Abstract
Objectives
Many healthcare organizations and professionals have had interests in healthcare information and communication technology (ICT). The objective of this study was to investigate the current status of overall healthcare ICT, especially focusing on Electronic Medical Record (EMR) systems in Korea.
Methods
This study used a part of the nationwide survey collected for the OECD benchmarking ICT study. The Health Insurance Review and Assessment Service conducted the survey from November 19, 2013 to January 10, 2014. This study followed the methodological guidelines of the OECD. A total of 2,093 hospitals and clinics, including long-term care hospitals, participated in the survey. Among them, 554 hospitals and 906 clinics were included in this study for the generalization of the results.
Results
The adoption rates of EMR systems were 96.3% in hospitals and 95.7% in clinics. Most of the hospitals and clinics had high rates of healthcare information exchange (HIE) within the organization; however, there were extremely low HIE rates among external organizations. Most of the hospitals and clinics had EMR systems with clinical-decision-supporting functionalities. Ninety-six percent of the EMR systems of the hospitals and 89.2% of the clinic systems had checking functions, such as alerts or reminders, on contraindications of drug-drug and drug-age interaction.
Healthcare information and communication technology (ICT) in the heath sector can improve the quality of care, managerial efficiency, and cost savings [12345]. For these reasons, many countries, including members of the Organisation for Economic Development and Cooperation (OECD) have been interested in ICT in the health sector and the dispersion of ICT into the healthcare industry.
Recently, the OECD, representing 30 countries, started a pilot project to benchmark ICT in the health sector, which is measuring the healthcare ICT status of each member country with a common model survey questionnaire and methodological guidelines [6]. The project was to facilitate cross-country data collection and comparison, and to promote the availability and use of health ICTs. Each country can learn about healthcare ICT from others through this kind of international research collaboration.
These efforts actually started at the beginning of 2012. On January 30–31, 2012, the OECD conducted an international workshop, Benchmarking Adoption and Use of Information and Communication Technologies in the Health Sector, in Paris, France, to develop a common questionnaire and methodological guidelines. On April 17–21, 2013, the OECD-EU held a joint EC-OECD workshop in Brussels, called Benchmarking Information and Communication Technologies in Health Systems. Member countries discussed methodological guidelines and made presentations regarding how they would conduct the survey. Since then, several studies have been conducted following the OECD methodological guidelines [7].
The Health Insurance Review and Assessment Service (HIRA) is one of the independent governmental agencies responsible for running the national health insurance program in Korea, providing professional health insurance claim review and assessment services. The HIRA participated in the workshop in 2013, and presented its plan to collect health ICT data. As a practical way of being involved in the pilot project, the HIRA reserved and allocated a research project fund at the end of 2012 for the annual budget for 2013. The HIRA started the survey at the end of September 2013 to collect information on ICT usage in the health sector and completed the survey at the end of February 2014. Thus, this report is the first result of the survey.
The HIRA hopes that this participation and the results of the survey will contribute to international cooperation between Korea and the member countries of the OECD. The study results could also be used to develop good political alternatives to improve the ICT status of the health sector and the expansion of ICT use in the health sector and the healthcare industry in general. The results of this project will also provide policy makers with important information about how ICT diffusion in various healthcare domains proceeding in South Korea.
The objective of this project was to investigate the ICT status of the health sector in South Korea. The survey results and data collected in this study will be used to enhance international cooperation with OECD member countries through benchmarking studies with other countries on health ICTs. The results will also be used to establish various political initiatives regarding ICT in the health sector in Korea.
The target population of this study was 280 general hospitals, 1,371 small hospitals, and 26,063 clinics, excluding tertiary hospitals and long-term care hospitals in Korea. This study excluded tertiary hospitals and long-term care hospitals because the general characteristics of both types of hospitals differ from those of general and small hospitals. Among the target population, this study selected 280 general hospitals as study subjects in addition to 288 small hospitals and 1,349 clinics. The proportions of the sample of small hospitals and clinics were 21.0% with a 5% sampling error and 3.5% with a 3% sample error, respectively. Respondents of the survey were general/primary care/family practitioners in ambulatory settings and chief information officers and administrators in hospitals following the standard methodological guidelines of the OECD. For simplicity and the generalization of the study results, this paper uses the term ‘hospitals’ to refer to both general hospitals and small hospitals.
The HIRA, an independent government agency dealing with the national health insurance system in Korea, has actively participated in the various cooperative activities of the OECD, such as healthcare quality improvements and the development of healthcare quality indicators including ICT projects. Data collection methods were face-to-face interviewing and the administration of an online survey. After the survey had been completed, it was found that 96% and 4% of the respondents had participated in the survey through interviews and the online survey, respectively. The HIRA conducted the survey from November 19, 2013 to January 10, 2014. For this work, 681 hospitals and 906 clinics were randomly selected, representing 40.2% and 5.2% of each target population. The response rates of hospitals and clinics were 86.9% and 67.2%, respectively.
The model questionnaire was composed of two parts. One was concerned with the current Electronic Medical Record (EMR) status of general/primary care/family practitioners in ambulatory settings, and the other was concerned with the EMR status of hospitals targeting the chief information officers and administrators. The organization of health systems across OECD countries varies significantly. Therefore, we tried to follow the OECD's methodological guidelines on definitions, sampling methods, sample size, and so on, to produce internationally comparable statistical indicators.
The HIRA administratively constructed a survey support network. First, the Ministry of Health and Welfare provided various administrative supports, such as official administrative letters. The HIRA selected a survey expert company through open bidding. We provided the company with basic information on the target population. The company randomly selected a sample using hospitals and clinics and conducted the survey. Before starting the survey, the HIRA also requested survey supports to professional groups, such as the Korean Hospital Association.
The company selected survey interviewers who had some previous experience conducting IT surveys or survey on the healthcare sector. The number of interviewers involved in this survey was 61 persons. The company educated them for 2 days. They had to attend a 2-hour education program each day. The company also conducted a pre-survey to identify potential problems of the survey instruments for one week and reflected any findings in the survey instruments, such as correcting the translation of the survey instrument into the Korean language.
This study also randomly selected a substitute sample. If respondents in the main sample group chose not to participate in the survey, we used the substitute sample. As mentioned above, the response rates were 86.9% for hospitals and 67.2% for clinics. Among the sampled hospitals and clinics, 266 general hospitals (response rate [RR] = 95.0%), 288 small hospitals (RR = 80.4%), and 906 clinics (RR = 67.2%) participated in the survey.
This study was an explanatory study on the current status of healthcare ICT, especially focusing on EMR systems in Korea; therefore, statistical modeling and association analysis were not conducted. However, the two types of facilities (hospitals and clinics) are important, so each variable was tabulated by the type of facility and then statistical tests, such as the chi-square test of independence, were conducted. If the table had more than two by two matrices, then the Mantel-Haenszel chi-square test was conducted. Finally, to ensure the clarity and accuracy of the results, the cases in which a respondent answered “I don't know” were excluded from the analysis. All the descriptive statistical analyses were conducted using SAS ver. 9.1 (SAS Institute Inc., Cary, NC, USA).
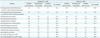
Table 1 presents the general characteristics of the study subjects. Forty-three percent of the hospitals and 50.9% of the clinics were located in the mega-metro cities. Fifty-six percent of the clinics provided primary care, and 44.3% of respondents provided specialty care. For the question asking the teaching status of hospitals, 28.7% of hospitals replied that they were teaching hospitals. The average number of full-time physicians for the clinics was 1.4 persons. Approximately 82% of the clinics had only one physician working at the clinic.
This study investigated the adoption rate of EMR systems in hospitals and clinics (Figure 1). For the definition of EMR we followed the methodological guidelines of the OECD. Sixty-eight percent of the hospitals (376) surveyed were fully adopting EMR systems. Twenty-nine percent of the hospitals (163) were adopting partial EMR systems, and the rest of the hospitals, 2.7% (15), did not have any EMR system. Therefore, the adoption rate of any EMR system was 97.3% (539) in hospitals. For clinics, the full adoption rate was 67.8% (614). The partial and no EMR adoption rates were 27.9% (253) and 4.3% (39), respectively. Thus, the proportion of clinics having any type of EMR system were 95.7% (867).
Table 2 presents the availability or usage of patient data created within the organization. Hospitals routinely used data about patient demographics (80.8%), diagnosis (75.9%), and active/current medication lists (74.3%) in the order of high usage frequency. Clinics also have a similar pattern with hospitals. Data about patient demographics (83.9%), diagnosis (77.8%), and active/current medication lists (77.3%) was used in the order of high frequency.
Table 3 shows the availability and use of data in EMR systems created outside the organization. In all questionnaire items, less than 3% of hospitals routinely used data that was generated outside the organization. Less than 2% of clinics said that they could use patient data created outside the clinics.
Regarding the availability and use of EMR systems to prescribe medication, 94% of hospitals routinely used electronic systems. Eighty-nine percent of clinics routinely used them to prescribe medications. Regarding whether hospitals and clinics could issue medication prescriptions to outside pharmacies through electronic systems, 15% of hospitals could send their prescriptions to outside pharmacies, whereas 79% of hospitals could not. Fifteen percent of clinics had electronic systems for sending their prescriptions to outside pharmacies, but 76.4% did not (Table 4).
The survey asked a question about whether the systems allow physicians to access information on the dispensing status of drugs by pharmacists working in pharmacies outside the hospital or clinic. Such access was not available at all in any of the hospitals or clinics. Regarding whether the electronic systems allow physicians to perform some specific functions, such as listing patients or medication orders, 85% of hospitals and 58.8% of clinics said that they were able to list patients who are due for tests, which is a statistically significant difference between the two groups (p < 0.001). However, the capability to list medications ordered from outside the organization or dispensed outside the organization was not available to hospitals or clinics.
Regarding general health management (Figure 2), 70% of hospitals and 44.8% of clinics were able to list patients by diagnosis. Fifty-eight percent of hospitals and 35.9% of clinics were able to list patients by lab result.
Almost 30% of hospitals used EMR systems that have functionalities for clinical guidelines, protocols, and best practices. Approximately 75% and 95.8% of hospitals used structured order sets and drug-drug interaction/contradictions alerts function in their EMR systems, respectively. Around 44% and 89.2% of clinics had EMR systems with functions of structured order sets and drug-interaction/contradictions alerts, respectively (Table 5).
Table 6 presents the degree of healthcare information exchange (HIE) within organizations. More than 75% of the hospitals and clinics surveyed routinely used all specified items except items of receiving radiology test reports and images.
Table 7 presents the degree of HIE coming from outside the organizations. The rate of HIE was extremely low in both hospitals and clinics. Almost 90% of hospitals and 97% of clinics said that HIE was not available.
The objective of this project was to investigate the healthcare ICT status of Korea following the OECD's guidelines measuring ICT in the healthcare sector. The project plan, design, and implementation were conducted by the HIRA as a stand-alone survey. However, data collection was carried out by a professional survey company through a contract with the HIRA.
We found a number of facts through this survey project. The rates of EMR system adoption in hospitals and clinics were 96.5% and 95.7%, respectively. The overall adoption rates were much higher than those found in studies conducted in the following year [8]. The study found that the adoption rates in tertiary hospitals and general hospitals were 97.3% and 91.4%, respectively. The main methodological difference between the two studies was that the former study used face-to-face interviews, and the latter study used a mail or online survey. The adoption rate in Korean hospitals was much higher than that in European Union countries, but the rates were similar in clinics [91011121314]. This study showed that EMR systems allow medical professionals to access various types of clinical data for individual patients electronically within each organization, but access was not available to data from outside of each organization. For example, 95.8% of hospitals and 94.1% of clinics routinely or occasionally used patients' demographic information created within the organization. In contrast, only 9.7% of hospitals and 2.2% of clinics had access to such information from outside the organization. Most of the hospitals (94.3%) and clinics (89.2%) surveyed were prescribing medications through electronic systems. Most of the hospitals and clinics exchanged health care information on patients and related data within the organization. However, there was lack of HIE with external organizations. This may be related to several complex issues, such as patients' privacy protection and legal requirements, as well as information security issues and technological infra-structural problems, such as network issues. In Korea, the vast majority of hospitals still do not allow external access to their electronic patient records.
This study briefly overviewed the survey results on the current healthcare ICT status of hospitals and clinics in Korea. However, this study had several limitations. First, the OECD survey model may not fit the situation of Korea well. For example, the OECD asked about the availability of HIEs within organizations. In Korea, the implementation rate of computerized physician order entry (CPOE) systems has been very high. The CPOE also has functionalities of HIE. Thus, most of the respondents might have been confused about whether the HIE within the organization means HIE coming from EMR or CPOE. This confusion might have affected the study results, regarding the high availability of HIE within organizations. Second, the survey itself could have been heavily dependent on the memories of the respondents. This is because most of the survey contents were composed of the questionnaires recording the availability of functions or degree of HIE. A future study should use more objective ways of recording EMR system adoption. Although this study had some limitations, most OECD model surveys have these common issues. It is hoped that future work could investigate adoption rates using more objective methods or visual verification or confirmation of EMR installation or EMR screen shots.
The survey findings could provide useful insights to the OECD members and other countries. The results can be used for comparative analysis or an example of how to investigate the current status of EMR systems. We believe that the results of this project could especially be useful for ICT policymaker of other foreign countries. This project may enhance healthcare policymakers' understanding of hospitals' EMR system adoption and use behaviors. Identifying related factors is important because actual benefits from the systems would occur through hospitals' adoption of health ICT systems, their use, and healthcare information exchanges with other organizations. Using information derived from this study, they may design more effective and efficient strategies or roadmaps to achieve their IT diffusion policy goals [151617].
We expect that the results of this study will provide hospital managers, scholars, and politicians working in the health informatics field with useful information on factors affecting health ICT adoption, use, and HIE with other organizations. We also expect that the results can be used to eliminate some of the barriers to adopting EMR systems and to accelerate system adoption and use, which will indirectly contribute to the improvement of health outcomes in healthcare organizations.
Figures and Tables
References
1. Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006; 144(10):742–752.

2. Campanella P, Lovato E, Marone C, Fallacara L, Mancuso A, Ricciardi W, et al. The impact of electronic health records on healthcare quality: a systematic review and meta-analysis. Eur J Public Health. 2016; 26(1):60–64.

3. Kamau N. Electronic health documentation and its impact on nurses routine practices [master's thesis]. Helsinki, Finland: Laurea University of Applied Sciences;2015.
4. Bowman S. Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013; 10:1c.
5. Khangura S, Grimshaw J, Moher D. Evidence summary: Electronic Health Records (EHRs): to the chief information officer of the Champlain LHIN. Ottawa, Canada: Ottawa Hospital Research Institute;2010.
6. Organisation for Economic Co-operation and Development. Draft OECD guide to measuring ICTs in the health sector. Paris, France: Organisation for Economic Co-operation and Development;2015.
7. Zelmer J, Ronchi E, Hypponen H, Lupianez-Villanueva F, Codagnone C, Nohr C, et al. International health IT benchmarking: learning from cross-country comparisons. J Am Med Inform Assoc. 2017; 24(2):371–379.

8. Kim YG, Jung K, Park YT, Shin D, Cho SY, Yoon D, et al. Rate of electronic health record adoption in South Korea: a nation-wide survey. Int J Med Inform. 2017; 101:100–107.

9. Codagnone C. Benchmarking information and communication technologies in health systems: adoption of ehealth among general practitioners. In : Proceedings of the Joint EC-OECD Workshop; 2013 Apr 18-19; Brussels, Belgium.
10. Maghiros I, Sabes-Figuera R. European hospital survey: benchmarking deployment of e-health services. In : Proceedings of Joint EC-OECD Workshop; 2013 Apr 18-19; Brussels, Belgium.
11. Deidda M, Lupianez-Villanueva F, Maghiros I. European hospital survey: benchmarking deployment of ehealth services (2012–2013): methodological report. Luxembourg: European Commission;2013.
12. Sabes-Figuera R, Maghiros I. European hospital survey: benchmarking deployment of e-health services (2012–2013): synthesis outcomes. Luxembourg: European Commission;2013.
13. Price Waterhouse Cooper on behalf of JRC-IPTS. European hospital survey: benchmarking deployment of ehealth services (2012–2013): final report. Luxembourg: European Commission;2014.
14. European Commission. European hospital survey: benchmarking deployment of e-health services (2012–2013): questionnaire addressed to the CIOs of acute care hospitals (translated versions). Luxembourg: European Commission;2014.
15. Lee M, Heo E, Lim H, Lee JY, Weon S, Chae H, et al. Developing a common health information exchange platform to implement a nationwide health information network in South Korea. Healthc Inform Res. 2015; 21(1):21–29.

16. US Department of Health and Human Services, Centers for Medicare & Medicaid Services. Medicare and Medicaid programs; electronic health record incentive program: Stage 3 and modifications to meaningful use in 2015 through 2017. Fed Regist. 2015; 80(200):62761–62955.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download