Abstract
Sarcoidosis is an idiopathic multisystemic disorder with variable cutaneous presentations that are classified as specific or non-specific according to the presence of non-caseating granulomas on histologic examination. Specific manifestations can include papules, scar sarcoidosis, ulcers, or even alopecia. Herein, we present a case of cutaneous sarcoidosis that presented as multiple erythematous macules and patches on the trunk and extremities of a 32-year-old man. The clinical appearance was unlike any other form reported in the literature.
Sarcoidosis is a multisystem disorder of unknown etiology that most commonly affects the lungs, lymph nodes, liver, spleen, or skin1. Skin manifestations are present in approximately 20% to 35% of all patients2. Due to the varying morphologies that often mimic other skin and autoimmune disorders, the diagnosis is often not apparent. Depending upon the histologic examination results, the lesions are divided into specific or non-specific types1. We have encountered a case of cutaneous sarcoidosis presenting as multiple erythematous macules and patches, a form unlike any other reported in the literature.
A 32-year-old man presented with a 2-month history of multiple lesions on his arms and trunk. The lesions first began on a scratch wound on the left arm and began to spread during the past week. The patient denied any other symptoms and was otherwise in good health.
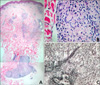
The dermatologic examination revealed multiple, asymptomatic, erythematous macules and patches on the trunk and extremities (Fig. 1). The lesions were relatively flat, showed minimal scaling, and ranged in size from 1~7 cm in diameter. There was no induration or atrophy upon palpation. A 3 mm punch biopsy was performed from one of the patches on the arm for histopathologic examination. The histologic examination revealed well-circumscribed non-caseating granulomas in the upper and lower dermis with a sparse interstitial lymphohistiocytic infiltration, a finding that is otherwise known as "naked tubercles" (Figs. 2A and B). Periodic acid Schiff and Ziehl Neelsen stains were both negative, excluding the possibility of fungal and mycobacterial infections. Scattered multinucleated giant cells were also observed. Reticulum staining showed fibers that were stained black by silver granules, surrounding and infiltrating the granulomas (Fig. 2C). There were no asteroid or Schaumann bodies.
In order to rule out the possibility of systemic involvement, additional examinations were performed. The chest X-ray showed no abnormal findings and the results of the complete blood cell count, blood chemistry, and urinalysis were within normal limits. The serum acetylcholinesterase level was checked to estimate the total granuloma burden, and was also normal.
The patient applied mild corticosteroids and 0.1% tacrolimus on the lesions. Significant improvement was observed after 1 month of application; however, the patient was lost to follow-up thereafter.
Sarcoidosis is a multisystemic disorder of unknown etiology. Although the lungs are most frequently involved, there are accompanying skin lesions in 25% of all patients1. Due to its variable clinical presentation, it is otherwise known as a "great mimic" and a thorough evaluation is needed to make the diagnosis. Sarcoidosis presents most frequently between the 3rd and 5th decades, and can be hereditary.
Cutaneous sarcoidosis is classified into specific and non-specific types, depending on the presence of non-caseating granulomas on histologic examination2. Non-specific skin lesions are often associated with an acute presentation of sarcoidosis, and lead to a good prognosis. The most common non-specific lesion is erythema nodosum. Other lesions include erythema multiforme, prurigo, calcifications, and nail clubbing. Specific manifestations include plaques, papules, nodules, scar sarcoidosis, ulcers, hypopigmented macules, erythroderma, lupus pernio, and alopecia3, among others. These types are more chronic and tend to resolve with scarring4. Our patient presented with specific skin lesions that were confirmed by biopsy, but differed from conventional cases in that topical treatment resulted in prompt amelioration with no evidence of scarring.
The diagnosis of cutaneous sarcoidosis relies upon the clinician's precise morphologic determination, followed by histologic examination, laboratory work-up, and interdepartmental collaboration between several medical specialties. Because cutaneous sarcoidosis is a diagnosis of exclusion, one can never be 100% certain of the diagnosis. Therefore, the differential diagnosis of other possibilities, such as tuberculosis, atypical mycobacterial infection, fungal infection, or foreign body reactions is essential. Because skin lesions are often the presenting symptom or the precursor of systemic disease, patient monitoring on a regular basis is mandatory5. Gallium-67 scanning may be useful in diagnosing sarcoidosis when typical patterns of uptake are observed6. The Panda sign refers to uptake in the nasopharynx, lacrimal and parotid glands, while the lambda sign is correlated with uptake in the perihilar lymph nodes.
The treatment of cutaneous sarcoidosis is often difficult with a high rate of recurrence and the many refractory lesions. Many modalities have been attempted with moderate success, including drugs, such as pentoxifylline, thalidomide, and infliximab. A novel therapeutic option for patients with progressive cutaneous sarcoidosis is systemic treatment with etanercept7. These drugs seem to show their effect through inhibition of tumor necrosis factor-α. Nonetheless, worldwide accepted standard therapies for sarcoidosis include the administration of corticosteroids, antimalarials, and methotrexate8. Steroids function by suppressing the pro-inflammatory cytokines and chemokines involved in cell-mediated immune responses and granuloma formation9.
Our patient presented with multiple erythematous macules and patches on the extremities and trunk. The lesions were slightly scaly and completely flat, with no evidence of induration or atrophy, unlike the plaques or papules commonly observed in sarcoidosis. This clinical appearance was unlike any other form reported in the literature, for the macular form usually presents as hypopigmented or atrophic macules10, and the patch or erythrodermic form is more extensively distributed, mimicking Sezary's syndrome10,11. The precise incidence of such forms is difficult to estimate due to the rarity of such cases5.
A review of the Korean dermatologic literature shows that subcutaneous nodules are the most common form of cutaneous sarcoidosis in Korean patients12, and although there are some reports of the macular or patch form, the lesions were associated with varying degrees of elevation, induration, or atrophy. Although more cases are needed for confirmation, it is worth considering this form as a new clinical variant of cutaneous sarcoidosis. It is important to note that sarcoidosis may present as flat erythematous patches and macules, so that in the future, on confronting cases with a similar presentation, we must keep sarcoidosis in mind as one of the differential diagnoses.
Figures and Tables
Fig. 1
Multiple erythematous, slightly scaly macules and patches on the back (A), thigh (B), and right arm (C).

Fig. 2
(A) Histologic examination shows a well-circumscribed, non-caseating granuloma in the lower dermis (H&E, ×100). (B) The magnified view shows a multinucleated giant cell within the granuloma (H&E, ×400). (C) Reticulum staining reveals numerous granulomas containing fibers stained black by silver granules, surrounding and permeating the granulomas (Reticulum stain, ×400).
References
1. Ji R, Koh MS, Irving LB. Cutaneous sarcoidosis. Ann Acad Med Singapore. 2007. 36:1044–1045.
2. Fernandez-Faith E, McDonnell J. Cutaneous sarcoidosis: differential diagnosis. Clin Dermatol. 2007. 25:276–287.

3. Akhdari N, Skalli HD, Lakhdar H. Erythematous lesions on the scalp. Sarcoidosis. Arch Dermatol. 2004. 140:1003–1008.
4. Marchell RM, Judson MA. Chronic cutaneous lesions of sarcoidosis. Clin Dermatol. 2007. 25:295–302.

5. Tchernev G. Cutaneous sarcoidosis: the "great imitator": etiopathogenesis, morphology, differential diagnosis, and clinical management. Am J Clin Dermatol. 2006. 7:375–382.
6. Sulavik SB, Spencer RP, Weed DA, Shapiro HR, Shiue ST, Castriotta RJ. Recognition of distinctive patterns of gallium-67 distribution in sarcoidosis. J Nucl Med. 1990. 31:1909–1914.
7. Tuchinda C, Wong HK. Etanercept for chronic progressive cutaneous sarcoidosis. J Drugs Dermatol. 2006. 5:538–540.
8. Doherty CB, Rosen T. Evidence-based therapy for cutaneous sarcoidosis. Drugs. 2008. 68:1361–1383.

9. Grutters JC, van den Bosch JM. Corticosteroid treatment in sarcoidosis. Eur Respir J. 2006. 28:627–636.

10. Alexis JB. Sarcoidosis presenting as cutaneous hypopigmentation with repeatedly negative skin biopsies. Int J Dermatol. 1994. 33:44–45.

11. Yoon CH, Lee CW. Case 6. Erythrodermic form of cutaneous sarcoidosis. Clin Exp Dermatol. 2003. 28:575–576.
12. Kim DH, Park YM, Kang H, Cho SH, Choi SW, Byun DG, et al. Seven cases of cutaneous sarcoidosis. Korean J Dermatol. 2000. 38:1070–1074.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download