Abstract
Actinic keratosis (AK) is a common, sun-induced, pre-malignant lesion with a strong likelihood of progressing to a malignancy. The reported risk of AK progressing to squamous cell carcinoma (SCC) varies from less than 1% to 20%. Clinically, induration, pain, large size, marked hyperkeratosis, ulceration, bleeding, rapid growth, and recurrence or persistence may be markers of AK progression into SCC. The risk of SCC metastasizing ranges between 0.5% and 3%. However, SCC of the lip arising from actinic cheilitis is more prone to metastasis than cutaneous SCC, with rates of the former varying between 3% and 20%. Here we report a typical case of SCC from actinic cheilitis with metastasis to the lymph nodes during a 4-year follow-up period. To exclude SCC, we emphasize the need for regular follow-up and prompt evaluation, including careful pathologic examination for actinic cheilitis.
Actinic cheilitis (AC) represents confluent actinic keratosis (AK) of the lip, most often involving the lower lip. It is a pre-malignant lesion with a strong likelihood of progressing to a malignancy. It is caused by prolonged exposure to ultraviolet (UV) radiation1.
Clinically, persistent pain, indurations, disease recurrence, and bleeding may be markers of progression to squamous cell carcinoma (SCC). Moreover, SCC of the lip has greater potential to metastasize than any other cutaneous SCC. Therefore, clinicians should promptly evaluate treat and follow-up SCC of the lip carefully if a patient presents with worrisome AC. We report a case of metastatic SCC arising from AC during the follow-up period.
A 66-year-old man presented at our clinic with a 5-month history of erythematous scaly erosive plaque on his lower lip that measured 1.0×1.5 cm (Fig. 1A) and was associated with a burning sensation. The patient did not have any notable medical, social or occupational history and denied habitual sun exposure and smoking. Biopsy of the lower lip showed infiltration of chronic inflammatory cells in the dermis, without any evidence of atypical keratinocytes in the epidermis (Fig. 2A). AC could not be ruled out at the time. A decision was made to treat this patient with liquid nitrogen cryosurgery, after which his skin lesion improved.
Thirty months later, this patient re-presented with a recurrent lesion on his lower lip (Fig. 1B), associated with dryness and a stinging sensation. His lesion was then re-evaluated and a biopsy was done on the recurrent lesion that revealed atypical, pleomorphic keratinocytes confined to the epidermis (Fig. 2B). A diagnosis of AC was made. He subsequently underwent tangential excision of the lesion for suspected SCC. Histological examination of the excised tissue confirmed extension of atypical keratinocytes beyond the basement membrane - a feature of SCC (Fig. 2C). After receiving a complete skin examination, this patient refused further evaluations.
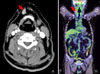
Six months later, the patient revisited our clinic with a right neck mass. A series of radiologic examinations including whole body computed tomography (CT) and positron emission tomography (PET)-CT were done (Fig. 3). The latter showed increased fluorine-18-fluorodeoxyglucose (18F-FDG) uptake in the right submandibular region. In addition, CT showed increased signal intensity in the same area, suggestive of lymph node metastasis or a new primary tumor. He was referred for excisional biopsy of the submandibular lymph node, which confirmed lymph node metastasis of the SCC (Fig. 2D). He is currently undergoing adjuvant radiation therapy and is being followed up on a regular basis.
AK is a precancerous lesion consisting of aberrant epidermal keratinocyte proliferation with the potential of progressing to SCC1. AC, a condition similar to AK, is usually confined to the vermilion zone of the lower lip. Important risk factors for AC are chronic sun-exposure, outdoor activity and skin type. The clinical features of classical AC include red, scaly, chapped lips associated with dryness, in addition to a burning or stinging sensation2.
SCC is the most common malignancy of the oral cavity and lips. It occurs in patients with a history of tobacco, or alcohol consumption. SCC of the lips usually presents as inflamed AC or leukoplakia. Therefore, any nonhealing, or recurrent AC warrants a biopsy. The reported risk for AK to progress onto SCC varies from less than 1% to 20%3,4. Clinically, persistent indurations, pain, ulceration, bleeding and recurrence may be markers of progression to SCC. Other factors include lifestyle risk factors and genetic predisposition. Moreover smoking and dietary habits associated with sunlight exposure might produce synergistic effects.
SCC arising from AK rarely metastasizes, with rates between 0.5% and 3%5. However, SCC of the lip is more prone to metastasis compared to cutaneous SCC, with rates varying between 3% and 20%6-8. Furthermore, the risk of metastatic spread to the cervical lymph nodes is higher than that of cutaneous SCC9. Generally, lymph node metastasis is detected 1 to 3 years after initial diagnosis and treatment.
In conclusion, patients with AC are at high risk of developing SCC and are prone to metastasis. This conclusion is for a classical case of AC transforming into SCC with lymph node metastasis. Our experience emphasizes the need to be vigilant when making a diagnosis of AK. It is a challenge to distinguish AK from SCC clinically. AC requires careful diagnosis and on-going follow-up to ensure detection of malignant changes and regional metastasis.
Figures and Tables
Fig. 1
Clinical presentation of our patient. (A) Initial visit, (B) 30 months later, (C) after excision.

Fig. 2
Histology of our patient. (A) Chronic inflammatory cell infiltration in the dermis without epidermal change at the initial visit. (B) Atypical, pleomorphic keratinocytes are confined to the epidermis 30 months later. (C) Extension of atypical keratinocytes in the tumor nest beyond the basement membrane after excision. (D) Suggestive squamous cell carcinoma in the lymph node (A, B, C, D: H&E, ×40, ×400).

Fig. 3
(A) A whole body computed tomography showing increased signal intensity in the right submandibular area. (B) The positron emission tomography-computed tomography image shows increased fluorine-18-fluorodeoxyglucose (18F-FDG) uptake in the same area, suggestive of lymph node metastasis (arrow).
References
1. Ducan KO, Geisse JK, Leffell DJ. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Epithelial precancerous lesions. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: Mc Graw Hill;1007–1027.
2. Markopoulos A, Albanidou-Farmaki E, Kayavis I. Actinic cheilitis: clinical and pathologic characteristics in 65 cases. Oral Dis. 2004. 10:212–216.

3. Cavalcante AS, Anbinder AL, Carvalho YR. Actinic cheilitis: clinical and histological features. J Oral Maxillofac Surg. 2008. 66:498–503.

4. Marks R, Rennie G, Selwood TS. Malignant transformation of solar keratoses to squamous cell carcinoma. Lancet. 1988. 1:795–797.

5. Abreu MA, Silva OM, Neto Pimentel DR, Hirata CH, Weckx LL, Alchorne MM, et al. Actinic cheilitis adjacent to squamous carcinoma of the lips as an indicator of prognosis. Braz J Otorhinolaryngol. 2006. 72:767–771.

7. Picascia DD, Robinson JK. Actinic cheilitis: a review of the etiology, differential diagnosis, and treatment. J Am Acad Dermatol. 1987. 17:255–264.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download