Abstract
Background
Urticaria and atopic dermatitis are representative allergic skin diseases that can be mediated by IgE. Measuring levels of specific IgE can be used to confirm causative agents of these skin diseases.
Objective
To analyze results from the multiple allergosorbent test chemiluminescent assay (MAST-CLA), which measures specific IgE in the presence of a causative agent/allergen, in IgE-mediated skin diseases.
Methods
A total of 404 patients with urticaria, atopic dermatitis or pruritus were enrolled in the present study. Positive rates of specific IgE as well as total serum IgE from the MAST-CLA were compared.
Results
Positive rates of specific IgE were highest in atopic dermatitis patients, followed by urticaria, and then pruritus, with 57.0%, 37.1%, and 20.8%, respectively (p<0.05). House dust mite species were the most common allergens in both atopic dermatitis and urticaria skin diseases. There were no differences in the overall MAST-CLA results between acute and chronic urticaria. The relative positive rate of inhalant allergen was significantly higher in adult than in child atopic dermatitis patients.
Conclusion
Results from the MAST-CLA showed diversity among the three disease groups, and within each disease group, with different positive rates of specific IgE, a different mean allergen number per patient, and so on. Therefore, we concluded that MAST-CLA could be a useful diagnostic tool for various allergic skin diseases.
With allergic diseases (or allergies), knowing the relationship to specific or potential allergens is important to determine the best therapeutic intervention and subsequent prevention. Diagnosing allergic diseases involves taking a detailed medical and personal history, a physical examination, and either in vivo or in vitro testing for relevant allergens. Although a skin prick test is the most widely used method and is considered the gold standard for determining specific antigen(s), it has several disadvantages, including a high percentage of false positives, antihistamine interference, and invasiveness. To circumvent these disadvantages, various in vitro analyses, including the radioallergosorbent test (RAST), Pharmacia CAP test (CAP), and the multiple allergosorbent test chemiluminescent assay (MAST-CLA) were developed. MAST-CLA is a simple method that can test for 35 common allergens simultaneously, and thus it is suitable as a screening test. Employing a very sensitive chemiluminescence technique, MAST-CLA is safer than other methods that use a radioactive isotope. Also, MAST-CLA was reported to have a relatively high sensitivity, specificity, and correlation rate when compared with the skin prick test in previous studies1-4.
Currently, MAST-CLA is one of the most popular tools used in the Republic of Korea to diagnose allergic skin diseases, including atopic dermatitis and acute/chronic urticaria. This laboratory test, measuring specific IgE, is helpful in confirming causative agents of these diseases. In the present study, we analyzed MAST-CLA results from patients, who had visited the Department of Dermatology at Boramae Hospital, and who were diagnosed with atopic dermatitis, urticaria and pruritus. We analyzed the results within each disease group according to different epidemiological factors. Furthermore, we compared the results among these three disease groups.
We reviewed results from the MAST-CLA that had been carried out between December 2005 and August 2007 at the Department of Dermatology, Boramae Hospital. The three most common diseases for which MAST-CLA was prescribed were urticaria, atopic dermatitis, and pruritus. A total of 404 patients, with these diseases, were enrolled. Positive rates of specific IgE from the MAST-CLA results were compared among the three disease groups.
Age, sex, major symptom, diagnosis, and disease duration were evaluated by reviewing patient's medical records retrospectively. Atopic dermatitis patients were divided into children or adults group. Reflecting the recent upward trend in the upper age limit of pediatric patients, we defined a child as a person younger than 18 years of age; this included neonates, infancy, adolescence, and puberty. Urticaria patients were divided into an acute or chronic group, by 6 weeks of disease duration - widely used in many references.
Patient blood samples were checked by using the Korean food panel of the MAST-CLA (MAST-Immunosystems, Mountain View, CA, USA). This assay can simultaneously measure 35 different specific IgE antibodies. Associated allergens consisted of those from food, mold, pollen, as well as inhalant allergens, all of which Korean people show a positive reaction most frequently. The test procedure was the method described in Kim et al.5. Class 2 or more was considered a positive reaction.
The statistical analysis was conducted with SPSS software (SPSS v. 15.0). Using the chi-square test, positive rates of specific IgE from the MAST-CLA were compared among the different groups. ANOVA was used to compare positive rates of each disease group for a specific allergen. p-values under 0.05 were considered to be statistically significant.
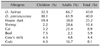
Table 1 summarizes the clinical characteristics of the 404 patient subjects, with a disease distribution of 245 urticaria, 135 atopic dermatitis, and 24 pruritus patients. Overall, subject ages ranged from 8 months to 76 years, with a mean of 31.37 years. In the urticaria group, the mean age was 37.45 years (1~55 years), with 109 males and 136 females. Mean disease duration was 13.22 months; 112 were diagnosed with acute, and 133 with chronic urticaria - persisting beyond 6 weeks. In the atopic dermatitis group, the mean age was 13.41 years (8 months~52 years); 93 were children under the age of 18 years, and 42 were adults. Of these, 71 were male, and 64 were female. Mean disease duration was 13.2 months (1 day~20 years).
Positive rates of specific IgE (number of patients who showed a positive reaction for one or more specific allergens out of the total number of patients) were significantly different among the three disease groups. In atopic dermatitis patients, 77 out of 135 showed a positive reaction with a positive rate of 57.0%. In urticaria patients, 91 of 245 showed a positive reaction with a positive rate of 37.1%. In pruritus patients, 5 of 24 showed a positive reaction with a positive rate of 20.8% (Fig. 1). The mean allergen number per patient, who showed a positive reaction, was highest at 4.0 in the atopic dermatitis group, followed by 3.3 in the urticaria group, and 2.4 in the pruritus group.
As mentioned above, the positive rate of specific IgE in atopic dermatitis was 57%. We analyzed this positive rate of specific IgE in atopic dermatitis patients according to different clinical characteristics and conditions.
A personal history (PHx) whether the patients had other atopic diseases was mentioned in 96 of a total 245 atopic patients. Among these 96 patients, 34 patients (35.4%) had other atopic diseases. Twenty-one patients (21.9%) had allergic rhinitis, 10 patients (10.4%) had urticaria, and 3 patients (3.1%) had asthma. Positive rate of specific IgE was significantly higher in PHx (+) patients at 65.2% than in PHx (-) patients at 49.4% (p<0.05).
Existence of family history (FHx) of atopic dermatitis was recorded in 54 patients. Among them, 22 patients (40.7%) had a FHx of atopic dermatitis. Positive rate of specific IgE was higher in the FHx (+) group at 68.5% than in the FHx (-) group at 52.5% (p<0.05).
In atopic dermatitis, we compared the results of children (age under 18 years) with adult patients. Positive rate of specific IgE in the adult group was higher than in the child group (64.3% vs. 52.7%), with a statistical significance (p<0.05). Mean allergen number per patient, of those who showed a positive reaction, was higher in the adult group than in the child group (6.7 vs. 2.3). Table 2 shows the number of positive specific IgE in adult and child atopic dermatitis patients.
Table 3 shows common allergens in atopic dermatitis. In general, the most common allergen in atopic dermatitis was Dermatophagoides farinae (D. farinae) (43.0%), followed by Dermatophagoides pteronyssinus (D. pteronyssinus) (40.0%) and house dust (25.2%). Shrimp (10.4%) and cat (8.9%) were next. The five most common allergens in adults were identical to those of total atopic dermatitis patients. In children, although the first, second, and third most common allergens were identical with total atopic dermatitis, the fourth was beef, and the fifth was cow's milk and crab. Among food allergens, the most common was shrimp (10.4%); the second, crab (8.1%); the third, baker's yeast (6.7%); the fourth, beef (5.9%); and the fifth, rice (5.2%).
Generally, a positive rate for inhalant allergens (48.9%) was higher than that for food allergens (29.6%). A positive rate for food allergens showed no significant difference between adults and children (28.0% vs. 33.3% respectively). However, a positive rate for aeroallergen was higher in adults (64.3%) than in children (41.9%), with p<0.05) (Fig. 2).
As mentioned above, a positive rate of specific IgE in urticaria was 37.1%. There was no statistically significant difference in positive rates of specific IgE between acute and chronic urticaria (38.3% vs. 34.2%). Mean allergen number per patient, of those who showed a positive reaction did not show any significant difference, either (data not shown).
The three most common allergens of urticaria were identical to those of atopic dermatitis, although the positive rates in urticaria patients were significantly lower than in atopic dermatitis patients. The first was D. farinae (25.9%), the second was D. pteronyssinus (22.4%), and the third, house dust (11.4%). Mugwort (5.7%) and cockroach mix (5.3%) followed after house dust. No allergen showed significantly different positive rates between acute and chronic urticaria.
Specific allergens that showed different positive rates between urticaria and atopic dermatitis were baker's yeast (p=0.000), beef (p=0.003), chicken (p=0.007), peanut (p=0.014), rice (p=0.022), tuna (p=0.014), house dust (p=0.000), D. farinae (p=0.000), D. pteronyssinus (p=0.000), cow's milk (p=0.019), shrimp (p=0.029), and alternaria (p=0.019). All values were higher in atopic dermatitis.
Five (20.8%), of a total of 24, pruritus patients were positive for one or more specific allergens. The most common allergens were house dust and Dermatophagoides, which each of three patients had a positive reaction. However, detailed analysis was not carried out in the pruritus group, because the number of patients, who showed a positive reaction for specific IgE, was too small.
There are several allergic skin diseases that can be mediated by IgE, and atopic dermatitis is one of them. It is a chronic recurrent skin disease that usually occurs in children. Although the precise etiology of atopic dermatitis has not been clarified, it is now widely accepted that serum IgE has a key role in pathogenesis. Another representative skin disease that can be mediated by IgE is urticaria. Urticaria is classified into immunologic and non-immunologic; in immunologic urticaria, IgE-mediated immune response is one of the main etiologic factors. Pruritus is defined as a sensation that leads to a desire to scratch. It is a predominant symptom for a varying number of skin diseases, but it may also be a diagnostic term when it is the only symptom in the absence of any specific skin lesion. There are numerous causes of pruritus. A type 1 immune reaction can be one cause, especially when a pruritic symptom appears several minutes to hours after exposure to a causative agent. Laboratory tests that measure specific IgE could be used to confirm causative agents.
In the present study, we measured specific IgE in urticaria, atopic dermatitis, and pruritus patients using MAST-CLA, and analyzed the results. A recent technique, the MAST-CLA technology is a simple, practical and safe approach for in vitro measurement in the diagnosis of allergic diseases. It can test simultaneously for 35 common allergens, found in any environment, using a fluorescent antigen-antibody reaction. We tried to analyze the MAST-CLA results within each of these three disease groups, and moreover, to compare the results among disease groups. Although there are several prior studies that analyzed specific IgE in atopic dermatitis using MAST-CLA3,5-7, few have worked with two or more diseases, or have compared the results among and within various diseases as in our study.
A positive rate of specific IgE was highest in atopic dermatitis (57.0%), followed by urticaria (37.1%) and pruritus (20.8%) - with statistical significance. A positive rate in atopic dermatitis and urticaria was in agreement with that of previous studies in Korea3,5. Mean allergen number per patient of those who showed a positive reaction was largest in atopic dermatitis (4.0), compared with urticaria (3.3) and pruritus (2.4). Mean allergen number in atopic dermatitis was similar to the results of a recent study in Korea5.
In atopic dermatitis patients, the positive rates were different according to the various epidemiological factors. Patients who had a personal or family history of other atopic diseases showed higher positive rates of specific IgE than patients who had no histories. This correlates with the well-known fact, patients who have a personal or family history of atopy show higher total and specific IgE6. Comparing results of child and adult atopic patients, positive rates of specific IgE were significantly higher in adults (64.3%) than in children (52.7%). This is in accordance with the previous report by Kim et al.5 in which positive rates of adult patients were significantly higher than that of children (71.2% vs. 45.6%). In other previous studies, there was an age-specific difference in positive rates, generally low in children under 10 years, high in the second and third decade of life, and decreasing after the fifth decade8,9. However, Tanei and Katsuoka10 reported that 14 of 16 senile atopic patients, with a mean age of 76.9 years, showed a high positive rate of 87.5% for antigen-specific IgE antibodies. Therefore, further evaluation for an age-specific positive rate of specific IgE in a larger population is needed. Although the positive rates between adults and children showed minimal difference in this study, mean allergen number per patient, of those who showed a positive reaction, was significantly higher in adults than in children (6.7 vs. 2.3).
With respect to common allergens of atopic dermatitis, the most prevalent was D. farinae, followed by D. pteronyssinus, and house dust, consecutively. This result is in accordance with previous studies3,5-7, although the precise positive rates showed some discrepancies in each study. This reconfirmed that the most common allergen in allergic skin diseases is the house dust mite; D. farinae and D. pteronyssinus are known to be main sources of house dust allergens11,12. These allergens are considered to be the most important causative allergens in allergic asthma and perennial rhinitis13,14, and they also might be an essential causative allergen in atopic dermatitis. Teplitsky et al.15 reported that atopic dermatitis patients showed a higher prevalence of mites, which could be involved in allergic sensitization and disease exacerbation, on their skin than did healthy individuals. Furthermore, repeated topical application of a crude extract of Dermatophagoides can induce atopic dermatitis-like skin lesions in NC/Nga mice16,17. Moreover, previous in vitro studies18,19 demonstrated that house dust mites induce inflammatory cytokines in human keratinocytes via enzyme activity or gene expression. The fourth most common allergen was shrimp, and the fifth, cat. Although the first through third most common allergens were identical in previous studies, the fourth and the fifth were variable. In atopic dermatitis, Lee et al.7 reported that the fourth most common allergen was cockroach mix, and the fifth, crab, whereas Kim et al.5 reported that oak, rye and Aspergillus followed after house dust allergens. The five most common allergens in adults were identical with that of total atopic dermatitis patients. However, in children, although the first, second, and third most common allergens were identical with total atopic dermatitis, the fourth was beef, and the fifth was cow's milk and crab. Among food allergens, the most common was shrimp, then crab, followed by baker's yeast, beef, and rice, consecutively. The proportion of aeroallergen to food allergen was higher in adults. Food allergy is a well-known aggravating factor for atopic dermatitis, especially in moderate to severe child atopic dermatitis patients20. However, similar to the present study, patients showed higher positive reactions to inhalant allergens rather than to food allergens as they aged in previous studies6,21. This is possibly due to the fact that most patients develop tolerance to some food allergens, whereas they get exposed to more new aeroallergens that can induce an allergic reaction over time. With respect to just food allergens, children showed relatively higher positive rates for milk and beef; on the other hand, adults showed relatively higher positive rates for shrimp and crab. These results are explained by the fact that milk and beef are foods to which one is frequently exposed in infancy, so that most develop tolerance; whereas, people are exposed to crustaceans, such as crab or shrimp, relatively later in life. Higher positive rates for crustacean allergens in adults might be also explained by the fact that the relative proportions of aeroallergen that cross-react with crustacean is higher in adults. It has been described that cockroach, shrimp and crab can cross react with house dust mites via the tropomyosin allergen22. Hence, we have to be cautious when analyzing the results among these kinds of allergens.
In urticaria, the first, second, and third most common allergens were identical with that of atopic dermatitis, while the fourth was mugwort, and the fifth was a cockroach mix. Likewise, in atopic dermatitis, the first through third most common allergens were identical in previous studies, but the fourth and the fifth were variable. The fourth most common allergen was shrimp in Miyamoto et al.11, whereas in Park et al.8, pollen, molds and cockroach were the fourth, fifth and sixth respectively. In our present study, mugwort in urticaria and cat in atopic dermatitis were especially common allergens, apart from house dust allergens, and those that can cross-react with them.
In our study, there was no significant difference in the positive rate of specific IgE between acute and chronic urticaria. There was no specific allergen that showed different positive rates between the two groups. These results indicate that given enough time, a high percentage of currently acute urticaria cases may become chronic. Additionally, arbitrary categorization of urticaria into acute or chronic, by a cutoff time of 6 weeks, could be meaningless, as the causes may be identical. Urticaria is commonly classified into acute and chronic disease on the basis of the disease duration of 6 weeks. Some foods, drugs, or infections are known to cause acute urticaria; whereas, with chronic urticaria, it is difficult to find an obvious cause, except in the case of physical urticaria. In Lee et al.3, using MAST-CLA, D. farinae was the most common (21.4%) allergen in chronic urticaria, followed by D. pteronyssinus (21.4%), house dust (7.1%) and shrimp (4.3%). This is consistent with the results of our present study, although positive rates of house dust and shrimp were higher in the current study. Similarly, Caliskaner et al.23 reported that the most common allergen of chronic urticaria was the house dust mite (24.7%) - by using a skin prick test. They also reported that house dust mites were the only allergen that had a significantly different positive rate between urticaria patients and healthy controls. Moreover, the positive rate in urticaria was lower than in atopic dermatitis, consistent in our study.
We measured and analyzed specific IgE for several allergic diseases using MAST-CLA. This study is meaningful, in that we not only analyzed results within each disease group, but we also compared across different and related IgE-mediated diseases. We compared disease groups by identical laboratory methods and conditions. Among the previous studies mentioned above, discrepancies in positive rates of specific IgE existed even though investigations involved the same disease. These discrepancies might be caused by a disparity in subject populations or different laboratory conditions. This present retrospective study provides a cross-sectional analysis among three different diseases. Therefore, our results may assist clinicians in understanding etiology and determining causative agents of particular diseases, which may share an underlying mechanism. However, further investigation is needed to elucidate to what degree these allergens induce clinical symptoms in related diseases.
Figures and Tables
Fig. 1
Positive rates of specific IgE in urticaria, atopic dermatitis, and pruritus (*p<0.05, †p<0.01).

References
1. Lee IW, Kim TH, Ahn SK, Choi EH. Comparison of MAST chemiluminescent assay(MAST-CLA) with skin prick, test in patients with atopic dermatitis. Korean J Dermatol. 1999. 37:297–304.
2. Scolozzi R, Boccafogli A, Vicentini L, Baraldi A, Bagni B. Correlation of MAST chemiluminescent assay (CLA) with RAST and skin prick tests for diagnosis of inhalant allergic disease. Ann Allergy. 1989. 62:193a–193b.
3. Lee YJ, Park CW, Lee CH. A study of patients with chronic urticaria using the chemiluminescent assay and prick test. Korean J Dermatol. 1995. 33:260–267.
4. Finnerty JP, Summerell S, Holgate ST. Relationship between skin-prick tests, the multiple allergosorbent test and symptoms of allergic disease. Clin Exp Allergy. 1989. 19:51–56.

5. Kim HD, Cho MK, Lee SY, Lee JS, Park YL, Whang KU, et al. Evaluation of the MAST CLA allergy system for measuring total and allergen specific IgE in child and adult atopic dermatitis. Korean J Dermatol. 2007. 45:413–421.
6. Lee EJ, Piao YJ, Kim KH, Suhr KB, Lee JH, Park JK. The relationship among the clinical evaluation, total IgE, and allergen-specific IgE of MAST-CLA in atopic dermatitis. Korean J Dermatol. 2003. 41:197–206.
7. Lee CS, Tang RB, Chung RL. The evaluation of allergens and allergic diseases in children. J Microbiol Immunol Infect. 2000. 33:227–232.
8. Park KI, Chun HS, Shin JW, Kim HS, Song KS. Allergen frequencies on MAST CLA by age groups using new Korean panel. J Clin Pathol Qual Control. 1999. 21:243–249.
9. Cho YW, Park HS, Oh SH, Hong CS. Immediate skin reactivity to 12 inhalant allergens in a general population of Korea. J Korean Med Assoc. 1987. 30:647–656.
10. Tanei R, Katsuoka K. Clinical analyses of atopic dermatitis in the aged. J Dermatol. 2008. 35:562–569.

11. Miyamoto T, Oshima S, Ishizaki T, Sato SH. Allergenic identity between the common floor mite (Dermatophagoides farinae Hughes, 1961) and house dust as a causative antigen in bronchial asthma. J Allergy. 1968. 42:14–28.

12. Voorhorst R, Spieksma FTM, Varekamp H, Leupen MJ, Lyklema AW. The house-dust mite (Dermatophagoides pteronyssinus) and the allergens it produces. Identity with the house-dust allergen. J Allergy. 1967. 39:325–339.

13. Tang RB, Tsai LC, Hung MW, Hwang B, Wu KG. Detection of house dust mite allergens and immunoblot analysis in asthmatic children. J Asthma. 1988. 25:83–88.

14. Tang RB, Chang HN, Lin FM, Chang YF, Chou NS, Lin CY. Serum IgE, skin and radioallergosorbent tests for house dust and mites in asthmatic children. J Asthma. 1986. 23:245–249.

15. Teplitsky V, Mumcuoglu KY, Babai I, Dalal I, Cohen R, Tanay A. House dust mites on skin, clothes, and bedding of atopic dermatitis patients. Int J Dermatol. 2008. 47:790–795.

16. Kang JS, Lee K, Han SB, Ahn JM, Lee H, Han MH, et al. Induction of atopic eczema/dermatitis syndrome-like skin lesions by repeated topical application of a crude extract of Dermatophagoides pteronyssinus in NC/Nga mice. Int Immunopharmacol. 2006. 6:1616–1622.

17. Oshio T, Sasaki Y, Funakoshi-Tago M, Aizu-Yokota E, Sonoda Y, Matsuoka H, et al. Dermatophagoides farinae extract induces severe atopic dermatitis in NC/Nga mice, which is effectively suppressed by the administration of tacrolimus ointment. Int Immunopharmacol. 2009. 9:403–411.

18. Kato T, Takai T, Fujimura T, Matsuoka H, Ogawa T, Murayama K, et al. Mite serine protease activates protease-activated receptor-2 and induces cytokine release in human keratinocytes. Allergy. 2009. 64:1366–1374.

19. Maeda S, Shibata S, Chimura N, Fukata T. House dust mite major allergen Der f 1 enhances proinflammatory cytokine and chemokine gene expression in a cell line of canine epidermal keratinocytes. Vet Immunol Immunopathol. 2009. 131:298–302.

20. Host A. Cow's milk protein allergy and intolerance in infancy. Some clinical, epidemiological and immunological aspects. Pediatr Allergy Immunol. 1994. 5:5 Suppl. 1–36.

21. Chang DS, Seo SJ, Hong CK. Patch test and specific IgE level with food antigens in atopic dermatitis patients. Korean J Dermatol. 2002. 40:1028–1034.
22. Purohit A, Shao J, Degreef JM, van Leeuwen A, van Ree R, Pauli G, et al. Role of tropomyosin as a cross-reacting allergen in sensitization to cockroach in patients from Martinique (French Caribbean island) with a respiratory allergy to mite and a food allergy to crab and shrimp. Eur Ann Allergy Clin Immunol. 2007. 39:85–88.
23. Caliskaner Z, Ozturk S, Turan M, Karaayvaz M. Skin test positivity to aeroallergens in the patients with chronic urticaria without allergic respiratory disease. J Investig Allergol Clin Immunol. 2004. 14:50–54.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download