Abstract
Basaloid follicular hamartoma (BFH), uncommon rare benign neoplasm connected to the adnexal structures, presents with multiple clinical manifestations that can develop into basal cell carcinoma. BFH may be congenital or acquired, and the congenital form can be further divided into the generalized and unilateral type, and the acquired form may present as localized and solitary lesions. Congenital, generalized BFH is associated with systemic diseases such as alopecia, cystic fibrosis, hypohidrosis, and myasthenia gravis. In contrast, sporadic cases are observed as unilateral or localized lesions. BFH shows thick cords and thin strands of anastomosing basaloid proliferations that arise from hair follicles and are enclosed by loose fibrous stroma. Here, we report a 70-year-old man with an acquired, solitary form of BFH.
Basaloid follicular hamartoma (BFH) is an unusual, benign adnexal tumor composed of basaloid proliferating cells near hair follicules1,2. The variable clinical manifestations include one or more skin-colored papules, plaques, and nodules, predominantly on the face1,3. It may also appear at the distribution area of the terminal hair such as scalp, axilla, and pubic region4,5 with identical histologic findings. Histopathologically, there are multiple cords and thin strands of anastomosing basaloid or squamoid cells with numerous epidermal connections confined to the superficial papillary dermis1,3,4.
BFH is a very rare skin disease, with only 3 cases reported in the Korean literature. Herein, we report a case of BFH in a 70-year-old male presenting with a lesion located on the forehead, along with a review of literatures.
A 70-year-old-man presented with a 10 year history of a yellowish papule on the forehead. He had no subjective symptoms and no other medical history. The size of the lesion was invariable for the past 10 years. Physical examination revealed a 0.6×0.6 cm, ill-defined, flesh-colored firm papule with a central, pea-shaped depression on the left forehead (Fig. 1).
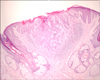
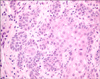
A skin biopsy specimen was taken from the lesion and stained with hematoxylin and eosin. Histopathologic examination demonstrated a clear demarcation between the tumor cells and surrounding tissues in the upper dermis. The lesion revealed strands and cords of small, basaloid cells emanating from the infundibular portion of the hair follicle (Fig. 2). The tumor stroma is mildly fibrocellular. There was no significant clefting between the tumor and stroma. No atypical cellular features or mitotic features were found (Fig. 3). The lesion was completely removed and no further relapse was observed.
BFH was first reported with a unilateral linear distribution in 1952 by Carvey6. In Korea, only 3 cases have been reported1,3,4. Han et al.4 reported an acquired, solitary form of BFH that was present as a single papule on the ala nasi, similar to our case. The others were acquired, solitary forms of BFH with combined basal cell epithelioma present as a single plaque on the tip of the nose3 and familial BFH syndrome that appeared as multiple hereditary form of BFH1. Our case showed a solitary, acquired form of BFH present as a single papule on the forehead without basal cell epithelioma.
BFH is classified as hereditary and acquired2,7. The hereditary form is divided into the generalized and unilateral nevoid type, and the latter form may present as localized and solitary lesions8. Dominantly inherited, generalized BFH syndrome is an autosomal dominant inherited type grouped with generalized, inherited BFH. It can present as small (1 to 2 mm), skin-colored, multiple lesions8. In particular, the familial generalized form of BFH is usually associated with systemic manifestations, including autoimmune diseases such as alopecia, myasthenia gravis; hypohidrosis; hypotrichosis; palmoplantar pitting; cystic fibrosis1,2,9. This type develops during early childhood. BFH is composed of strands and cords of small basaloid or squamoid cells originating from the infundibular portions of the hair follicles enclosed in a loose fibrous stroma8. BFH may have no atypical cellular features or mitotic activity, and there may not be a cleft between the tumor cells and surrounding stroma3-5,7.
The differential diagnosis of BFH includes basal cell carcinoma (BCC), generalized follicular hamartoma, basal cell nevus syndromes, trichoepitheliomas, fibrofolliculoma, and Cowden. Kaiser et al.10 reported a linear, solitary form of BFH that featured trichoblastomatous proliferations. Clinically, misdiagnosis of these conditions are BCC, sebaceous hyperplasia, seborrheic keratosis, and nevi of melanocyte2-4,11.
BFH and BCC are not related but may increase the risk for malignant transformation2. Thus, histological differentiation between infundibulocystic BCC and BFH is important. Both lesions may have anastomosing strands and cords of basaloid cells with numerous epidermal connections, an association with hair follicle structure, and no cleft between the tumor island and stroma2,4. However, the cleft between stromal cells and the mitotic activity of tumor cells is characteristic of infundibulocystic BCC4. Thus BFH should be discriminated from BCC depending on clinical, histological molecular features, and gene expression12.
Treatments of BFH include surgical excision, cryosurgery, laser surgery, and photodynamic therapy with particularly diffuse or extensive lesions13. Smith and Skelton9 reported that BFH associated with autoimmune disease may respond to retinoid therapy because it diminishes the hedgehog signaling pathways with decreased Gli-1 transcription activity. BFH may be malignant; thus, surgical excision is the first treatment choice despite risks of complications and post-scarring problems1,3,4.
We hereby report a case of BFH that sporadically developed on the forehead of an elderly man. It was an acquired, solitary form of BFH, not associated with basal cell epithelioma. Although BFH is a rare neoplasm, it is important to differentiate because of the malignancy risk of BCC and similar characteristics to other benign tumors. The accuracy of diagnosis and patient outcomes will improve with increasing awareness of this disorder.
Figures and Tables
Fig. 1
The skin lesion is solitary, skin colored, 0.6×0.6 cm, and smooth, with a central depressed papule on the left forehead.

References
1. Lee HJ, Lee WJ, Chang SE, Lee MW, Moon KC, Choi JH, et al. A case of familial basaloid follicular hamartoma syndrome. Korean J Dermatol. 2007. 45:1070–1073.
2. Patel AB, Harting MS, Smith-Zagone MJ, Hsu S. Familial basaloid follicular hamartoma: a report of one family. Dermatol Online J. 2008. 14:14.

3. Choi SW, Ryu YS, Kim HO, Kim CW. A case of basaloid follicular hamartoma combined with basal cell epithelioma. Korean J Dermatol. 1998. 36:148–151.
4. Han ES, Seo SJ, Hong CK, Song KY, Ro BI. A case of basaloid follicular hamartoma. Korean J Dermatol. 1997. 35:303–306.
5. Walsh N, Ackerman AB. Basaloid follicular hamartoma: solitary and multiple types. J Am Acad Dermatol. 1993. 29:125–129.

6. Carney RG. Linear unilateral basal-cell nevus with comedones; report of a case. AMA Arch Derm Syphilol. 1952. 65:471–476.
7. Brownstein MH. Basaloid follicular hamartoma: solitary and multiple types. J Am Acad Dermatol. 1992. 27:237–240.

8. El-Darouti MA, Marzouk SA, Abdel-Halim MR, Zidan AZ, Fawzy MM. Basaloid follicular hamartoma. Int J Dermatol. 2005. 44:361–365.

9. Smith KJ, Skelton H. Basaloid follicular hamartomas associated with autoimmune disease: a possible role for retinoids in therapy. J Am Acad Dermatol. 2003. 49:1067–1070.

10. Kaiser A, Spence RJ, Parwani A, Tihan T, Barrett TL. Basaloid follicular hamartoma with trichoblastomatous proliferations. J Cutan Med Surg. 2003. 7:395–398.

11. Nelson BR, Johnson TM, Waldinger T, Gillard M, Lowe L. Basaloid follicular hamartoma: a histologic diagnosis with diverse clinical presentations. Arch Dermatol. 1993. 129:915–917.

12. Jih DM, Shapiro M, James WD, Levin M, Gelfand J, Williams PT, et al. Familial basaloid follicular hamartoma: lesional characterization and review of the literature. Am J Dermatopathol. 2003. 25:130–137.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download