I. Introduction
II. Methods
1. Conceptual Model
2. Data
3. Analytical Methods
 is coefficient estimate.
is coefficient estimate.Journal List > Healthc Inform Res > v.24(4) > 1107277
 is coefficient estimate.
is coefficient estimate.
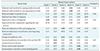
Factor loadings over 0.5 appear in bold.
HIE: health information exchange, Factor 1: improvement in diagnosis and communication, Factor 2: improvement in provider-patient relations, Factor 3: decrease in duplication and healthcare costs, Factor 4: convenience of HIE, Factor 5: concerns about information security and system reliability, Factor 6: expedited care process.

Exp. Inp.: recent experience with inpatient care, Exp. Outp.: recent experience with outpatient care, Health status: self-reported health status, Exp. Offline: experience with offline-based information exchange, Per. Ease: perception as to the ease of use of health information exchange (HIE), Per. Conv.: perceived benefit of the convenience by reducing work involved in information exchange, Per. Exped.: perceived benefit of the expedited care process, Per. Diag.: perceived benefit of improved diagnosis and communication with doctors, Per. Red. Costs: perceived benefit of reduced duplication and healthcare costs, Per. Pro. Rel.: perceived benefit of improved provider-patient relations, Per. Sec & sys.: perceived concern about information security and system reliability, Att. Need: attitude towards the need for HIE, Att. Paying: attitude towards the need for paying providers for the provision of HIE, Int. Use: intention to use HIE.
*p < 0.05, **p < 0.01, ***p < 0.0001.

Exp. Inp.: recent experience with inpatient care, Exp. Outp.: recent experience with outpatient care, Health status: self-reported health status, Exp. Offline: experience with offline-based information exchange, Per. Ease: perception as to the ease of use of health information exchange (HIE), Per. Conv.: perceived benefit of the convenience by reducing work involved in information exchange, Per. Exped.: perceived benefit of the expedited care process, Per. Diag.: perceived benefit of improved diagnosis and communication with doctors, Per. Red. Costs: perceived benefit of reduced duplication and healthcare costs, Per. Pro. Rel.: perceived benefit of improved provider-patient relations, Per. Sec & sys.: perceived concern about information security and system reliability, Att. Need: attitude towards the need for HIE, Att. Paying: attitude towards the need for paying providers for the provision of HIE, Int. Use: intention to use HIE.
*p < 0.05, **p < 0.01, ***p < 0.0001.
Hayoung Park 
https://orcid.org/0000-0001-5000-5043