Abstract
Purpose
The objective of this study was to survey potential candidates for bariatric/metabolic surgery for procedure preferences.
Methods
Questions asked were divided into 5 categories: (1) demographic and anthropometric data, comorbidities, and favored surgery; (2) awareness of safety, effectiveness, and complications of each type of surgery; (3) discordances in opinion between self-selected and medically recommended procedures; and (4, 5) reasons for/against particular surgery.
Results
From 1 October to 15 November 2018, 104 respondents adequately responded and were included in the analysis. The number (%) of female respondents was 79 (76.0%). The number (%) of respondents by decade was 17 (16.3%) in their 20s, 65 (62.5%) in their 30s, 19 (18.3%) in their 40s, and 3 (2.9%) in their 60s, respectively. Mean body mass index was 37.1 ± 6.3 kg/m2. Comorbidities were type 2 diabetes in 34 (32.7%) and hypertension in 35 (33.7%). The most favored procedure was sleeve gastrectomy (SG) in 78 (75.0%), adjustable gastric band (AGB) surgery in 12 (11.5%), Roux-en-Y gastric bypass (RYGB) in 6 (5.8%), and gastric plication (GP) in 8 (7.7%). Major reasons for choosing procedures were; “adjustable” for AGB, “stomach sparing” for GP, “excellent weight loss” for SG, and “comorbidity resolution” in RYGB.
Obesity has reached epidemic proportions worldwide, mainly because of high caloric consumptions and sedentary lifestyles. Over 1.5 billion adults aged 20 years and older are now considered overweight or obese [1]. Metabolic disorders such as type 2 diabetes, hypertension, and nonalcoholic fatty liver disease have also increased remarkably, and this disturbing trend has also been reported in Asian countries. According to the Korea National Health and Nutritional Examination Survey conducted in 2016, the prevalence of obesity in Korea had then increased to 42.3% for men and 26.4% for women. Bariatric surgical procedures are known to achieve substantial weight loss and provide major secondary health benefits. Bariatric procedures are classified as restrictive (adjustable gastric band [AGB], sleeve gastrectomy [SG]) or hypoabsorptive (gastric bypass, duodenal switch). In addition, gastric plication [GP] is an emerging procedure in some countries, although its efficacy and safety have yet to be confirmed [2]. A recent worldwide survey revealed that the most performed primary surgical bariatric/metabolic procedure is SG (53.6%), followed by Roux-en-Y gastric bypass (RYGB; 30.1%) and one anastomosis gastric bypass (4.8%) [3]. The bariatric population is extremely heterogeneous, and it is impractical to assume that any single bariatric procedure would succeed in all patients. Furthermore, each procedure has its unique advantages and disadvantages, which makes procedure choice for individual patients difficult. In a previous study, candidates for bariatric surgery considered cost, expected weight loss, and resolution of medical conditions the most important characteristics of weight loss surgery decisions [4]. However, little is known as to why patients undergo one bariatric procedure rather than another. Furthermore, to our knowledge, no study has assessed attitudes toward choice of weight loss surgery in presurgical candidates. Accordingly, we designed an online cross-sectional survey to assess these attitudes using Google Forms.
This study was a cross-sectional survey of candidates for bariatric/metabolic surgery. Questionnaires were completed anonymously without and any completion incentive. The questions addressed 5 categories, namely, (1) demographic and anthropometric data, comorbidities, reason for considering surgery, and current most favorite surgery; (2) awareness of safety, effectiveness (weight loss and resolution of comorbidities), and the complications of each type of surgery; (3) discordances in opinion about surgery between the patient and that recommended medically; (4) reasons for favoring a particular surgery; (5) reasons for disliking a particular surgery. Questions were asked of participants via a link with Google Forms (https://docs.google.com/forms/d/12HzNVXxNNqLnpt4vSyZVKZw0yqlhpi1qV3VNUZqn3js/edit?usp=sharing), which was uploaded to the online patient com munity or the homepage of our hospital.
Mean Likert scale scores (LSSs) for patient awareness were analyzed and compared. The survey question sheet was hyperlinked to a colorful animation scene and uploaded to our hospital's homepage (https://cafe.naver.com/barisurg) and to a patient community web site. Clicking to participate in the survey confirmed consent to participate. The study sample size (N) was determined using a 95% confidence level (z = 1.96), a 10% margin of error (E = 0.1), and a population proportion of 50% (P = 0.5). Ninety-seven or more samples were required (N = z2P(1 − P)/E2; z = z-score, P = population proportion, E = margin of error or confidence interval). Data were analyzed using SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as means ± standard deviations (SDs) and were compared using 1-way analysis of variance for independent samples, whereas categorical variables are presented as percentages (%). Categorical variables were compared using Pearson chi-square or Fisher exact test, as appropriate. All tests were 2-tailed, and statistical significance was accepted for P-values of < 0.05. Results are presented as means ± SDs or as numbers (%), as indicated. Written informed consent was obtained from all participants. The study was approved beforehand by Institutional Review Board of Gachon University Gil Medical Center (GCIRB2019-171).
From 1 October to 15 November 2018, a total of 120 respondents submitted the Survey form. Sixty-eight (57%) responses were received on the first day, 104 (87%) within 14 days, and 120 within 45 days. Of these 120 initial respondents, 104 responded adequately and were included in the analysis.
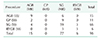
Of the 104 respondents 25 (24.0%) were male and 79 (76.0%) were female. Numbers (%) of respondents by decade were; 17 (16.3%) in their 20s, 65 (62.5%) in their 30s, 19 (18.3%) in their 40s, and 3 (2.9%) in their 60s, respectively. The mean ± SD (range) of the height, weight, and body mass index (BMI) of the respondents were 165.3 ± 7.2 cm (150.0–182.0 cm), 101.6 ± 20.2 kg (75.0–185.0 kg), and 37.1 ± 6.3 kg/m2 (31.2–64.0 kg/m2), respectively. Comorbidities of respondents were type 2 diabetes in 34 (32.7%), hypertension in 35 (33.7%), fatty liver disease in 28 (26.9%), hyperlipidemia in 28 (26.9%), dysmenorrhea in 33 (33/79, 41.8%), gastroesophageal reflux in 26 (25.0%), arthritis/arthralgia in 27 (26.0%), and a neuro-psychiatric problem in 15 (14.4%). Reasons for considering surgery were “to achieve substantial weight loss” in 75 (72.1%), “to cure comorbidities” in 69 (66.3%), “to prevent adult diseases” in 29 (27.9%), and “to achieve modest weight loss/diet” in 22 (21.2%). SG was favored by 78 respondents (75.0%), AGB surgery by 12 (11.5%), RYGB surgery by 6 (5.8%), and GP surgery by 8 (7.7%). Twenty-one (18.6%) respondents had family/friends/acquaintances that had undergone surgery; AGB in 13 (11.5%) and SG in 8 (7.1%) (Table 1).
Mean LSS scores (5, very high; 4, high; 3, intermediate; 2, low; and 1, very low) for awareness of the safeties of AGB, GP, SG, and RYGP were 3.5 ± 1.1, 3.3 ± 0.8, 3.6 ± 0.8, and 3.3 ± 0.8, respectively (P = 0.016). Mean LSS scores for awareness of weight loss effects of each procedure were 3.3 ± 0.8, 3.4 ± 0.7, 4.4 ± 0.6, and 4.2 ± 0.8, respectively (P < 0.001), and for awareness of the effects of each procedure in terms of curing comorbidities were 3.1 ± 0.8, 3.3 ± 0.8, 4.2 ± 0.6, and 4.4 ± 0.6 respectively (P < 0.001). Mean LSS scores for awareness of procedural complication rates were 3.6 ± 0.9, 3.2 ± 0.5, 3.2 ± 0.9, and 3.3 ± 0.8, respectively (P < 0.001). Thus, SG was the safest and most effective weight loss procedure that people thought, and RYGB was the best procedure resulting in comorbidity resolution. On the contrary, AGB was the procedure that most related to complication (Table 2, Fig. 1).
Ninety-eight of the 104 respondents underwent medical consultation to select an appropriate procedure. Seventy-one (72.4%) indicated that the self-selected (SS) procedure was the same as the medically recommended (MR) procedure. For the remaining 27 (27.8%), the SS and MR procedures differed (Table 3). Eight respondents favored GP after consultation, but had been recommended either AGB (n = 2) or SG (n = 6) during medical consultation. Of the 78 respondents that favored SG after consultation, 19 reported that the SS and MR procedures differed. Twelve respondents changed their favored SS procedure after consultation (AGB to SG in 6, GP to SG in 3, and RYGB to SG in 3). On the other hand, 7 respondents insisted on SS procedures after medical consultation (AGB was recommended for 4 and RYGB for 3) (Table 4).
Subjective questions regarding reasons for chosen procedures showed that major reasons for AGB were “adjustable” (n = 8), “reversible” (n = 1), and “small meal size” (n = 1); for GP were “stomach sparing” (n = 2) and “high food tolerance” (n = 2); for SG were “excellent weight loss” (n = 19), “fewer follow-up visits” (n = 16), and a “small stomach” (n = 10); for RYGB were “comorbidity resolution” (n = 2), “smaller meals” (n = 1), and “safety” (n = 1). The major reasons for not choosing AGB were “concern of long-term complications” (n = 28), “frequent follow-up visits” (n = 16), and “ineffectiveness” (n = 9); for GP were “stomach dilatation” (n = 25), “no information” (n = 21), and “concern of complications” (n = 8); for SG, “stomach resection” (n = 9), “stomach dilatation” (n = 6), and “concern of possible leakage” (n = 5); and for RYGB “procedural complexity” (n = 22), “concern of complications” (n = 19), and “No information” (n = 15) (Table 5).
It has been suggested that SS bariatric procedures provide excellent weight loss and metabolic outcomes [5]. In addition to surgeons' influences, patients demonstrate clear procedural preferences based on their own research, knowledge, and experiences [6]. In this survey, the most favored procedure among respondents was SG (75.0%), followed AGB (11.5%), GP (7.7%), and gastric bypass (5.8%). According to LSS in our study, respondents favored SG due to its safety and effectiveness, which is in-line with the conclusion of a previous study, in which safety and invasiveness were found to have greatest impact on patient bariatric choice [7].
However, these responses are quite different from those published in early 2010, when AGB was the dominating procedure [3]. At that time, AGB was more frequently performed than RYGB due to its safety and equal long-term weight loss, and SG was in its infancy. As a result, candidates for bariatric surgery chose AGB rather than RYGB or SG because AGB appealed to patients and surgeons due to adjustability, reversibility, and no need to alter gastrointestinal tract anatomy or invasive gastric stapling or partitioning [89]. However, in our survey AGB was not favored by many candidates due to long-term complications (n = 28), frequent follow-up visits (n = 16), ineffectiveness (n = 9), foreign body placement (n = 8), device explantation (n = 5), and frequent vomiting (n = 2). The reason for a changing pattern toward AGB is likely to be multifactorial and include the introduction and increasing use of SG for the treatment of morbid obesity and specific complications (e.g., slippage, erosion, and intolerance) associated with AGB. Furthermore, the death of a famous person after AGB was well publicized in 2013 and 2014 in our country, and previously the rate of AGB implantation was far greater than those of SG or RYGB. Overall, the better outcomes achieved by SG in terms of weight loss and morbidity, have contributed to its popularity and accelerated the decline in the popularity of AGB over recent years. Our survey also showed that SG was the safest and most effective weight loss procedure, and RYGB was the best procedure resulting in comorbidity resolution. On the contrary, AGB was the procedure that most related to complication.
In this survey, only 5.8% of the respondents favored RYGB, which was lower than expected. The major reason for favoring RYGB was resolution of comorbidities, which is compatible with the current evidence-based clinical data [101112]. However there several reasons were given for not favoring RYGB, namely, complex procedure (n = 22), concern for complications (n = 19), no information (n = 15), EGD not possible (n = 11), and concerns regarding long-term nutritional imbalance (n = 6). Thus, although RYGB remains the gold standard bariatric procedure, candidates for bariatric surgery in the present study did not favor RYGB as a primary procedure. Furthermore, setting patient perspectives aside, recent randomized clinical trials failed to document the superiority of RYGB over SG [1314]. Notably, in a recent worldwide survey by International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO), RYGB was found to have slipped to third place in the Asia/Pacific region after SG and one anastomosis gastric bypass [3].
GP is characterized by a reduction in total gastric volume through reversible plication of the greater curvature without the need for resection or costly stapling devices. In our country, the first case of GP was performed in 2013 [15]. Its advantages include no stapling or rerouting of the GI tract, minimal fistula formation, no requirement for foreign body implantation, and potential reversibility [16], which appeals to both patient and surgeon. However, technical difficulty and limited long-term follow-up data, especially with respect to weight regain, are obstacles that remain to be overcome before GP becomes a generally accepted procedure. In the present study, GP was favored only in 7.7%, and the reasons given were stomach dilatation (n = 25), no information (n = 21), and complications (n = 8), thus respondents appeared to be primarily concerned about weight regain following gastric dilatation. Minor reasons included experimental nature (n = 5), long recovery time (n = 3), and concerns regarding cancer screening (n = 1).
In our survey, the one reason for choosing GP was its “stomach sparing” nature; this indicates the need for further discussion with patients because stomach sparing appears to intuitively contradict the rationale regarding the long-term efficacy of restrictive surgery. Of the 8 respondents that favored GP, 2 were recommended AGB and 6 were recommended SG during medical consultations, which suggests potential patients for GP are more prone to resistant medical recommendations. This observation presents a dilemma for surgeons during procedure selection because postoperative compliance might be suboptimal in patients that favor GP, but undergo another restrictive procedure such as AGB or SG, based on medical advice. It has been suggested patients tend to have confidence in and are more comfortable with a favored procedure, and therefore, tend to be unwilling to undergo another procedure [17]. However, it is our opinion that the effectiveness of GP is suspect in patients with a BMI > 40 kg/m2 or moderate to severe metabolic disease (e.g., type 2 diabetes). One of the merits of GP is the cost of the procedure, but in our country, GP will be covered by public health insurance from 2019, and thus, the economic advantage of GP will be no longer an issue. Notably, no respondent in our survey favored GP for economic reasons. It should be clearly stated to patients that the stomach-sparing tradeoff offered by GP may result in early loss of restriction, accompanying dilatation, and weight regain.
As we expected, a gap was found between SS and MR procedures. Actually, SS and MR procedures differed in 27.8% (27 of 98) of the respondents that completed medical consultation. In detail, 8 respondents that favored GP after consultation were recommended to undergo either AGB (n = 2) or SG (n = 6) during consultation, and of 78 respondents whose favored procedure after consultation was SG, 19 respondents favored a procedure not recommended during consultation. Twelve respondents changed their SS procedure after consultation (AGB to SG in 6, GP to SG in 3, and RYGB to SG in 3), whereas 7 respondents insisted on their SS procedures (SG) after consultation (AGB was recommended in 4 and RYGB recommended in 3), thus it appears from our study that SG has become the procedure most favored by surgeons and patients. Regarding RYGB, SG was favored by respondents when SS and MR procedures differed.
The use of free Google Forms allowed us to easily obtain a sample size sufficient to answer the research questions, substantially reduced research expenses, because there were no data entry costs, and allowed us to effortlessly collect and enter data in Excel. We also found the potential candidate survey return rate was high and that completed forms were received in a relatively short time. However, the study has several limitations that warrant mention. Although we were blind to respondent information in terms of sources of medical consultation, it is unlikely that all medical consultations were conducted at hospitals that practice all 4 procedures, and this may have affected relative rates of MR procedures. Second, as the survey was online based, the respondents were all probably internet users, and thus, the web was probably the main source of information about surgery, as it is known to play an important role in the decision-making process of candidates for bariatric surgery [18]. Therefore, our results are based on the opinions of patients arrived at after internet searches. Lastly, the results of our survey concern patients' perspectives, and thus, may not be in-line with current medical science. However, we feel survey results were not quite different from the current medical consensus for each procedure. More sophisticate survey with experts might show the recognition match or difference with the candidates. In conclusion, candidates for bariatric/metabolic surgery were found to favor SG followed in order by AGB, RYGB, and GP. Patients provided clear reasons about their procedural preferences based on personal research, knowledge, and experience, and these preferences were compatible with current evidence-based clinical data. Based on the results of this survey and those of recent randomized controlled trials and the trends observed in the IFSO survey, we foresee that SG will continue to be a dominating procedure in our country.
Figures and Tables
Fig. 1
Mean Likert scale scores of awareness of safety, awareness of effect on weight loss, awareness of curing comorbidities, and awareness of complications in each procedure. AGB, adjustable gastric band; GP, gastric plication; SG, sleeve gastrectomy; RYGB, Roux-en-Y gastric bypass. *P = 0.046 (SG vs. GP), **P < 0.001 (SG vs. AGB or GP), ***P < 0.001 (AGB vs. GP or SG) or P = 0.021 (AGB vs. RYGB).

Table 1
Demographic and anthropometric data, comorbidities, reasons for considering surgery, and the procedure most favored by the 104 respondents

Values are presented as number (%) or mean ± standard deviation (range).
NAFLD, nonalcoholic fatty liver disease; GERD, gastroesophageal reflux disease; SG, sleeve gastrectomy; AGB, adjustable gastric band; RYGB, Roux-en-Y gastric bypass; GP, gastric plication.
a)Patient had more than one comorbidities. b)Respondents were allowed to choose more than one item.
References
2. Perivoliotis K, Sioka E, Katsogridaki G, Zacharoulis D. Laparoscopic gastric plication versus laparoscopic sleeve gastrectomy: an up-to-date systematic review and meta-analysis. J Obes. 2018; 2018:3617458.

3. Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, et al. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018; 28:3783–3794.


4. Rozier MD, Ghaferi AA, Rose A, Simon NJ, Birkmeyer N, Prosser LA. Patient preferences for bariatric surgery: findings from a survey using discrete choice experiment methodology. JAMA Surg. 2019; 154:e184375.

5. Vasas P, Nehemiah S, Hussain A, Finney J, Kirk K, Yeluri S, et al. Influence of patient choice on outcome of bariatric surgery. Obes Surg. 2018; 28:483–488.


6. Opozda M, Wittert G, Chur-Hansen A. Patients' reasons for and against undergoing Roux-en-Y gastric bypass, adjustable gastric banding, and vertical sleeve gastrectomy. Surg Obes Relat Dis. 2017; 13:1887–1896.


7. Ren CJ, Cabrera I, Rajaram K, Fielding GA. Factors influencing patient choice for bariatric operation. Obes Surg. 2005; 15:202–206.


8. Favretti F, Cadiere GB, Segato G, Bruyns G, De Marchi F, Himpens J, et al. Laparoscopic placement of adjustable silicone gastric banding: early experience. Obes Surg. 1995; 5:71–73.


9. Favretti F, Cadiere GB, Segato G, Bruyns G, De Marchi F, Himpens J, et al. Laparoscopic adjustable silicone gastric banding: technique and results. Obes Surg. 1995; 5:364–371.


10. Lee JH, Nguyen QN, Le QA. Comparative effectiveness of 3 bariatric surgery procedures: Roux-en-Y gastric bypass, laparoscopic adjustable gastric band, and sleeve gastrectomy. Surg Obes Relat Dis. 2016; 12:997–1002.


11. Shoar S, Saber AA. Long-term and midterm outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass: a systematic review and meta-analysis of comparative studies. Surg Obes Relat Dis. 2017; 13:170–180.


12. Li JF, Lai DD, Lin ZH, Jiang TY, Zhang AM, Dai JF. Comparison of the long-term results of Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis of randomized and nonrandomized trials. Surg Laparosc Endosc Percutan Tech. 2014; 24:1–11.

13. Peterli R, Wolnerhanssen BK, Peters T, Vetter D, Kroll D, Borbely Y, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018; 319:255–265.


14. Salminen P, Helmio M, Ovaska J, Juuti A, Leivonen M, Peromaa-Haavisto P, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. JAMA. 2018; 319:241–254.


15. Kim SB, Kim KK, Chung JW, Kim SM. Initial experiences of laparoscopic gastric greater curvature plication in Korea-a review of 64 cases. J Laparoendosc Adv Surg Tech A. 2015; 25:793–799.


16. Park YH, Kim SM. Short-term outcomes of laparoscopic greater curvature plication and laparoscopic sleeve gastrectomy in patients with a body mass index of 30 to 35 kg/m2. Yonsei Med J. 2017; 58:1025–1030.






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download