Abstract
Childhood granulomatous periorificial dermatitis (CGPD), also known as facial Afro-Caribbean childhood eruption (FACE), is a distinctive granulomatous form of perioral dermatitis. It is a condition of unknown etiology, characterized by monomorphous, small, papular eruptions around the mouth, nose and eyes that histopathologically show a granulomatous pattern. It affects prepubescent children of both sexes and typically persists for several months but resolved without scarring. We report a 9 year-old girl with multiple, discrete, monomorphic, papular eruptions of 2-months duration on the perioral and periocular areas. Histopathological examination demonstrated upper dermal and perifollicular granulomatous infiltrate.
Childhood granulomatous periorificial dermatitis (CGPD) is a benign eruption of the face previously reported in prepubertal, Afro-Caribbean children. It was first described in 1970 in French published by Gianotti et al.1. It occurs most commonly in prepubertal children as an asymptomatic, discrete, 1~3 mm dome-shaped papule that is red or yellow-brown around the mouth, nose and eyes. Typically, the disease is benign and self-limited, therefore treatment is unnecessary. Differential diagnoses of CGPD include perioral dermatitis (PD), granulomatous-rosacea, sarcoidosis, and lupus miliaris disseminatus faciei (LMDF). Herein, we report a case of CGPD with a review of the literature.
A 9 year-old girl first presented to our department with a two-month history of non-pruritic papular eruption on her face. She had no personal or family history of skin disorders, including acne, atopy, contact allergies, or oily skin. She was not on oral medication and denied the use of topical steroids/irritants on her face. Physical examination revealed numerous monomorphic, small red-to-yellow-colored papules ranging from 1 to 3 mm in diameter, primarily located in the perioral area (Fig. 1A). A few papules were noted around the nose and both lower eyelids (Fig. 1B). Several dome-shaped papules on the lower eyelids were suspected to be syringoma or LMDF. Laboratory evaluation, including complete blood cell count, chemistry panel, calcium level, erythrocyte sedimentation rate (ESR), and serum levels of anti-nuclear antibody, showed no abnormalities.
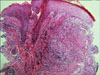
Biopsy was taken from a papule on the face. Granulomatous infiltrates were located around the hair follicles in the superficial dermis, comprised of epitheloid histiocytes and lymphocytes (Fig. 2). A small nodular granulomatous infiltrate containing many lymphocytes and a few epithelioid cells could also be seen in the mid to deep dermis. There was no caseation necrosis. Special stains for fungi and acid-fast bacilli revealed no microorganisms. These clinicopathological features were consistent with the diagnosis of CGPD. The patient did not receive treatment, but the papular eruptions resolved spontaneously over several months without therapy.
CGPD was first reported in 1970 in the French literature by Gianotti et al.1 He described five Italian children ranging in age from 2.5 to 7 years with distinctive eruption of the skin around the mouth. In 1974, Marten et al.2 reported 22 black children with papular eruption limited to the face. This eruption was described as flesh-colored papules grouped primarily on the central face. In 1989, Frieden et al.3 termed the disease as granulomatous PD in children. In 1990, Williams et al.4 reported 5 patients very similar to those of Marten et al. and Frieden et al. He coined the term facial Afro-Caribbean childhood eruption (FACE) to reflect that all their cases occurred in Afro-Caribbean children. Finally, in 1996, Knautz and Lesher5 used the term CGPD to differentiate the eruption from traditional PD and to avoid the term FACE which limits the diagnosis to Afro-Caribbean's subjects.
CGPD is thought to be an uncommon variant of perioral dermatitis. It typically affects prepubertal children and is more common in boys than girls6,7. In the Korean dermatologic literature, 3 cases in boys and 1 case in a girl were reported and the affected age of CGPD was known to be commonly between 3 and 126-9. According to the literature, CGPD is seen more commonly in dark-skinned patients, but several cases involving fair-skinned children have been reported10. Typical lesions have been described as flesh-colored, yellow-brown papules, not pustules or paulovesicles. The lack of pustules and the presence of discrete yellow-brown papules, less prominent erythema and scaling, and perifollicular granulomatous infiltrate on examination of a biopsy specimen can differentiate CGPD from perioral dermatitis5.
The etiology of this condition remains unknown. In some cases the eruption was related to allergens or irritants3. Other reports have implicated reactions to bubble gum, formaldehyde, cosmetic preparations, and antiseptic solutions11,12. Long-term use of topical steroids may induce or exacerbate CGPD3,13. In 2002, Urbatsch et al.14 reported a case of GPD as an unusual reaction to varicella vaccination.
Histopathologically, upper dermal and perifollicular granulomatous infiltrates are seen. Granulomatous infiltrates consist of epithelioid macrophages, lymphocytes, and giant cells. In some biopsy specimens, the infiltrate has been more diffuse, in others, well formed non-caseating granuloma are surrounded by lymphocytes. CGPD may also show epidermal change with mild to moderate spongiosis. The results of special stains and cultures are always negative for mycobacteria and fungus.
CGPD should be differentiated from sarcoidosis, granulomatous rosaea, and LMDF. Sarcoidosis differs clinically and histologically. Clinically, sarcoidosis is very rare in children and almost always associated with systemic involvement and symptoms such as fatigue, fever, cough, and dyspnea15. Histologically, sarcoidosis is characterized by "naked granulomas," without the inflammatory cells around and within the granulomas. Granulomatous rosacea usually involves the central third of the face and is characterized by erythema, telangiectasia, pustules, flushing, and edema16. It is most common in 30 to 50 year-old women17. LMDF is clinically characterized by chronic papular eruption occurring primarily in the central face. The lesions are usually red or yellow-brown dome-shaped papules with a predilection for the eyelid and are seen more commonly in the adult population. Histologic examination demonstrates well-formed granuloma with central caseation necrosis, but some exceptions have been reported, that in early LMDF lesions, they may not have central caseation18. However, LMDF is distinguished from CGPD by epithelioid cell granuloma with central caseation necrosis; the clinical course of LMDF resolves spontaneously with scarring.
The first step in therapeutic management should be discontinuation of all topical corticosteroids. Although CGPD is considered a self-limiting condition, treatment with tetracyclines, metronidazole, and erythromycin may be efficacious in CGPD. Most importantly, patients and parents should be reassured that CGPD is a benign, self-limited condition.
Figures and Tables
References
1. Gianotti F, Ermacora E, Bennelli MG, Caputo R. Particuliere dermatite peri-orale infantile. Observations sur 5 cas. Bull Soc Fr Dermatol Syphiligr. 1970. 77:341.
2. Marten RH, Presbury DG, Adamson JE, Cardell BS. An unusual papular and acneiform facial eruption in the negro child. Br J Dermatol. 1974. 91:435–438.

3. Frieden IJ, Prose NS, Fletcher V, Turner ML. Granulomatous perioral dermatitis in children. Arch Dermatol. 1989. 125:369–373.

4. Williams HC, Ashworth J, Pembroke AC, Breathnach SM. FACE-facial Afro-Caribbean childhood eruption. Clin Exp Dermatol. 1990. 15:163–166.

5. Knautz MA, Lesher JL Jr. Childhood granulomatous periorificial dermatitis. Pediatr Dermatol. 1996. 13:131–134.

6. Kim MS, Kim BS, Koh WS, Cho JJ, Chun DK. A case of childhood granulomatous perioral dermatitis. Korean J Dermatol. 2000. 38:526–529.
7. Lee WJ, Yang JH, Lee MW, Choi JH, Moon KC, Koh JK. A case of childhood granulomatous periorificial dermatitis. Korean J Dermatol. 2008. 46:1570–1572.
8. Kim JY, Park SY, Kim CW, Lee KS. A case of childhood granulomatous periorificial dermatitis. Korean J Dermatol. 2004. 42:1333–1336.
9. Choi JC, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. A case of childhood granulomatous perioral dermatitis. Ann Dermatol. 2001. 13:113–115.

10. Urbatsch AJ, Frieden I, Williams ML, Elewski BE, Mancini AJ, Paller AS. Extrafacial and generalized granulomatous periorificial dermatitis. Arch Dermatol. 2002. 138:1354–1358.

11. Georgouras K, Kocsard E. Micropapular sarcoidal facial eruption in a child: Gianotti-type perioral dermatitis. Acta Derm Venereol. 1978. 58:433–436.
13. Fisher AA. Sarcoid-like periocular dermatitis due to strong topical corticosteroids: prompt response to treatment with tetracycline. Cutis. 1987. 40:95–96.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download