Abstract
Morsicatio labiorum is a form of tissue alteration caused by self-induced injury, mostly occurring on the lips, and is considered to be a rarely encountered mucocutaneous disorder. Clinically, it is a macerated grey-white patch and plaque of the mucosa caused by external stimuli (self-induced injury) such as habitual biting, chewing, or sucking of the lip. It is often confused with other dermatological disorders involving the oral mucosa, which can lead to a misdiagnosis. We herein report three cases of morsicatio labiorum; two cases were misdiagnosed as exfoliative cheilitis at the time of the first visit.
'Morsicatio' represents changes of surface features of the tongue, buccal mucosa, or lips caused by chronic tissue irritation, such as biting or sucking1,2. When this change occurs on the lips, it is called 'morsicatio labiorum'2. It is a self-induced injury caused by habitual behaviors, which may be associated with stress or mental illness in some patients1-3. Most information regarding morsicatio labiorum can be found in the dental literature; it has been rarely reported in the dermatology literature1. It can be misdiagnosed when missing a prudent history taking. We herein report three cases of this condition, with emphasis on habit-related histories such as self-mutilation.
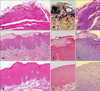
The first case was a 22-year-old female who presented with yellow plaques on the lips that had appeared 4 years prior to the current visit (Fig. 1A). She had tried to manage her lip problem with topical corticosteroids but there was no improvement. We found that the patient habitually stimulated her lips with her teeth, and sucked her lips. There were no associated medical or dental problems. We performed KOH examinations, which were also negative. The biopsy specimen revealed that the epidermis had a focal hyperkeratosis with basophilic debris on the surface (Fig. 2A). The gram stain showed many gram-positive cocci at the surface (Fig. 2B). The periodic acid-Schiff (PAS) stain were negative for fungal infection (Fig. 2C). Since the patient could not stimulate her lips any more because of pain at the biopsy site, the plaque lesions almost disappeared. The patient then recognized that her habitual behavior caused the lesion, and tried to refrain from lip stimulation. The lesions completely disappeared and there were no episodes of recurrence at one month of follow-up (Fig. 1B).
The second case was a 21-year-old male patient who presented with yellowish plaques on the lips that had appeared 7 years earlier (Fig. 1C). The patient had been treated with topical steroids with no response. The patient recognized that he chewed and sucked his lips habitually. The patient did not have any associated diseases or episodes of trauma. We performed KOH examinations, which were also negative. The biopsy specimen showed a marked acanthosis of the mucosal epithelium with surface exfoliation. In some areas, swollen epithelium was also seen (Fig. 2D). On the gram stain, bacterial colonies were not seen (Fig. 2E). The PAS stain was negative for fungal infection (Fig. 2F). After the skin biopsy, we advised the patient to refrain from habitual licking, and the lesions nearly disappeared after three months (Fig. 1D).
The third case was a 17-year-old healthy male who presented with a whitish surfaced plaque on the lower lip that had appeared 3 months earlier (Fig. 1E). KOH examinations were negative. The patient recognized that he habitually stimulated his lower lip with his teeth. The biopsy specimen showed marked acanthosis of the mucosal epithelium, and an underlying retention cyst was found in the interstitium (Fig. 2G). A gram stain was negative (Fig. 2H). The PAS stain was negative for fungal infection (Fig. 2I). We diagnosed this lesion as a 'morsicatio labiorum' with underlying mucocele. We removed the cystic lesion and advised the patient to cease his habitual licking. One month later, the lesion had almost completely disappeared (Fig. 1F).
Morsicatio is a condition caused by chronic physical irritation such as continuous biting of the tongue (morsicatio linguarum), buccal mucosa (morsicatio buccarum) or labial mucosa (morsicatio labiorum)1,2. Studies have reported that the tongue was the most common site affected; buccal and labial mucosal involvement were low in frequency4. It is much more common in individuals who are tense or anxious and who may also show bruxism, mandibular pain dysfunction, or other oral features of psychological disorders3,4. In these three cases, they all had habitually stimulated their lips with their teeth.
Clinically, morsicatio labiorum is characterized by a macerated, grey-white lesion of the mucosa where bacterial colonization may or may not be detected1. The condition shows bilateral shaggy white lesions of the anterior buccal mucosa that approximate the area where the upper and lower teeth meet5. The white areas are ragged and shredded. However, foci of erythema, erosion, or traumatic ulceration can occasionally be identified5.
Microscopic evaluation reveals marked acanthosis of the mucosal epithelium with an irregular surface, which demonstrates a ragged morphology. Basophilic debris accumulates on the surface and bacteria colonization is usually, but not inevitably, present4. It is thought that the surface irregularity of the oral mucosa may precede the onset of biting habits, and patients feel compelled to remove the lesion by manipulation1,6. The stratum spinosum may show markedly swollen keratinocytes that contain much glycogen1. Mild chronic inflammatory infiltration can be seen in the stroma and occasionally reactive atypia are present if there is ulceration or inflammation6. Because these findings are not that pathognomonic, biopsy specimens had been previously misinterpreted as non-specific chronic inflammation of the oral mucosa1,5.
The differential diagnosis of morsicatio should include other mucosal pathologies of the oral cavity that appear whitish or yellowish, such as oral lichen planus, candidiasis, leukoplakia, leukoedema, white sponge nevus, and chemical burn2,7. Some helpful clinical features that distinguish this from other whitish lesions are a rough, shaggy, often peeling surface. In addition, morsicatio is usually bilateral and located on movable, nonkeratinized mucosa that can be reached by the teeth4. Although proliferative leukoplakia may be bilateral and sometimes even symmetric, they will often involve areas that cannot be reached by the teeth (such as the gingiva)4. If the clinician is not absolutely certain that a white lesion is a morsicatio, a biopsy is always warranted1,4.
In conclusion, well-demarcated borders of the lesion of the mucosa, and the recognition of relevant habits of each patient are considered to be important in making a diagnosis and the differential diagnosis. Accurate diagnosis with history taking and educational modification of the patient's habitual actions are essential in the treatment of morsicatio, and this should be included in the differential diagnosis for hyperkeratotic lesion within the lips and mouth.
Figures and Tables
Fig. 1
(A, C) Localized yellow hyperkeratotic plaques on the upper and lower lips in patients 1 & 2. (E) A well-demarcated, white, smooth plaque on the lower lip in patient 3. (B, D, F) The lesions had completely disappeared after the patients retained from their lesion causing habits.

Fig. 2
(A) Histopathologic examination of the underneath mucosal surface of the plaque showed focal hyperkeratosis with basophilic debris on the surface (H&E, ×100). (B) Gram positive (purple-colored) bacterial colonies were found (Gram stain, ×100). (C) The specimen was negative for fungal infection (PAS stain, ×400). (D) The epidermis showed marked acanthosis and necrotic keratinocytes. Beneath the surface, swollen keratinocytes were seen (H&E, ×100). (E) Bacteria colonization was not observed (Gram stain, ×100). (F) The specimen was negative for fungal infection (PAS stain, ×400). (G) The epidermis showed marked acanthosis; however, bacteria colonization was not seen (H&E, ×100). (H) A gram stain was negative (Gram stain, ×100). (I) The specimen was negative for fungal infection (PAS stain, ×400).
References
1. Glass LF, Maize JC. Morsicatio buccarum et labiorum (excessive cheek and lip biting). Am J Dermatopathol. 1991. 13:271–274.

2. Tomás Carmona I, Cameselle Tejeiro J, Diz Dios P, Seoane Lestón J, Castro Ferreiro M, Limeres Posses J. Morsicatio linguarum versus oral hairy leukoplakia. Dermatology. 2000. 201:281–282.

3. Scully C, Hegarty A. Burns T, Breathnach S, Cox N, Griffiths C, editors. The oral cavity and lips. Rook's textbook of dermatology. 2010. 8th ed. Massachusetts: Blackwell;69.87–69.88.

4. Woo SB, Lin D. Morsicatio mucosae oris--a chronic oral frictional keratosis, not a leukoplakia. J Oral Maxillofac Surg. 2009. 67:140–146.

5. Allen AM, Camisa C. Callen JP, Horn TD, Mancini AJ, Salasche SJ, Schaffer JV, Schwarz T, editors. Oral disease. Dermatology. 2008. 2nd ed. Spain: Mosby Elsevier;1044.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download