This article has been
cited by other articles in ScienceCentral.
A 73-year-old woman with systemic sarcoidosis (ocular, skin, and lung manifestations) was admitted to our institution with exertional dyspnea. Steroid treatment (prednisolone 30 mg/day with gradually decreasing dose to 5 mg/day after 12 months,) had been administered for 13 years before admission. At the current admission electrocardiogram (ECG) revealed right bundle branch block (
Figure 1A). Eight years later, the regularly checked ECG revealed a newly inverted T wave in leads V2–3 (
Figure 1B). Echocardiogram revealed mild right ventricular (RV) enlargement with moderate tricuspid regurgitation (TR). Furthermore, 6 months ago, the patient started experiencing exertional dyspnea. On admission, ECG revealed a newly inverted T wave in leads II, III, aVF, V4, and V5 (
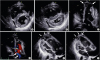
Figure 1C) and echocardiogram demonstrated severe RV dilatation with an apical aneurysm and severe TR, which compressed the left ventricle (
Figure 2), whereas left ventricular systolic function was not impaired and the thinning of interventricular septum was not detected. Cardiac catheterization testing revealed normal coronary artery, and ruled out pulmonary hypertension and volume overload. Further evaluation with cardiac magnetic resonance imaging confirmed RV dilatation and dysfunction with apical aneurysm and revealed late gadolinium enhancement in the RV apical wall and basal septum (
Figure 3). [
18F]fluorodeoxyglucose positron emission tomographic scan demonstrated focal enhancement of the RV basal septum (standardized uptake value (SUV) max 2.1) (
Figure 4) with similar level of uptake in hilar lymph nodes (SUV max 2.9). Although the cardiac biopsy failed to detect the finding of sarcoidosis, the echocardiographic and radiographic images supported RV sarcoidosis. Prednisolone dose was increased to suppress progression of RV sarcoidosis. In the present case, the serial changes in ECGs remarkably corresponded with the progression of RV aneurysm, suggesting that routine ECG in patients with systemic sarcoidosis is useful for early detection of right cardiac involvement.
Figures and Tables
Figure 1
(A) Electrocardiogram (ECG) at the initial admission shows right bundle branch block. (B) ECG performed 8 years after the initial admission revealed a newly inverted T wave in leads V2–3. (C) At the current admission, the ECG shows a newly inverted T wave in leads II, III, aVF, V4, and V5.
Figure 2
(A, B) A transthoracic echocardiogram in the parasternal short axis view shows severe RV dilatation and LV compression (A: diastole, B: systole). (C, D) Apical four-chamber view reveals severe RV dilatation with apical aneurysm (C: arrows) and severe tricuspid regurgitation (D: arrows). (E, F) Apical four-chamber RV-focused view also shows RV aneurysm in diastole (E: arrows) and systole (F: arrows). LA: left atrium, LV: left ventricle, RA: right atrium, RV: right ventricle.
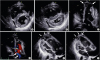
Figure 3
Functional (cine) cardiac magnetic resonance images in the four-chamber view in diastole (A) and systole (B) show normal LV function, RV dilatation and RV apical aneurysm. The corresponding cine (C) and contrast-enhanced magnetic resonance image (D) in the four-chamber view show late gadolinium enhancement in the RV apical wall (triangles) and basal septum (arrows). Ao: aorta, LV: left ventricle, PA: pulmonary artery, RV: right ventricle.

Figure 4
A [18F]fluorodeoxyglucose positron emission tomographic scan demonstrates focal enhancement of the intraventricular septum in the axial view (A and C: arrows) and in the coronal plane (B and D: arrows). LV: left ventricle, RV: right ventricle.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download