Introduction
Echocardiography plays an essential role in the evaluation of left ventricular (LV) diastolic function. Over the past decade, the diagnostic armamentarium was fortified by tissue Doppler imaging (TDI). The technique is based on recording the high amplitude, low frequency signals generated by tissue motion.1) Myocardial velocities can be measured in a longitudinal and a radial direction, and can be used to compute regional displacement and deformation. TDI has been successfully applied to study segmental LV systolic and diastolic function, since myocardial velocities are strongly related to interstitial fibrosis,2) beta-adrenergic receptor density,2) and regional cytokine expression.3) For examining global LV diastolic function, mitral annulus velocities are recorded by Pulsed-wave Doppler and the velocities can be measured on line from the spectral display (Fig. 1).
Relation of Early Diastolic Velocity to LV Relaxation and Preload
A number of observational studies4)5) have shown an inverse relation between age and the mitral annulus early diastolic velocity (e'). This observation is similar to other Doppler parameters which are age dependent, as the E/A (peak early filling velocity to peak late filling velocity) ratio in mitral inflow, and S/D (peak systolic to peak diastolic) ratio in pulmonary venous flow. In animal studies,6)7) e' related well to the time constant of LV relaxation (τ) and - dP/dt. Likewise, human studies8-10) have shown a significant inverse correlation between e' and τ.
The relation between e' and preload is more complicated. When LV relaxation is normal,6)7) preload is directly related to e'. On the other hand, preload has a minimal effect on e' with impaired LV relaxation (Fig. 2). These animal observations were also noted in humans when saline and nitroglycerin infusion8) had no effect on septal e' velocity in cardiac patients, whereas mean pulmonary capillary wedge pressure was directly related to e' in normal subjects.11) In summary, it is valid to use e' as a surrogate marker of LV relaxation in cardiac patients where LV relaxation is impaired, but not in normal individuals.
Relation of E' to Regional Function
Lateral e' velocity is usually higher than septal e' velocity.4) This difference can be exaggerated or reversed depending on the presence and extent of cardiac pathology. For example, this difference is exaggerated in patients with hypertrophic cardiomyopathy,12) septal infarction,13) or those with primary pulmonary hypertension.14) However, in patients with lateral wall infraction, septal e' velocity can be much higher than the lateral e' velocity.
An animal study15) showed that in the setting of myocardial ischemia, e' is dependent not only on global LV systolic and diastolic function, but also on regional thickening. Accordingly, it is imperative to use the average of septal and lateral e' velocities when drawing conclusions on LV diastolic function in patients with regional dysfunction.
Relation of E' to Cycle Length
Few studies have addressed this important question. We have noted in an animal model that e' is affected heart rate.15) Heart rate affected the transmitral pressure gradient (a higher heart rate reduces the transmitral pressure gradient), which in turn led to a reduced e'. Therefore, caution should be exercised in using e' to draw conclusions on LV relaxation in normal subjects with sinus tachycardia. On the other, e' relates significantly to τ in patients with cardiac disease, whether in regular tachycardia,16) or atrial fibrillation.17)
Doppler Assessment of LV Filling Pressures
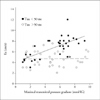
The ratio of mitral E velocity to annular e' velocity corrects for the effect of LV relaxation on mitral E velocity, and can be used to estimate LV filling pressures (Fig. 3). This method has been validated by several laboratories and used for patients with normal and depressed EF,4)10)18) sinus tachycardia,16)18) atrial fibrillation,17) pulmonary hypertension,14) and hypertrophic cardiomyopathy.12) It is usually not critical to use TDI in predicting LV filling pressures in patients with depressed EF. However, in patients with normal EF, TDI is the most reliable method for the assessment of LV relaxation and filling pressures.13)19) Importantly, 2 studies have shown the lateral velocity13)19) to be more accurate in that regard. However, if the septal velocity is used, an E/e' ratio <8 favors the presence of normal filling pressures, whereas a ratio >15 is usually associated with increased LV diastolic pressures.10) If the average of septal and lateral e' is used, a ratio <8 identifies patients with normal filling pressure, whereas a ratio >13 identifies those with increased filling pressures.13) When the ratio falls between these cutoffs, other echocardiographic measurements are needed. These include mitral inflow velocities, pulmonary venous flow velocities, pulmonary artery pressures, and LA volume index.
Comparison with BNP
BNP is currently used to determine the underlying etiology of dyspnea, as cardiac patients usually have an increased BNP level. The comparative performance of BNP and Doppler echocardiography was recently reported. BNP had a significant positive correlation with mean wedge pressure, but with a wide scatter.20) It also failed to detect changes in filling pressures with therapy. On the other hand, TDI (E/e' ratio) was more accurate in identifying patients with increased filling pressures, and tracked well the changes in mean wedge pressure with therapy.20)
Time Intervals
We observed in an animal model a decrease in the peak e' velocity and a delay in its onset with myocardial ischemia.15) Furthermore, e' is delayed (Fig. 4) such that it occurs after the onset of mitral E velocity.6)7) The time interval: TE-e' relates well with invasive indices of LV relaxation, and has been used for the estimation of LV filling pressures (in conjunction with end systolic pressure and isovolumetric relaxation time) in normal individuals, in patients with depressed EF, those with normal EF, and patients with mitral valve disease.21)22) The highest accuracy was obtained when the average time interval was computed from septal, lateral, anterior, and inferior TD signals.21) Recently, it was successfully used to identify patients with increased LV filling pressures23) when the E/e' fell in the indeterminate range of 8-15.
Role of TDI in Constrictive Pericarditis
Most patients with pericardial constriction have a normal or increased e' velocity (>7 cm/s). In this disease, septal e' velocity is usually higher than lateral e' velocity, and the E/e' ratio is inversely related to LV filling pressures.24) Recent studies have also noted that the presence of a reduced annular systolic velocity and a prolonged TE-e' are of value in borderline cases25) as they identify patients with primarily myocardial (as opposed to pericardial) disease.
Late Diastolic Velocity (a')
This velocity is affected by left atrial dP/dt and LV end diastolic pressure. Reduced left contractility leads to a decreased a' velocity. Likewise, an increase in LV end diastolic pressure (after-load) also leads to a decrease in a'.6) In patients with early diastolic dysfunction (impaired relaxation filling pattern), e'/a' ratio is reduced. With progressive diastolic dysfunction, a' velocity decreases, and e'/a' ratio is ≥1.8) Recently, e'/a' ratio was reported to identify well patients with diastolic heart failure as determined by high fidelity LV pressure/volume measurements.19)
Prognostic Power of Myocardial Diastolic Velocities
Mitral annulus e' velocity, a' velocity, and E/e' ratio have been shown to provide important prognostic information in several patient groups. This includes patients with heart failure,26-29) acute myocardial infarction,30) chronic renal failure,31) non-valvular atrial fibrillation,32) mitral regurgitation,33) cardiomyopathy,34)35) general community,36) and hypertension.37) In many of the above studies, TDI provided prognostic information that was incremental to clinical data, and conventional echocardiographic measurements.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download