoma. Pediatr Dermatol. 2009. 26:477–479.

6. Choy C, Cooper A, Kossard S. Primary cutaneous diffuse leiomyosarcoma with desmoplasia. Australas J Dermatol. 2006. 47:291–295.

7. Elder DE, Elenitsas R, Johnson BL Jr, Murphy GF, Xu G. Lever's histopathology of the skin. 2009. 10th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Cop..
8. Annest NM, Grekin SJ, Stone MS, Messingham MJ. Cutaneous leiomyosarcoma: a tumor of the head and neck. Dermatol Surg. 2007. 33:628–633.

9. Tsutsumida A, Yoshida T, Yamamoto Y, Itoh T, Minakawa H, Sugihara T. Management of superficial leiomyosarcoma: a retrospective study of 10 cases. Plast Reconstr Surg. 2005. 116:8–12.

10. Fields JP, Helwig EB. Leiomyosarcoma of the skin and subcutaneous tissue. Cancer. 1981. 47:156–169.

11. Kim DY, Song JY. A case of primary cutaneous leiomyosarcoma. Korean J Dermatol. 1984. 22:445–448.
12. Na GY, Sung GY, Jun JB, Suh SB. A case of primary cutaneous leiomyosarcoma. Korean J Dermatol. 1988. 26:106–109.
13. Park HS, Kim SJ, Choi JC, Chun DK, Lee YS. A case of cutaneous leiomyosarcoma on the face. Korean J Dermatol. 2003. 41:1111–1113.
14. Rho JH, Choi HB, Joh OJ, Park SR, Song KY. A case of cutaneous leiomyosarcoma. Korean J Dermatol. 2005. 43:121–123.
15. Chun SH, Jeon SY, Lee WS. A case of cutaneous leiomyosarcoma on the sole. Korean J Dermatol. 2005. 43:707–709.
16. Park KY, Han TY, Seo SJ, Hong CK, Song KY. A case of dermal type of cutaneous leiomyosarcoma. Korean J Dermatol. 2007. 45:938–941.
17. Lee HE, Jue MS, Ko JY, Kim YH, Ro YS. A case of uterine leiomyosarcoma metastasized to the skin: local recurrence and rapid growth after excision. Korean J Dermatol. 2010. 48:346–349.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download