Abstract
Background
Striae distensae are atrophic dermal scars with overlying epidermal atrophy causing significant cosmetic concern. Although a variety of laser and light sources have been used for the treatment of striae distensae, to date no definite 'gold standard' treatment modality has been determined.
Objective
To assess and compare the efficacy and safety of nonablative fractional photothermolysis and ablative CO2 fractional laser resurfacing in the treatment of striae distensae.
Methods
Twenty-four ethnic South Korean patients with varying degrees of atrophic striae alba in the abdomen were enrolled in a randomized blind split study. The patients were treated with 1,550 nm fractional Er:Glass laser and ablative fractional CO2 laser resurfacing. Each half of the abdominal lesion was randomly selected and treated three times at intervals of 4-weeks using the same parameters. Digital photography was conducted and skin elasticity and the width of the widest striae in each subject were measured at the baseline and 4 weeks after the final treatment. Clinical improvement was assessed by comparing pre- and post-treatment clinical photographs by two blinded physicians and participant satisfaction rates were evaluated. Skin biopsies were taken from three participants. All adverse effects were reported during the study.
Striae distensae, or so called 'stretch marks', are atrophic linear dermal scars with overlying epidermal atrophy1,2. They usually occur frequently in numerous physiological and pathological conditions such as adolescent growth spurts, pregnancy, obesity, Cushing's and Marfan syndromes, and long-term systemic or topical steroid use1. Especially in association with pregnancy, they are referred to as striae gravidarum. They have been noted to occur in more than 70% of pregnant women and are commonly found on the abdomen and breasts2. Although they do not cause any significant medical problems, aesthetically they can be a cause of great concern or psychological stress for many women. There is much controversy over their pathophysiology1. Besides hereditary factors, corticosteroids and mechanical stretching of the skin are presumed contributory factors in the development of striae distensae1.
A variety of treatment modalities have been attempted for striae distensae, but to date no definite 'gold standard' treatment modality has been determined. Topical therapy-with tretinoin or glycolic acid have yielded variable results, although these treatments work poorly if at all on mature striae (striae alba)3,4. Laser therapy has been advocated as a treatment option for striae distensae5-19, including the following types: flash-pumped 585-nm pulse dye laser, intense pulsed light, 308-nm excimer laser, nonablative 1,450-nm diode laser, radiofrequency device, 1,064-nm Nd:YAG laser, nonablative fractional photothermolysis, and ablative fractional CO2 resurfacing. Recent studies have suggested that nonablative fractional photothermolysis and ablative fractional CO2 resurfacing are the two most promising laser modalities for striae distensae in Asian skin15-19. However, a study comparing the clinical efficacy of the ablative vs. nonablative fractional photothermolysis system for the treatment of striae distensae has not been conducted.
The purpose of our study was to evaluate and compare the clinical efficacy and safety of nonablative fractional laser (NAFL) and ablative CO2 fractional laser (CO2FL) methods in the treatment of striae distensae in Asian skin.
Twenty-four ethnic South Korean female volunteers (Fitzpatrick skin types IV) aged between 30 and 48 with varying degrees of atrophic striae alba, developed on the abdomen after pregnancy, were enrolled in the study at the Department of Dermatology, Kangbuk Samsung Hospital between September 2010 and June 2011. Exclusion criteria were the history of keloid scarring or connective tissue disease, vitamin A derivatives use within 2 months of study initiation, any treatment procedure for striae distensae including any type of laser modality within 1 year of study initiation, pregnancy, use of immunosuppressive drugs, and any other diseases which can affect the wound-healing process. The protocol and informed consent were approved by the Kangbuk Samsung Hospital Institutional Review Board. This study was designed as a single-center, prospective, double-blind, randomized comparative split-scar trial.
Prior to laser procedure, a topical anesthetic cream (Encain® [mixture of lidocaine and prilocaine], Kolma Korea Co., Ltd, Seoul, Korea) was applied under an occlusive dressing for 60 minutes and subsequently washed off. The striae treatment areas were divided in half using the patients' umbilicus as the midline on the abdomen. On a randomly selected half side of the abdomen skin lesion, the patients were treated with 1,550 nm fractional Er:Glass laser (Mosaic, Lutronic Co., Ltd, Seoul, Korea) at a pulse energy of 50 mJ and a spot density of 100 spots/cm2, using a scan area of 5×10 mm in a static mode with one pass administered per treatment site without overlapping. The other half side was treated with ablative fractional CO2 laser resurfacing (eCO2, Lutronic Co., Ltd, Seoul, Korea) at a pulse energy of 40~50 mJ and a spot density of 75~100 spots/cm2, using a scan area of 8×8 mm in a static mode. Because no definite laser parameters have been established for striae distensae, suitable parameters for the study were determined based on comparison of results of preliminary experiments using various parameters, such as high energy with low density or low energy with high density (data not shown). The patients received three laser treatments at 4-week intervals using the same parameters.
High resolution digital photographs were taken using identical camera settings (Canon, Tokyo, Japan) at the baseline and 4 weeks after the final treatment. The width of the widest striae in each subject was measured at the baseline and 4 weeks after the final treatment. Skin elasticity was determined with a non-invasive, in vivo suction skin elasticity meter (Aramo TS™, Aram Huvis Co., Ltd, Gyeonggi, Korea) using a 6-mm measuring probe. The difference of the width and skin elasticity was converted into the percentage of reduction from the baseline. Clinical improvement was evaluated by two blind-study physicians by comparing photographs. The criteria for evaluations using a quartile grading scale were as follows; 0=no improvement, 1=mild (percent improvement, <25%), 2=moderate (percent improvement, 26~50%), 3=good (percent improvement, 51~75%), 4=excellent (percent improvement, >76%). In addition, a patient satisfaction score was rated using the following scale; 0=not satisfied, 1=slightly satisfied, 2=satisfied, 3=very satisfied, 4= extremely satisfied. 4-mm punch biopsy skin samples were taken from the most atrophic site before treatment and 4 weeks after the final laser treatment. The excised skin was fixed in 10% formalin and embedded in paraffin. Three micrometer-thick sections were stained with hematoxylin and eosin (H&E), Miller's elastic stains, and Masson trichrome stains. Two dermatologists masked at the time of sampling evaluated the histopathologic results. The epidermal thicknesses of the biopsy specimens were measured using an optic micrometer. All adverse effects were checked during the study.
All statistical analyses were carried out using IBM SPSS Statistics 19.0 (IBM, Armonk, New York, USA). The difference of skin elasticity and the width of the widest striae after laser treatment were analyzed by the repeated measures ANOVA test. The significances of the changes in skin elasticity and the width of the widest striae among the different laser modalities were determined using a paired t-test. The difference of clinical improvement and patient satisfaction score among the different laser modalities was analyzed by Pearson Chi-square and Fisher's exact test. Data were expressed as mean±standard deviation and statistical significance was accepted for p-values less than 0.05.
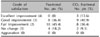
Of the 24 subjects initially enrolled, 22 completed the study. Two patients (8.3%) were excluded during treatment due to the occurrence of post-procedure pruritus and hyperpigmentation. The patients ranged in age from 30 to 48 years (mean 38.4 years). The cause of striae distense was pregnancy in all participants. No patient had a previous treatment history of striae distensae. The mean duration of the striae distensae was 11.4 years (range 5~23 years). Table 1 details the subject characteristics.
On an average, pre- and post-treatment skin elasticity varied from 59.05 to 69.55 and the width of the widest striae decreased from 7.00 to 4.55 in NAFL-treated sites (p <0.001). In CO2FL-treated sites, the average value of skin elasticity increased from 56.32 to 68.23 and the width of the widest striae was markedly reduced from 6.77 to 4.43 (p<0.001). These two objective parameters showed statistically significant differences between pre- and post-treatment states of both NAFL and CO2FL (p<0.001) (Table 2). To compare the therapeutic effects of the two laser modalities, we calculated the difference of skin elasticity and the width of the widest striae as percent value. In terms of skin elasticity, the CO2FL-treated sites (23.0±19.5) showed better improvement than the NAFL-treated sites (19.1±16.4) (p=0.377). The width of the widest striae was reduced more in the NAFL-treated sites (32.4±19.9) than in the CO2FL-treated sites (29.7±27.4) (p=0.486). However, there was no statistically significant difference between the two laser modalities.
In global photographs, 20 (90.9%) of the 22 patients were improved in the NAFL-treated sites. Among the 22 patients, 2 (9.1%) were good, 6 (27.3%) were fair, and 12 (54.5%) were poorly improved; however, 2 (9.1%) did not show any improvement after the treatment. Also, in CO2FL-treated sites, 20 (90.9%) of the 22 patients showed clinical improvement. Of the 22, 3 (13.6%) were good, 9 (40.9%) were fair, and 8 (36.4%) were poorly improved; however, 2 (9.1%) did not show any improvement after the treatment (Table 3). Considering all the patients who were assessed with excellent, good, and fair improvement, 12 patients (54.5%) in the CO2FL-treated sites demonstrated overall clinical improvement, which is greater than the 8 patients (36.4%) in the NAFL-treated sites. However, the difference between the two laser modalities was not statistically significant (p=0.226) (Fig. 1, 2).
Using the self-administered questionnaire, 18 (81.8%) patients judged their condition as improved and 4 (18.2%) as stabilized in the NAFL-treated sites. In the CO2FL-treated sites, 20 (90.9%) patients judged their condition as improved and 2 (9.1%) as stabilized. None of the patients considered their condition worsened (Table 4). Patient satisfaction surveys paralleled the clinical improvements. Considering all the rating scales of patients with excellent, good, and fair improvement, patients were more satisfied with CO2FL than with NAFL. However, the difference between the two laser modalities did not show statistical significance (p=0.664).
Pretreatment epidermal atrophy with flattening of the rete ridges and marked decrease of dermal collagen and elastic fibers were observed in all the cases. In the NAFL-treated sites, the average epidermal thickness was increased from 66.3 to 73.3 µm and the amount of collagen and elastic fibers were markedly increased after the laser treatment (Fig. 3). In the CO2FL-treated sites, the epidermal thickness was also increased on an average from 61.7 to 87.6 µm and the amount of collagen and elastic fibers were increased, compared to the pre-treatment state (Fig. 4).
The treatment was generally well tolerated. There was no significant long-lasting adverse effect except transient mild erythema and pigmentation. To evaluate the intensity of pain during the laser treatment, patients scored from 0 (no pain) to 10 (extremely intolerable pain). CO2FL treatment (average 6.41) was considered more painful than fractional laser treatment (average 3.41). Postinflammatory hyperpigmentation was noted in 8 patients (36.4%) in the NAFL-treated sites, and in 18 patients (81.8%) in the CO2FL-treated sites. Crusts remained longer in the CO2FL-treated sites (average 12 days) than in the NAFL-treated sites (average 3.5 days). Post-treatment erythema was noted for 6.43 days on an average after the CO2FL treatment, which was longer than that for the NAFL treatment (5.09 days). There was no incidence of hypopigmentation, blistering, ulceration, or worsening of striae distensae with either device.
Successful treatment of striae distensae has always been challenging. Although several treatment modalities have been proposed, no consistent modality is available. Besides the traditional topical therapies such as tretinoin, hydrant creams, glycolic acids and trichloroacetic acids, lasers have recently become a popular therapeutic alternative in the treatment of striae distensae5-19.
Fractional photothermolysis is a recently introduced laser treatment that creates numerous microscopic thermal injury zones of controlled width, depth, and density that are surrounded by a reservoir of spared epidermal and dermal tissue allowing for rapid repair of laser-induced thermal injury16. Considering that fractional photothermolysis showed effectiveness in the treatment of atrophic scars, few reports have described the use of fractional photothermolysis on the treatment of striae distensae15-17. Bak et al.17 revealed that a marked improvement of atrophic scar was owing to the increase of epidermal and dermal thickness and regeneration of dermal collagen after the fractional laser treatment. The U.S. Food and Drug Administration has recently approved the nonablative 1,540-nm erbium-droped glass fractional photothermolysis system (Lux 1540, Palomar Medical Technologies, Inc., Burlington, MA) for use in striae distensae.
Although a CO2 laser could theoretically stimulate fibroblast activity and improve the lesions through delicate abrasion of the skin, it was recommended that people with skin types IV to VI should avoid CO2 laser treatments for striae distensae in concern for the development of postinflammatory dyschromia after ablative laser therapy, especially for lesions in locations other than the face7. By incorporation of fractional technology into the conventional ablative CO2 lasers, more desirable clinical results could be expected. The efficacy of an ablative fractional laser system for the treatment of striae distensae has been demonstrated in recent retrospective and prospective studies18,19.
Our result showed that both NAFL and CO2 FL improve the clinical appearance of striae distensae remarkably over pretreatment states. Global assessment by physicians and scoring by participants showed better improvement in the CO2 FL-treated sites than in the NAFL-treated sites, but the difference was not statistically significant. To evaluate the efficiency of laser treatment objectively, we used a noninvasive, in vivo suction skin elasticity meter and measured the width of the widest striae. In both of the NAFL and CO2FL-treated sites, the changes of mean skin elasticity and mean width of the widest striae were statistically significant. Although the CO2FL-treated sites showed better improvement in skin elasticity and NAFL induced more reduction of the width of the widest striae, there was no statistically significant difference between the two devices. Previous clinical studies demonstrated that NAFL and CO2FL increase the amount of melanin pigment and transform the whitish bands into a natural skin color in striae alba15,18. Also in our study, almost all the striae alba bands showed marked changes of color. Along with the skin elasticity and textural changes, a more natural skin color tone created the marked clinical improvement. However, the small number of subjects (each group, n=3) might be a reason for the lack of difference between the two treatments.
This study, to our knowledge, is the first study comparing the clinical efficacy of the ablative vs nonablative fractional photothermolysis systems for the treatment of striae distensae. CO2 laser resurfacing may induce more dermal extracellular matrix remodeling than the nonablative laser treatment20,21, and CO2FL has been revealed to provide immediate tissue tightening and induce more collagen stimulation than nonablative fractional laser22. For these reasons, we assume that CO2FL might promise better clinical improvement of striae distensae. Although both physicians and patients evaluated that CO2FL induced a better clinical improvement, we failed to prove the statistically significant difference between the two devices. The risk of post-treatment hyperpigmentation of striae distensae in darker skinned patients is a major concern to dermatologists. Also, because of the poor wound healing, caution is required when treating the abdomen, buttock, or legs which are the preferential sites of stria distensa. In our study, the side effects of both treatments were limited to transient erythema, crust formation, and mild hyperpigmentation. Most of the hyperpigmentation improved spontaneously within 4 weeks. Although patients treated with CO2FL reported greater pain, a high incidence of hyperpigmentation and longer duration of post-treatment erythema and crust, this perception of greater pain and greater side effects did not appear to correlate with the laser preference and satisfaction levels. Even though there was no statistical difference, both the objective global assessment and the subjective patient satisfaction showed better clinical improvement with CO2FL than with NAFL. Further studies might be needed to establish the optimal parameter and treatment interval to enhance treatment efficacy, minimize the adverse events and to determine the better laser treatment modalities for striae distensae, especially in Asian skin. The smaller spot size and shorter dwelling time of ablative and NAFL treatment might minimize the side effects by deeper penetration depth and less thermal diffusion into the surrounding tissue23.
In conclusion, we suggest that both NAFL and CO2FL may be effective and safe treatment options for striae distensae of Asian skin, although it is difficult to distinguish which of the two laser modalities might be superior.
Figures and Tables
Fig. 1
Patient 5. Improvement in clinical appearance of striae distensae. Pre-treatment (A) and post-treatment (B) with a nonablative fractional laser treatment. Baseline (C) and post-treatment (D) with a CO2 fractional laser treatment.

Fig. 2
Patient 8. Improvement in clinical appearance of striae distensae. Pre-treatment (A) and post-treatment (B) with a nonablative fractional laser treatment. Baseline (C) and posttreatment (D) with a CO2 fractional laser treatment.

Fig. 3
Patient 13. Skin biopsies of untreated abdominal striae distensae (A, C, E) and the same site 1 month after three times of treatment with nonablative fractional laser (B, D, F), Note the increases in the epidermal thickness and the amount of collagen and elastic fibers after laser treatment. (A, B) H&E, ×200, (C, D) Masson trichrome stain, ×200, (E, F) Miller's elastic stain, ×200.

Fig. 4
Patient 13. Skin biopsies of untreated abdominal striae distensae (A, C, E) and the same site 1 month after three times of treatment with CO2 fractional laser (B, D, F), Note the increases in epidermal thickness and the amount of collagen and elastic fibers after the laser treatment. (A, B) H&E, ×200, (C, D) Masson trichrome stain, (E, F) ×200, Miller's elastic stain, ×200.

References
1. Cho S, Park ES, Lee DH, Li K, Chung JH. Clinical features and risk factors for striae distensae in Korean adolescents. J Eur Acad Dermatol Venereol. 2006. 20:1108–1113.

2. Atwal GS, Manku LK, Griffiths CE, Polson DW. Striae gravidarum in primiparae. Br J Dermatol. 2006. 155:965–969.

3. Kang S, Kim KJ, Griffiths CE, Wong TY, Talwar HS, Fisher GJ, et al. Topical tretinoin (retinoic acid) improves early stretch marks. Arch Dermatol. 1996. 132:519–526.

4. Ash K, Lord J, Zukowski M, McDaniel DH. Comparison of topical therapy for striae alba (20% glycolic acid/0.05% tretinoin versus 20% glycolic acid/10% L-ascorbic acid). Dermatol Surg. 1998. 24:849–856.

6. Elsaie ML, Baumann LS, Elsaaiee LT. Striae distensae (stretch marks) and different modalities of therapy: an update. Dermatol Surg. 2009. 35:563–573.
7. Nouri K, Romagosa R, Chartier T, Bowes L, Spencer JM. Comparison of the 585 nm pulse dye laser and the short pulsed CO2 laser in the treatment of striae distensae in skin types IV and VI. Dermatol Surg. 1999. 25:368–370.

8. Jiménez GP, Flores F, Berman B, Gunja-Smith Z. Treatment of striae rubra and striae alba with the 585-nm pulsed-dye laser. Dermatol Surg. 2003. 29:362–365.

9. Hernández-Pérez E, Colombo-Charrier E, Valencia-Ibiett E. Intense pulsed light in the treatment of striae distensae. Dermatol Surg. 2002. 28:1124–1130.

10. Alexiades-Armenakas MR, Bernstein LJ, Friedman PM, Geronemus RG. The safety and efficacy of the 308-nm excimer laser for pigment correction of hypopigmented scars and striae alba. Arch Dermatol. 2004. 140:955–960.

11. Tay YK, Kwok C, Tan E. Non-ablative 1,450-nm diode laser treatment of striae distensae. Lasers Surg Med. 2006. 38:196–199.

12. Suh DH, Chang KY, Son HC, Ryu JH, Lee SJ, Song KY. Radiofrequency and 585-nm pulsed dye laser treatment of striae distensae: a report of 37 Asian patients. Dermatol Surg. 2007. 33:29–34.

13. Goldman A, Rossato F, Prati C. Stretch marks: treatment using the 1,064-nm Nd:YAG laser. Dermatol Surg. 2008. 34:686–691.

14. Manuskiatti W, Boonthaweeyuwat E, Varothai S. Treatment of striae distensae with a TriPollar radiofrequency device: a pilot study. J Dermatolog Treat. 2009. 20:359–364.

15. Kim BJ, Lee DH, Kim MN, Song KY, Cho WI, Lee CK, et al. Fractional photothermolysis for the treatment of striae distensae in Asian skin. Am J Clin Dermatol. 2008. 9:33–37.

16. Katz TM, Goldberg LH, Friedman PM. Nonablative fractional photothermolysis for the treatment of striae rubra. Dermatol Surg. 2009. 35:1430–1433.

17. Bak H, Kim BJ, Lee WJ, Bang JS, Lee SY, Choi JH, et al. Treatment of striae distensae with fractional photothermolysis. Dermatol Surg. 2009. 35:1215–1220.

18. Lee SE, Kim JH, Lee SJ, Lee JE, Kang JM, Kim YK, et al. Treatment of striae distensae using an ablative 10,600-nm carbon dioxide fractional laser: a retrospective review of 27 participants. Dermatol Surg. 2010. 36:1683–1690.

19. Shin JU, Roh MR, Rah DK, Ae NK, Suh H, Chung KY. The effect of succinylated atelocollagen and ablative fractional resurfacing laser on striae distensae. J Dermatolog Treat. 2011. 22:113–121.

20. Fisher GJ, Varani J, Voorhees JJ. Looking older: fibroblast collapse and therapeutic implications. Arch Dermatol. 2008. 144:666–672.
21. Orringer JS, Voorhees JJ, Hamilton T, Hammerberg C, Kang S, Johnson TM, et al. Dermal matrix remodeling after nonablative laser therapy. J Am Acad Dermatol. 2005. 53:775–782.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download