Abstract
Purpose
We evaluated the relationship between the degree of osteopontin (OPN) expression in papillary thyroid carcinoma (PTC) specimens and the presence of the BRAF mutation and clinicopathologic variables.
Methods
Fifty-six snap-frozen thyroid tumor samples, including those of 49 PTCs, four follicular adenomas, two follicular carcinomas, and one Hürthle cell adenoma, were studied. We performed reverse transcription-polymerase chain reaction (RT-PCR) to assess the OPN expression levels. We also tested the BRAF codon 599 mutations using RT-PCR with the direct sequencing method. All of the tumors were microscopically reexamined by a pathologist with a special interest in thyroid neoplasia.
Results
OPN mRNA was significantly overexpressed in the PTC samples compared with other thyroid tumors (P = 0.011). In PTCs, the OPN expression level was higher in the BRAF mutation group than in the wild-type group (P = 0.041). Among the clinicopathologic variables, nonfollicular variant histologic subtypes (P = 0.002) and the presence of lymph node metastases (P = 0.042) were correlated with elevated level of OPN expression.
Thyroid cancer is the most prevalent endocrine malignancy in humans [1], and the incidence of this type of cancer is rapidly increasing. The increase of thyroid cancer is so distinct in Korea that thyroid cancer has become the most common malignancy in Korean women according to a 2005 statistical report by the National Health Insurance Corporation of Korea. This is presumably due to the fact that papillary thyroid microcarcinoma is frequently detected as a result of the broad use of ultrasonography combined with fine needle aspiration cytology [2]. Consequently, the proportion of papillary thyroid carcinoma (PTC) among thyroid cancers is growing and is now an explanation for more than 90% of all thyroid cases.
Significant progress in the understanding of genetic events in PTC has been achieved over the past several decades. The RET proto-oncogene, which is rearranged during transfection, is located on chromosome 10q11.2 and was first isolated in 1985 and was shown to be activated by a DNA rearrangement [3]. RET encodes a single-pass transmembrane tyrosine kinase that functions as the receptor tyrosine kinase for the growth factors of the glial cell line-derived neurotropic factor family [4]. In PTC, genomic rearrangements juxtapose the RET kinase and COOH-terminus encoding domains to unrelated genes, which thereby creates dominantly transforming oncogenes called RET/PTC rearrangements [5]. RET/PTC1 and RET/PTC3 account for more than 90% of all rearrangements and are hence, by far, the most frequent variants [6,7]. These variants result from the fusion of RET to the coiled-coil domain containing gene 6 (CCDC6, formerly called H4/D10S170) or to the nuclear receptor coactivator gene 4 (NcoA4, formerly called RET fused gene/ELE1/ androgen receptor activator 70) [6,7].
A somatic point mutation in the BRAF gene has recently been identified as the most common genetic event in PTC [8]. The BRAF gene encodes a cytoplasmic serine/threonine kinase that is regulated by binding with RAS. Almost all of the BRAF point mutations found in PTC are a thymine-to-adenine transversion that occurs at nucleotide position 1796, which results in a valine-to-glutamate substitution at residue 599 (V599E) [9]. The V599E mutation is believed to mimic the phosphorylation in the activation segment as a result of the insertion of an acidic residue close to a site of regulated phosphorylation at serine 598 [10]. RAS point mutations are infrequent in PTC and are restricted to aggressive subtypes and to the follicular variant (FV) of PTC [11]. Despite the known linkage between these oncogenes and PTC, little is known about the molecular mechanisms that control the establishment, maintenance and progression of the PTC neoplastic phenotype.
Osteopontin (OPN), a secreted noncollagenous, sialicacid-rich, chemokine-like protein is recently receiving attention to give a clue to it. OPN is also known as a member of the small integrin binding ligand N-linked glycoprotein family with multifunctional properties in cell migration and cell survival. Previous researches have elucidated that OPN is up-regulated in a variety of cancers, such as breast, gastric, and colorectal cancers and in some highly metastatic cancer cell lines [12,13]. In a recent study, OPN was found to be overexpressed in human PTCs, and the prevalence and intensity of OPN staining were correlated with aggressive features [14], which suggests that OPN is one of the end products of the RET-RAS-BRAF-MAPK oncogenic cascade in PTCs. However, its direct correlation with somatic mutations was not examined.
This study was designed to evaluate the relationships between the degree of OPN expression in human PTC specimens, and the BRAF mutation and clinicopathologic variables. We expected it would serve practical hints on understanding of the RET-RAS-BRAF-MAPK linear signaling cascade of thyroid cancer cells.
Fifty-six snap-frozen thyroid tumor samples, including those of 49 PTCs, four follicular adenomas, two follicular carcinomas, and one Hurthle cell adenoma, were studied. All of the analyzed specimens were sampled from primary tumors treated surgically at the Department of Surgery of the Seoul National University Hospital in Korea. All of the specimens were snap-frozen immediately after collection and stored at -80℃ until use. Each patient signed an informed consent form prior to their surgical procedure, in which they approved the collection of fresh thyroid samples to be used for medical research. After the initial review of selected cases, all of the glass slides of these samples were microscopically reexamined by a pathologist with a special interest in thyroid neoplasia. PTC was subclassified as classic papillary carcinoma or as a distinct histologic variant [15] based on the following criteria: FV, more than two-thirds of the tumor has follicular architecture with no well-formed papillae found; tall cell variant, more than 50% of tumor cells are twice as tall as they are wide.
The clinicopathologic variables were recorded for all PTC cases, which included sex, age, tumor size, extra-thyroidal extension, encapsulation, multicentricity, regional lymph node metastasis, lymphatic invasion, distant metastasis, and background thyroiditis. Tumor staging was based on the recommendations of the sixth edition of the American Joint Committee on Cancer.
RNA extraction from the snap-frozen specimens was performed using Trizol reagent (Invitrogen, Carlsbad, CA, USA), according to the manufacturer's instructions. The quality of RNA was verified by electrophoresis through a 1.2% agarose gel with formaldehyde. Five micrograms of total RNA were used for the reverse transcription reactions. In detail, the RNA was incubated at 37℃ for 1 hour with superscript reverse transcriptase II (Invitrogen) using oligo dT primers in a total volume of 20 µL. The integrity of the RNA and efficiency of the RT reaction in each sample were confirmed using the housekeeping gene GAPDH for comparison purposes.
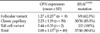
Specific primer pairs for the OPN gene were used to create gene-specific PCR amplicons using the reverse-transcribed product (Table 1). The levels of the housekeeping GAPDH gene transcript were used as a control to ensure that an equal amount of RNA was loaded. For each PCR reaction, 1 µL of reverse-transcribed mixture was amplified with 10 pmol of each primer, 200 µM deoxynucleotide triphosphates, 20 mM Tris-Cl (pH8.0), 100 mM KCl, 0.1 mM ethylenediaminetetraacetic acid, 1 mM dithiothreitol, 0.5% Tween 20, 0.5% Nonidet P-40, 50% glycerol, and 0.5 U of rTaq polymerase (TaKaRa) in a final volume of 20 µL. Forty cycles of denaturation (94℃ for 30 seconds), annealing (58℃ for 30 seconds), and extension (72℃ for 30 seconds) were conducted on an automated heat block (PTC-100, MJ Research, Watertown, MA, USA). Each RT-PCR product was loaded onto a 1.5% agarose gel stained with ethidium bromide (0.5 µg/mL). The image of the gel was saved, and the density and width of each band were quantified using the MyImager 1000 Image Analysis System (SeouLin Bioscience Co., Seongnam, Korea). The OPN mRNA expression level of each sample was recorded as the fold increase with respect to the expression of the housekeeping GAPDH gene.
The BRAF mutations that have been characterized so far are localized in two critical segments of the gene, namely exon 11 and exon 15. Almost all BRAF mutations in PTCs are detected at nucleotide 1796 of exon 15. Thus, all of the cDNAs were amplified via PCR using sets of primers that were designed to flank exons 15 of BRAF (Table 1). The PCR amplicon was amplified using 1 µL reverse-transcribed product in a reaction volume of 20 µL with 20 pmol of the specified primer pairs. The PCR products were purified using the QIAquick spin kit (QIAGEN, Valencia, CA, USA). Sequencing was performed with the ABI PRISM BigDyeTM Terminator Cycle Sequencing Ready Reaction Kit v3.1 (Applied Biosystems, Foster City, CA, USA), and the sequencing data were analyzed with the ABI 3130XL Genetic Analyzer.
The association of OPN mRNA expression with multiple variables was assessed using Student's t-test, one-way analysis of variance or nonparametric Kruskal-Wallis test according to each statistic condition. Spearman's correlation coefficient was calculated to evaluate the relationships of OPN expression in PTCs with N stage and the overall stage. Receiver operating characteristics (ROC) were performed in order to calculate the cut-off values of the OPN mRNA expression level according to the most accurate value obtained. Logistic regression analyses were conducted as a multivariate study to evaluate the associations between the OPN mRNA expression level or the presence of the BRAFV599E mutation and the clinicopathologic features of PTC patients. For comparisons of the prevalence of the examined variables in BRAFV599E mutation and BRAF wild-type subgroups, chi-square tests, Fisher's exact tests or linear-by-linear association tests were used. All of the data were analyzed using the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA).
We calculated the OPN mRNA expression level as the fold increase with respect to the expression of the housekeeping GAPDH gene (Fig. 1). OPN mRNA was significantly overexpressed in the PTCs, with respect to the other thyroid tumors including follicular adenomas, follicular carcinomas and Hurthle cell adenoma (P = 0.011) (Table 2). Since the OPN expression level of the Hürthle cell adenoma was exceptionally high, the OPN overexpression in PTCs was more obvious compared to follicular neoplasms alone (P = 0.002) (Table 2).
A pathologic review subdivided the PTCs into three histologic subtypes, classic papillary (n = 39), FV-PTC (n = 8), and tall cell variant PTC (n = 2). The mean OPN expression level of the FV-PTCs was markedly lower than that of the other subtypes (P = 0.024) (Table 3). The nonparametric Kruskal-Wallis test also showed that significant differences of OPN expression level exist among these three histologic subtypes (P = 0.002).
A search of BRAF mutations in PTCs showed the presence of a mutation of exon 15 in 37 of 46 PTCs (80.4%) (Table 3). All of the mutations observed were the same missense T to A transversion at nucleotide 1796, which results in the substitution of a valine to glutamate at residue 599 (Fig. 2). None of the seven non-PTC neoplasms had a mutation in exon 15. The frequency of the BRAFV599E mutation of each histologic PTC subtype, which all showed a tendency for similar influence on OPN expression, showed that FV-PTCs had the lowest frequency of the BRAFV599E mutation, but this was not statistically significant (P = 0.134).
Among the clinicopathologic variables studied, the absence of lymph node metastasis was significantly correlated with FV-PTC (not shown in table) (P = 0.006).
To disclose whether OPN expression has any relevance in PTC phenotypes, we compared OPN mRNA expression levels among the PTCs with different clinicopathologic features (Table 4). The mean OPN mRNA expression level was significantly higher in patients with lymph node metastasis (P = 0.042), those diagnosed as advanced N stage (P = 0.027), and those with BRAFV599E mutation (P = 0.027). To investigate the possible correlation of OPN expression and tumor progression, the OPN mRNA expression level was compared against T stage, N stage and overall stage. OPN expression was found to be positively correlated with N stage (P = 0.000, rs = 0.630) and overall stage (P = 0.035, rs = 0.306) using a Spearman's correlation coefficient. To control for possible confounding factors, logistic regression analysis was conducted as part of our multivariate study. We defined an elevated OPN expression level according to the proper predictive values calculated with the ROC analyses. As a result of the multivariate study, elevated expression level of OPN was associated with non-FV subtypes (P = 0.005), the BRAFV599E mutation (P = 0.033), and lymph node metastasis (P = 0.040).
Table 5 displays the clinicopathologic characteristics of the PTCs and the results of the comparisons of the prevalence of the examined variables according to the BRAFV599E mutation and BRAF wild type subgroups. Of all of the clinicopathologic features that were compared, female sex (P = 0.036, Fisher's exact test) and N stage (P = 0.044, linear-by-linear association test) were statistically associated with the BRAFV599E mutation. However, the multivariate study using logistic regression revealed that only pN1b had a borderline significant association with the presence of the BRAFV599E mutation (P = 0.101).
Ever since OPN was first identified in bone, its various roles have been intensely investigated. The results have elucidated the pivotal role of OPN in regulating the cell signaling that controls tumor progression and metastasis. OPN exerts biological effects by mainly binding two types of cell surface receptors, which are CD44v6 and av-containing integrins [16]. Integrin or CD44-bound OPN activates the phosphoinositide 3-kinase (PI3-K)-Akt signaling pathways in murine pro-B-cell cell lines [17], breast cancer cells [18], and prostate cancer cells [19]. Akt is a serine/threonine kinase and regulates cell cycle progression, growth-factor-mediated cell survival, cell migration and anchorage-independent growth of tumor cells [20]. When it comes to thyroid carcinoma, there have been two remarkable studies in regard to OPN. Castellone et al. [21] found that OPN was the most strongly upregulated gene (9.4-folds) in RET/PTC3-transformed follicular cells with respect to the parental cells by using an oligonucleotide microarray. They also demonstrated that RET/PTC3-transformed PC Cl 3 cells that were stimulated with exogenous recombinant OPN or transduced with a lentiviral vector for OPN have increased migration ability in Matrigel media, and that this ability is blocked by anti-OPN or -CD44 antibodies. Guarino et al. [14] showed that the presence of lymph node metastases and tumor size both positively correlated with OPN positivity in the immunohistochemical study of human thyroid tumor samples. They also revealed that OPN and its selective cell surface receptor CD44v6 are up-regulated in a panel of PTC cell lines that are characterized for the presence of RET/PTC rearrangements or the BRAFV599E mutation.
Using RT-PCR of fresh-frozen tissue of thyroid tumors, we identified in this study that PTC shows high OPN expression compared with other thyroid tumors, and that it is especially accentuated in non-FV, BRAFV599E mutation, and lymph node metastasis subgroups. This is a special finding since there have only been few studies on OPN in human PTC specimens.
We confirmed high OPN expression in PTC as in other studies, but interestingly, a Hürthle cell adenoma showed very high OPN expression. There has been no reported data regarding OPN expression in Hurthle cell adenomas. Although one specimen's result has little significance, we can infer that the disruptive mutations of mitochondrial DNA that is reported to be present in 26% of all Hurthle cell tumors [22] may have some role in the OPN expression that was observed in our study.
Our data demonstrate that FV-PTC is negatively correlated with OPN expression, and this is identical to the results of a previous study [14]. On the molecular level, FV-PTC is characterized by a high prevalence of RAS mutations and a low prevalence of RET/PTC rearrangement or the BRAF mutation [11,23]. In two large series of FV-PTC, a significantly higher frequency of total or partial encapsulation and a lower rate of lymph node metastases were found in FV tumors in comparison with classic papillary carcinomas, and the prognosis of this type of cancer is similar to or better than those of classic PTCs [24,25]. In the present study, we could not identify a significant tendency of encapsulation in FV-PTC, and this may be due to the small sample number of FV-PTC cases; however, FV-PTCs were significantly correlated with low level of OPN expression and the absence of lymph node metastasis. These results support that the prognoses of FV-PTCs are better than those of classic or other subtypes of PTCs even though we did not compare the prognoses directly.
The RAS-RAF-MAP kinase pathway is an important signaling pathway in human cancers and mediates cellular responses to growth signals. The RET/PTC-RAS-BRAF-MAPK pathway is specific to thyroid follicular cell origin carcinoma. No overlap was observed between papillary carcinomas harboring BRAF, RAS, and RET/PTC mutations [8], which is consistent with the notion that each mutation acts along the RET/PTC-RAS-BRAF-MAPK pathway in thyroid cells, and that any one of these intermediate mutations can potentially initiate PTCs. Although this linear signaling pathway is believed to play a key role in the initiation and progression of PTC, there is marked phenotypic variability of PTC according to the harbored somatic mutations. For instance, Giordano et al. [23] have reported that the microarray analysis of 51 PTCs showed that tumors with BRAF mutations displayed either tall cell variant or classic papillary morphology, tumors with RET/PTC rearrangements predominantly displayed the classic papillary morphology and tumors with RAS mutations exclusively displayed the FV morphology. These close correlations between phenotypes and genotypes indicate that each somatic mutation has its own distinct pattern of abnormal gene expression that can trigger specific signals in addition to the common ones along the linear signaling pathway. Of these intermediate mutations, the BRAF mutation is the most common somatic mutation in PTCs, and its prevalence was reported as 29 to 69% [26]. This is especially important in Korea since the prevalence of PTCs is very high (83%) in Koreans [27]. A high prevalence of the BRAF mutation in PTCs (80.4%) was observed in our study, and all identified BRAF exon 15 mutations in the present study were BRAFV599E, which is similar to the findings of previous studies. There has been controversy regarding the significance of the BRAF mutation as a prognostic factor, but recent studies with relatively large sample sizes support that the BRAF mutation is associated with poorer clinicopathological outcomes [28] and independently predicts recurrence [29]. We observed, in the present study, a significant association between the BRAF mutation and advanced N stage, but did not find association between the BRAF mutation and any other aggressive feature of PTC. This is probably due to the high prevalence of the BRAF mutation in our study.
We also showed that the OPN mRNA expression level was significantly high in human PTC specimens with the BRAFV599E mutation and aggressive clinicopathologic features. This result suggests that OPN can be a common product of the RET/PTC-RAS-BRAF-MAPK pathway or a result of the BRAF mutation, and that it plays a pivotal role in tumor progression and metastasis of PTC cells. This finding is also in concordance with the reports that OPN bound with integrin or CD44 activates the PI3-K-Akt signaling pathways, and increased Akt stimulates cell survival and migration in other types of cancer cells [17-19]. We emphasize that the illustrated correlation between OPN mRNA expression level and BRAF mutation will have importance in geographic areas where the prevalence of BRAF mutation in PTCs is relatively high, like in Korea, and that, if a better understanding of OPN can be achieved in future studies, then OPN might be used as a useful diagnostic tumor maker and therapeutic target of PTCs.
In conclusion, OPN is overexpressed in PTCs with BRAF mutations, aggressive histologic subtypes, and lymph node metastasis, and this indicates that it plays a crucial role in tumorigenesis and the progression of PTC.
Figures and Tables
Fig. 1
Osteopontin (OPN) expression according to histologic type. Each product of reverse transcription-polymerase chain reaction of OPN mRNA was loaded onto a 1.5% agarose gel that was stained with ethidium bromide (0.5 µg/mL). MyImager 1000 Image Analysis System was used for the quantification of each band. OPN mRNA expression of each sample was recorded as the fold increase with respect to the expression of the housekeeping GAPDH gene. CP, classic papillary type of papillary thyroid carcinoma; FV, follicular variant of papillary thyroid carcinoma; FA, follicular adenoma.

Fig. 2
Sequence chromatograms of BRAF exon 15 wild-type and mutant type of PTC BRAF mutation-positive sample (mutant type) shows the heterogeneous thymine-to-adenine transversion at nucleotide position 1796, which results in a valine-to-glutamate substitution at residue 599. All of the detected BRAF mutations in this study were these BRAFV599E mutations.

References
1. DeLellis RA, Williams ED. DeLellis LA, Lloyd RV, Heitz PU, Eng C, editors. Thyroid and parathyroid tumors. Pathology and genetics of tumours of endocrine organs. 2004. Lyon: IARC Press;51–56.
2. Pelizzo MR, Boschin IM, Toniato A, Pagetta C, Piotto A, Bernante P, et al. Natural history, diagnosis, treatment and outcome of papillary thyroid microcarcinoma (PTMC): a mono-institutional 12-year experience. Nucl Med Commun. 2004. 25:547–552.
3. Takahashi M, Ritz J, Cooper GM. Activation of a novel human transforming gene, ret, by DNA rearrangement. Cell. 1985. 42:581–588.
4. Airaksinen MS, Saarma M. The GDNF family: signalling, biological functions and therapeutic value. Nat Rev Neurosci. 2002. 3:383–394.
5. Grieco M, Santoro M, Berlingieri MT, Melillo RM, Donghi R, Bongarzone I, et al. PTC is a novel rearranged form of the ret proto-oncogene and is frequently detected in vivo in human thyroid papillary carcinomas. Cell. 1990. 60:557–563.
6. Tallini G, Asa SL. RET oncogene activation in papillary thyroid carcinoma. Adv Anat Pathol. 2001. 8:345–354.
7. Kondo T, Ezzat S, Asa SL. Pathogenetic mechanisms in thyroid follicular-cell neoplasia. Nat Rev Cancer. 2006. 6:292–306.
8. Kimura ET, Nikiforova MN, Zhu Z, Knauf JA, Nikiforov YE, Fagin JA. High prevalence of BRAF mutations in thyroid cancer: genetic evidence for constitutive activation of the RET/PTC-RAS-BRAF signaling pathway in papillary thyroid carcinoma. Cancer Res. 2003. 63:1454–1457.
9. Cohen Y, Xing M, Mambo E, Guo Z, Wu G, Trink B, et al. BRAF mutation in papillary thyroid carcinoma. J Natl Cancer Inst. 2003. 95:625–627.
10. Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, et al. Mutations of the BRAF gene in human cancer. Nature. 2002. 417:949–954.
11. Zhu Z, Gandhi M, Nikiforova MN, Fischer AH, Nikiforov YE. Molecular profile and clinical-pathologic features of the follicular variant of papillary thyroid carcinoma: an unusually high prevalence of ras mutations. Am J Clin Pathol. 2003. 120:71–77.
12. Weber GF. The metastasis gene osteopontin: a candidate target for cancer therapy. Biochim Biophys Acta. 2001. 1552:61–85.
13. Rudland PS, Platt-Higgins A, El-Tanani M, De Silva, Barraclough R, Winstanley JH, et al. Prognostic significance of the metastasis-associated protein osteopontin in human breast cancer. Cancer Res. 2002. 62:3417–3427.
14. Guarino V, Faviana P, Salvatore G, Castellone MD, Cirafici AM, De Falco V, et al. Osteopontin is overexpressed in human papillary thyroid carcinomas and enhances thyroid carcinoma cell invasiveness. J Clin Endocrinol Metab. 2005. 90:5270–5278.
15. Livolsi VA. Surgical pathology of the thyroid. Philadelphia: Saunders;1990.
16. Rangaswami H, Bulbule A, Kundu GC. Osteopontin: role in cell signaling and cancer progression. Trends Cell Biol. 2006. 16:79–87.
17. Lin YH, Yang-Yen HF. The osteopontin-CD44 survival signal involves activation of the phosphatidylinositol 3-kinase/Akt signaling pathway. J Biol Chem. 2001. 276:46024–46030.
18. Das R, Mahabeleshwar GH, Kundu GC. Osteopontin stimulates cell motility and nuclear factor kappaB-mediated secretion of urokinase type plasminogen activator through phosphatidylinositol 3-kinase/Akt signaling pathways in breast cancer cells. J Biol Chem. 2003. 278:28593–28606.
19. Zheng DQ, Woodard AS, Tallini G, Languino LR. Substrate specificity of alpha(v)beta(3) integrin-mediated cell migration and phosphatidylinositol 3-kinase/AKT pathway activation. J Biol Chem. 2000. 275:24565–24574.
20. Nicholson KM, Anderson NG. The protein kinase B/Akt signalling pathway in human malignancy. Cell Signal. 2002. 14:381–395.
21. Castellone MD, Celetti A, Guarino V, Cirafici AM, Basolo F, Giannini R, et al. Autocrine stimulation by osteopontin plays a pivotal role in the expression of the mitogenic and invasive phenotype of RET/PTC-transformed thyroid cells. Oncogene. 2004. 23:2188–2196.
22. Gasparre G, Porcelli AM, Bonora E, Pennisi LF, Toller M, Iommarini L, et al. Disruptive mitochondrial DNA mutations in complex I subunits are markers of oncocytic phenotype in thyroid tumors. Proc Natl Acad Sci U S A. 2007. 104:9001–9006.
23. Giordano TJ, Kuick R, Thomas DG, Misek DE, Vinco M, Sanders D, et al. Molecular classification of papillary thyroid carcinoma: distinct BRAF, RAS, and RET/PTC mutation-specific gene expression profiles discovered by DNA microarray analysis. Oncogene. 2005. 24:6646–6656.
24. Tielens ET, Sherman SI, Hruban RH, Ladenson PW. Follicular variant of papillary thyroid carcinoma. A clinicopathologic study. Cancer. 1994. 73:424–431.
25. Jain M, Khan A, Patwardhan N, Reale F, Safran M. Follicular variant of papillary thyroid carcinoma: a comparative study of histopathologic features and cytology results in 141 patients. Endocr Pract. 2001. 7:79–84.
26. Puxeddu E, Moretti S, Elisei R, Romei C, Pascucci R, Martinelli M, et al. BRAF(V599E) mutation is the leading genetic event in adult sporadic papillary thyroid carcinomas. J Clin Endocrinol Metab. 2004. 89:2414–2420.
27. Kim KH, Kang DW, Kim SH, Seong IO, Kang DY. Mutations of the BRAF gene in papillary thyroid carcinoma in a Korean population. Yonsei Med J. 2004. 45:818–821.
28. Nikiforova MN, Kimura ET, Gandhi M, Biddinger PW, Knauf JA, Basolo F, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab. 2003. 88:5399–5404.
29. Xing M, Westra WH, Tufano RP, Cohen Y, Rosenbaum E, Rhoden KJ, et al. BRAF mutation predicts a poorer clinical prognosis for papillary thyroid cancer. J Clin Endocrinol Metab. 2005. 90:6373–6379.




 ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download