Abstract
Objectives
Over the past decade, hospitals and clinics have gradually adopted hospital information systems, including provider order entries and electronic health records. Although these systems have helped to improve patient safety and efficiency of healthcare providers, not all healthcare providers and patients are satisfied with the current situation. Healthcare should be smarter. Thus, there is a need for state-of-the-art medical and healthcare devices that can handle massive amounts of data with the help of sophisticated information processing and discovery technologies.
Methods
This article compares hospital information systems with the information systems of other social infrastructures. It also explores the possibilities of smarter healthcare, including personal health devices and personal health records with interoperability.
In recent decades, information technology (IT) has dramatically enhanced our lifestyle with greater levels of efficiency and convenience. It has also changed our clinical practices, though some doubt whether IT has helped clinical practices achieve the high levels of efficiency and effectiveness previously expected.
There are many examples that illustrate how IT has made our daily lives more efficient and convenient. Point-of-sales systems are one example; they have bar code readers or radio frequency identification readers that can collect products and sales data at registers. Car navigation systems with touch panel displays and voice guidance are another example; they have made modern cars smarter than conventional cars, which have always relied on the brake, accelerator, and steering wheel as main human-machine interface. A third example features non-contact IC card ticketing systems, which automatically provide data on when and where the user has used the card. The focus of this study is on two common properties of these types of systems: the generation of large volumes of data (beyond the normal processing capabilities of humans) and the unique devices that act as an interface between computer systems and the real world.
Although IT has changed clinical practices, some think the changes have not produced the expected levels of efficiency and effectiveness. For instance, the data of hospital information systems are limited to the contents of paper medical charts and are therefore within the scope of human processing. Moreover, desktop and laptop computers are the main devices that healthcare providers use to interface with hospital information systems.
This article examines why the use of IT in clinical practices lags behind our use of IT in our modern lifestyle. The basic question is how can IT be efficiently and effectively utilized in healthcare.
Expectations for hospital information systems have grown since the early 2000s when the US Institute of Medicine published To err is human [1] and Crossing the quality chasm [2]. The focus of those publications was on safety, effectiveness, a patient-centered approach, timeliness, efficiency, and equitableness. These features were the hallmarks of well-designed systems. Although the word system can apply to many things, the concept of an information system evokes high expectations.
The Japanese Ministry of Health, Labour and Welfare published a report titled A grand design of information systems in healthcare [3]. It emphasizes that information sharing, quality improvement, and efficiency and safety in healthcare should be incorporated into electronic health records. To attain these goals, the Japanese government subsidized hospitals which adopted electronic health records. They expected more than 60% of hospitals with more than 400 beds to adopt electronic health records systems by 2006 [4]. In 2011 that goal has still not been accomplished. One reason for this failure is the high cost of hospital information systems. In addition, many healthcare providers are skeptical about the system capabilities, especially in light of the disappointment expressed by various early adopters.
It is becoming a common practice for hospitals to implement hospital information systems by selecting and combining off-the-shelf products. One of the major components of hospital information systems is the electronic health record system. Discussing the functionalities of electronic health record systems is a good to determine why hospital information systems fail to generate a large amount of data. The functionalities of electronic health records have been listed elsewhere [5,6]. However, most off-the-shelf products handle provider order entries (POEs), results management, document management, and billing processes. Of these functions, the POE functions are the most important and widely used.
Figure 1 shows a diagram of clinical processes. When observing a patient, a physician first tries to detect any abnormalities. Later the physician uses the available data and information to assess the patient's condition. In the action phase, the physician or another medical practitioner conducts various clinical tests or procedures. After the action phase, the patient is observed and evaluated again. Note that the POE is used when the physician communicates with other healthcare providers. The amount of data generated by the POE function may be limited to the amount of data recorded on paper slips. Furthermore, the data of all the clinical processes must be gathered. One of the goals of designing and implementing electronic health record systems is to ensure that all the clinical processes are automatically captured as a by-product of clinical practices.
A large amount of data must be fed into computer systems so that the systems can fulfill their capabilities. Special devices must also be able to function as an effective human-machine interface. How a large amount of data can be utilized is an important question which can only be resolved by considering a data model and a hierarchy of information, knowledge, and wisdom [7,8]. Such a model has existed for many years. It is recognized as a basic principle of information science. Under this model, information is formed from data, knowledge is extracted from information and, ideally, wisdom is derived from knowledge. However, hospitals operate in the real world, not a conceptual world. So how can the data model be incorporated into the implementation of a system in the real world?
In the following description, we explore how data should be utilized in real-world settings. We consider a game with a six-sided dice. The dice has values from one to six. It is not a regular dice, and the value of six appears under a certain condition. Participants of the game predict when the value of six is likely to appear.
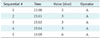
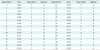
If appropriate IT were available, a system could be implemented to efficiently predict the value of six. How would such an information system be designed and implemented? As described above, the first step would be to design a system that can store enough data to produce information. For useful data storage, the database must be designed with certain kinds of attributes. In the dice example, the database should include attributes pertaining to the number sequence, the time, the value of the dice, and the operators who throw the dice (Table 1). The data can be stored as soon as the database is designed (Table 2). The next step is to analyze the data to determine which facts would be most useful for achieving the objective (in this case, predicting when number six will turn up). The data are then analyzed for the purpose of formulating various hypotheses. One hypothesis, for example, as shown in rows 2 to 5 and 9 to 12 in Table 1, could be that number six will appear after three consecutive appearances of number three, though this hypothesis is not supported by the data in rows 23, 25, and 29 of Table 1. Another hypothesis might be based on the time of the throws. For example, number six will appear exactly 5 minutes after the previous throw. All the data in the data table support this hypothesis. Thus, this hypothesis can be described as a pattern.
The confirmed hypothesis begs another question: how can the pattern be used to predict number six in real-world settings? One possibility (albeit one that is not highly efficient or convenient) is to use a stopwatch to measure the intervals between throws. Another possibility is to design and implement software that signals when exactly 5 minutes has elapsed since the previous throw. This type of implementation can be described as automation. A mobile device with such an automation app would guarantee success every time.
As described above, computers can handle much more data than the human brain can process. And the patterns which can be discovered in a large amount of data may be implemented as a system to automate processes. In this context, mobile devices can act as an interface to facilitate human interaction with information systems. Mobile devices capture the real world as data, and computers process the data. Then, as shown in Figure 2, mobile devices convert the processed data into information or automated notifications.
A new ward of Teikyo University Hospital, Tokyo, was opened in May 2009. With 1,154 beds, the hospital is one of the largest in Japan. It is also equipped with a state-of-the-art information system. The main traits of the system are IT governance, unification, and workflow efficiency. The IT governance capabilities enable hospital administrators to effectively control data management, IT assets, and system operations. Hospital administrators in Japan often have difficulty controlling their information systems and providing solutions for emerging problems. Most hospitals outsource all aspects of IT managements-from planning to maintenance. In such cases, the hospitals are restrained by the limitations of the IT vendors and are unable to improve their information systems without the IT vendors' help. The goal at Teikyo University was to enable the administrators to overcome problems by themselves. They now do the planning, designing, implementing, and maintenance of their own hospital information systems.
The unification feature helps minimize the physical IT resources, which in turn reduces the frequency of system failures and simplifies the system operations. The efficiency of the hospital workflows was improved as a result of a two and a half year survey of every single workflow in the hospital. All the workflows were documented in swim lane diagrams and visualized. The stakeholders used the visualized work-flow documentation to refine the workflows [9].
The network capabilities allow for three different networks to be integrated into a single physical network system. The first network is a closed local area network (LAN) system tailored for the hospital information system. The second network is linked to the Internet. The third one is a voice over Internet protocol (VoIP) system-one of the largest to be used in healthcare in Japan [10]. Each network has a wired LAN and a wireless LAN. There are about 1,500 PCs, 1,000 wired IP phones, and 1,200 wireless IP phones. The wireless IP phones are linked to a nurse call system, and patients can directly communicate with medical staff from their beds.
Another feature of the VoIP system is a messaging functionality which connects wireless IP phones to the hospital information system. For example, if a laboratory system detects an abnormal result, the system can send messages to members of the medical staff who are related to the patient with the abnormality. The hardware of the hospital information system was consolidated with server virtualization technology. More than 30 subsystems consisting of more than 50 physical servers work as virtual guest servers on seven physical hosting servers [11].
Service-oriented architecture was adopted as the system architecture. It has a number of independent Web services that provide basic information for the hospital information system; one of them provides patient information. A business process execution language (BPEL) engine was deployed. The BPEL engine coordinates and orchestrates the Web services for efficient and effective hospital workflows [12]. The hospital information system has a 30 terabyte clinical data repository and a 120 terabyte PACS; the system generates about 2 million data entries a day.
Modern medicine can be described as reactive, disease-oriented, and sporadic. It is reactive because patients seek medical services as a result of unpleasant experiences such as pain and fear. It is disease-oriented because patients and physicians alike try to detect the patients' abnormalities. It is sporadic because the relationship between a patient and physician tends to terminate when the patient is cured or if the patient dislikes the physician. The paradigm of modern medicine works fine as long as there are sufficient medical resources (such as labor and capital) and the targeted population is relatively limited. Over the next several decades, medical services will face problems with an aging society and financial difficulties. There is a need for a new paradigm of medicine-one that supports sustainable healthcare systems.
The new paradigm must be proactive, lifestyle-oriented, and continual. A proactive approach means people strive to keep healthy. Instead of focusing on disease, medical and healthcare advice can be oriented to a positive lifestyle. The relationship between patients and healthcare providers can be continual as patients participate more fully in the management of their diseases and health. IT can support the new paradigm [13]. Standardized messaging protocols between healthcare devices and computers can be used to record health data. The guidelines of the Continua Health Alliance include standardized protocols for personal health devices [14].
Personal health record (PHR) systems must have standards-compliant interfaces. Some widely adopted standards are the Continuity of Care Record from ASTM International [15] and the Continuity of Care Document from HL7 [16]. The Division of Biomedical Informatics at Seoul National University and Teikyo University Medical Information and Systems Center have started a proof of concept trial to assess the interoperability of PHR data among PHR services [17]. PHR systems with Continuity of Care Record compliance are being used in the trial.
Traditional medicine relies on laboratory tests, physiology studies, imaging studies, and patient monitors to examine the status of tissues, organs, and human bodies. These types of examinations provide fundamental data on clinical practices. The advancement of genomics has enabled the status of genomes and cells to be observed through gene sequences and gene expressions (Figure 3). In contrast with most traditional studies, genomic studies produce results which are first processed by a machine so that humans can read them and recognize their significance. Computers are indispensable for data processing in bioinformatics.
In the next few decades, there will be an exponential increase in life data from PHRs, blogs, and social network services. Hospitals treat diseases, not health. Modern imaging techniques can visualize states of mind and thoughts. Soon the data of social network services will be used to analyze a patient's moods and state of mind. And these factors may be the key to understanding the meaning of health [13].
Data should be processed and presented to humans to enable them to act on the processed data. General warnings are sometimes ineffective because they deemed to be intended for somebody else. However, they can be effective if presented in a timely, context-based, and personalized manner. Such systems can be designed to include the components of modeling and prediction (Figure 4), albeit with the overhead of greater computer resources and smarter algorithms. Nevertheless, smarter healthcare can be achieved by leveraging the full capabilities of devices, data, and sophisticated algorithms.
Figures and Tables
References
1. Kohh LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. 2000. Washington DC: National Academy Press.
2. Institute of Medicine (US). Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. 2001. Washington DC: National Academy Press.
3. A grand design of information systems in healthcare [Internet]. Ministry of Health, Labour and Welfare of Japan. 2001. cited at 2011 Aug 1. Tokyo: Ministry of Health, Labour and Welfare of Japan;Available from: http://www.mhlw.go.jp/shingi/0112/s1226-1a.html.
4. A work schedule of information systems in healthcare [Internet]. Ministry of Health, Labour and Welfare of Japan. 2001. cited at 2011 Aug 1. Tokyo: Ministry of Health, Labour and Welfare of Japan;Available from: http://www.mhlw.go.jp/shingi/0112/s1226-1c.html.
5. Electronic health record/personal health record [Internet]. Health Level Seven International. c2077-2011. cited at 2011 Aug 1. Ann Arbor, MI: Health Level Seven International;Available from: http://www.hl7.org/implement/standards/ehrphr.cfm.
6. Electronic health record (EHR) [Internet]. Healthcare Information and Management Systems Society. cited at 2011 Aug 1. Healthcare Information and Management Systems Society;Available from: http://www.himss.org/ASP/topics_ehr.asp.
7. Rowley J. The wisdom hierarchy: representations of the DIKW hierarchy. J Inf Sci. 2007. 33:163–180.

8. Zins C. Conceptual approaches for defining data, information, and knowledge. J Am Soc Inf Sci Technol. 2007. 58:479–493.

9. Saito K. CIO magazine: a case file [Internet]. Teikyo University Hospital. 2009. cited 2011 Aug 1. Tokyo: IDG Japan;Available from: http://www.ciojp.com.
10. VoIP system: Teikyo University Hospital [Internet]. NEC Corporation. c1994-2011. cited 2011 Aug 1. Tokyo: NEC Corporation;Available from: http://www.nec.com/global/cases/teikyo-uh/contents.html.
11. Teikyo University Hospital: realizing IT governance in healthcare [Internet]. Nikkei Medical Online. c2006-2011. cited 2011 Aug 1. Tokyo: Nikkei Business Publications Inc;Available from: http://medical.nikkeibp.co.jp/leaf/all/special/it/casestudy/201005/515206.html.
12. Teikyo University Hospital improves patient care by enabling real-time data delivery to doctors. Oracle customer case study [Internet]. Oracle. c2010. cited 2011 Aug 1. Redwood Shores, CA: Oracle;Available from: http://www.oracle.com/us/corporate/customers/teikyo-case-study-080251.pdf.
13. Reforming hospital information systems [Internet]. RBB Today. 2010. cited 2011 Aug 1. Tokyo: RBB Today;Available from: http://www.rbbtoday.com/article/2010/07/17/69227.html.
14. Continua Health Allicance [Internet]. c2010. cited 2011 Aug 1. Beaverton, OR: Continua Health Allicance;Available from: http://www.continuaalliance.org/index.html.
15. ASTM E2369 - 05e1 standard specification for continuity of care record [Internet]. ASTM International. c1996-2011. cited 2011 Aug 1. West Conshohocken, PA: ASTM International;Available from: http://www.astm.org/Standards/E2369.htm.
16. Clinical document architecture [Internet]. Health Level Seven International. c2077-2011. cited 2011 Aug 1. Ann Arbor, MI: Health Level Seven International;Available from: http://www.hl7.org/implement/standards/cda.cfm.
17. A proposal of PHR platform using cloud services [Internet]. Nikkei Medical Online. c2006-2011. cited 2011 Aug 1. Tokyo: Nikkei Business Publications Inc;Available from: http://medical.nikkeibp.co.jp/leaf/all/special/it/casestudy/201106/520224.html.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download