Abstract
Purpose
Traumatic lumbar hernia is rare, thus making diagnosis and proper treatment challenging. Accordingly, we aimed to investigate the clinical manifestations and proper management strategies of traumatic lumbar hernias.
Methods
The medical records of patients with traumatic lumbar hernia treated at Gachon University Gil Hospital from March 2006 to February 2015, were retrospectively reviewed.
Results
We included 5 men and 4 women (mean age, 55 years; range, 23–71 years). In 8 patients, most injuries were caused by motor vehicle collisions, including those wherein a pedestrian was struck (5 cases of car accidents, 2 falls, and 1 involving penetrating materials); in 1 patient, the probable cause was severe cough. Eight patients underwent hernia repair surgery (5 open and 3 laparoscopic), and a prosthetic mesh was used in 7 patients. Hernia repairs were elective in 7 patients; emergency hernia repair was performed with right hemicolectomy in 1 patient. No severe complication or recurrence was observed. Only 2 patients had mild complications, such as postoperative seroma.
Conclusion
Traumatic lumbar hernia is a relatively rare injury of the posteriolateral abdominal wall. Lumbar hernia should be suspected in patients with high-energy injuries of the torso, and all such patients should undergo abdominopelvic computed tomography. After diagnosis, hernia repair can be electively performed without complications in most cases.
Lumbar hernias are uncommon defects of the posteriolateral abdominal wall. To date, approximately 300 cases have been reported in the English literature [1]. Lumbar hernias can be congenital (20%) or acquired (80%) (primary or secondary) [23]. The primary types account for 55%, and secondary types, which are related to trauma, surgery, and infection, account for 25% [2]. Traumatic lumbar hernias are particularly rare among lumbar hernias. According to Burt et al. [2], only 66 cases, including their own 3 cases, have been reported in the English literature. Consequently, when surgeons encounter lumbar hernias in emergency situations, proper diagnosis and treatment can be challenging. In this study, we investigated clinical manifestations and proper management for traumatic lumbar hernias.
Nine patients with traumatic lumbar hernias were referred to Gachon University Gil Hospital from March 2006 to February 2015. We retrospectively reviewed the patients' medical records for epidemiological data, injury mechanism, diagnosis, imaging findings, treatment plan, operation methods, and outcomes. We descriptively analyzed the data because the number of patients with traumatic hernia was insufficient to obtain statistically significant results.
Ethical approval was obtained from Institutional Review Board of Gachon University Gil Medical Center (approval number: GAIRB2018-050).
The study included 5 men and 4 women, with a mean age of 55 years (range, 23–71 years). The height of the patients ranged from 147 cm to 170 cm (mean, 162 cm), and the weight ranged from 52 kg to 73 kg (mean, 60 kg).
All lumbar hernias were of traumatic origin; hence, they were classified as secondary lumbar hernias. However, 1 patient had a debatable etiology because he had symptoms of lumbar hernia after a severe cough due to vocal cord cancer. This patient also had a rib fracture. We ruled out other possible causes and speculated that the severe cough may have caused the hernia and rib fracture. However, whether the cough can provide a sufficient external force to cause a lumbar hernia is controversial. The other eight patients were injured by a high-energy external force. Five patients were injured during car accidents, 2 by falls, and 1 by penetrating materials (Table 1).
All patients underwent abdominopelvic CT scanning at the Emergency Department, except for 1 patient with a palpable mass after severe coughing (Fig. 1). Eight patients were immediately diagnosed with lumbar hernia (Table 2). Because our patients had other injuries due to trauma, CT scanning was essential for diagnosis. However, hernia repair was not immediately performed after diagnosis in contrast with other injuries, such as bowel perforation or traumatic subarachnoid hemorrhage, which were treated first. The hernia repairs were performed electively in 7 patients after acute-phase surgery had been completed.
Five patients had intra-abdominal organ injuries; 4 of these were bowel perforations that needed emergency laparotomy, and the other was a right kidney laceration (Table 1). Of 4 patients with bowel perforation, 3 underwent hernia repair 97 days, 141 days, and 273 days after the injury, respectively. The other patient underwent laparotomy after 2 days of follow-up because the abdominopelvic CT result in the Emergency Department did not show prominent bowel injury. The ascending colon perforation was observed during the surgery; hence, a right hemicolectomy was performed with primary fascia closure. Three patients had no intraabdominal organ injury. The injury mechanisms of those patients are cough due to vocal cord cancer, fall from 2 m high and motor vehicle collision for each. The patient injured by motor vehicle collision also had rib fractures on same side of lumbar hernia.
Lumbar hernias in this study were located on the right and left in 6 and 3 patients, respectively. No case was bilateral. Hernia sizes varied from 1 cm to 15 cm in diameter (mean, 6.7 cm; median, 5 cm). The hernia sacs mostly contained preperitoneal fat, but it contained the ascending colon in one patient. Complications involving incarceration or strangulation were not found.
The lumbar hernia classification criteria suggested by Moreno-Egea et al. [1] in 2007 was used to evaluate the types of hernia in our patients. Five patients had type A (small and minor type) lumbar hernias, and 2 patients each had types B (moderate type) and C (large and severe types). Type D (pseudohernia) lumbar hernias were not observed.
The hernia repair was performed by using a traditional open approach or laparoscopic approach (Table 2). Five and 3 patients underwent open and laparoscopic hernia repairs, respectively. The other patient refused to undergo hernia repair. The operative method differed based on the type; a laparoscopic approach was used for hernia types A and B, and an open approach was used for hernia types A and C (Table 3).
A prosthetic mesh was used for hernia repair in 7 patients. The mesh could not be applied for hernia repair in 1 patient with an ascending colon perforation because of the high probability of infection. In the open repair technique, a prosthetic mesh was applied in 4 patients, except in 1 patient with an ascending colon perforation. Onlay or sublay mesh placement with transfascial fixation (Fig. 2) was used. In 1 open case, we used a titanium tacker to fix the prosthetic mesh on the fascia layer for stability.
Laparoscopic repair used the total extraperitoneal approach in 3 patients, and mesh was used in all 3 patients. Because the peritoneum was not opened, we expected fewer complications and morbidities due to adhesion. In the laparoscopic approach, the prosthetic mesh was applied by using scroll or classic technique (scroll technique, 2 patients; classic technique, 1 patient). The mesh was fixed by using a titanium tacker (Fig. 3).
No severe postoperative complications were found (Table 3). Two patients had minor wound seromas, and only 1 patient had a wound infection, which needed percutaneous drainage catheter insertion. Complications were observed only with the open methods, although they were not statistically significant. However, the laparoscopic approach is generally used in less severe types of hernia; hence, it cannot be concluded that the laparoscopic approach is implicitly less likely to cause complications compared with the open approach.
No patient experienced lumbar hernia recurrences, but the follow-up was only 6 months, which was too short for evaluating recurrence. In our situation, however, longer tracking was not possible for many of the patients because they did not visit the hospital again unless they developed new symptoms.
The traumatic lumbar hernias are rare and clinical characteristics of them are diverse. So they may be overlooked or treated inappropriately in emergency situations. Zhou et al. [4] reported the clinical features of primary acquired lumbar hernias. Their findings showed that men >60 years old who performed physical labor were prone to lumbar hernias, and men were more vulnerable than women. However, in our study, no difference was found in the prevalence between men and women. No difference was found in the accidents that caused traumatic lumbar hernias between men and women.
The most common clinical manifestation of lumbar hernias is a palpable mass that increases in size with coughing and strenuous activity, is usually reducible, and disappears when the patient lies supine [1]. Common symptoms include nonspecific abdominal discomfort, fatigue, and back pain along the area of distribution of the sciatic nerve. If lumbar hernia is accompanied by bowel obstruction, nausea, vomiting, abdominal distension, and a palpable mass may be present. If the hernia contents are renal, the patient could have urinary symptoms, such as hematuria, oliguria, and colicky pain [56]. Other rare manifestations are pelvic mass and retroperitoneal and gluteal abscesses [789]. In our study, the origin of lumbar hernia was a traumatic event, and most of the lumbar hernias were diagnosed by CT scans before the patients could present with the symptoms described above. Acquiring abdominal CT scans can determine the hernia type and existence of the lumber hernia and aid in the differential diagnosis.
The location and size of traumatic lumbar hernias have no specific features. For primary spontaneous lumbar hernia, the most common site is the superior lumbar triangle (Grynfeltt-Lesshaft triangle) (Fig. 4). A superior lumbar hernia is a primary lumbar hernia that is more common, larger, and deeper than the inferior lumbar hernia [10]. In lumbar hernias with trauma origin, the inferior lumbar triangle is more common according to the review of Burt et al. [2]. Our study showed that the location could not be classified either as the superior or inferior triangle; the hernias' defects were distributed in both areas. Therefore, we did not classify lumbar hernias by their locations but instead used the classification system of Moreno-Egea et al. [1]. They proposed a classification system with a therapeutic aim that identified 4 types of hernias based on 6 criteria: size, location, hernia sac contents, muscular atrophy, origin, and previous recurrence. The presence of 2 criteria is enough to define the type of lumbar hernia. We were able to use this classification system even if we did not know the exact location of the lumbar hernia. In our study, small and minor type hernias were more common than large and severe types. We speculate that this was because the trauma patients did not have congenital weak lesions on the lumbar site.
The management plan of lumbar hernia is generally surgical. The natural course of traumatic lumbar hernia is a gradual increase in size and progression of symptoms. Therefore, most surgeons think that hernias should be repaired surgically in all patients except those at high risk [12]. In the cases of traumatic lumbar hernia, the patients mostly had other injuries. We performed the emergency surgery first and then repaired the hernias later. However, surgical hernia repair is more difficult in advanced cases; hence, hernia repair should be performed as soon as possible if other emergency treatments were completed [1].
Consequently, we considered a laparoscopic approach if the hernia was a minor or moderate type (type A or B) while planning the treatment strategy. The open hernia approach requires a large incision and dissection area, which are associated with various morbidities, such as wound pain and surgical site infection [1112]. The laparoscopic approach has the advantage of being minimally invasive; however, it does not allow for parietal reconstruction or repair under controlled tension [131415161718]. Therefore, treatment plans should be carefully considered, and if possible, the laparoscopic approach should be used. In this study, we used a laparoscopic approach in type A and B hernias (type A, 1; type B, 2). The open approach was used in type A and C hernias (type A, 3; type C, 2). Relatively small and moderate hernias tended to be repaired by the laparoscopic method. Before 2013, however, we repaired type A hernias using the open method because of technical problems.
The hernia repair should always be performed with the mesh extended to provide maximum overlap around the perimeter (6 cm) and adequate fixation [1319]. Primary repair may be performed for small and minor defects, but the failure rate is high, which may be because of the low elasticity of the lumbar area tissue. Currently, repairs using prosthetic mesh are generally preferred.
In summary, traumatic lumbar hernia of the abdominal wall is a relatively rare injury. Suspecting lumbar hernia when patients have high-energy injuries to the torso area is essential. Abdominopelvic CT scans should be obtained in every suspected case [2021]. Use of the classification system may help to diagnosis and manage lumbar hernias. Hernia repairs should use a prosthetic mesh to prevent recurrence. The operation timing should be decided after considering the patient's general condition and combined injuries. Elective repair can be performed after other acute conditions become stable.
Figures and Tables
Fig. 1
Abdominopelvic CT scan (A: axial view, B: coronal view) shows the lumbar area wall defect (arrows).
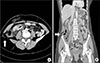
Fig. 2
Mesh fixation. Transfascial fixations are used to fix mesh around the margin of the defect. The periphery of mesh is fixed to the abdominal wall with tacks and to the psoas muscle with sutures.

Fig. 3
Total extraperitoneal approach was used for laparoscopic hernia repair. Arrows indicate lumbar wall defect in the extraperitoneal space. Arrowheads indicate preperitoneal fat in the hernia site.

Fig. 4
Anatomic locations of lumbar hernias. (a) Superior lumbar hernia (Grynfeltt-Lesshaft triangle). (b) Inferior lumbar hernia (Petit triangle).

ACKNOWLEDGEMENTS
We dedicate this research to Dr. Min Chung who devoted his life to challenging and researching hernias.
References
1. Moreno-Egea A, Baena EG, Calle MC, Martinez JA, Albasini JL. Controversies in the current management of lumbar hernias. Arch Surg. 2007; 142:82–88.

2. Burt BM, Afifi HY, Wantz GE, Barie PS. Traumatic lumbar hernia: report of cases and comprehensive review of the literature. J Trauma. 2004; 57:1361–1370.

3. Geis WP, Saletta JD. Lumbar hernia. In : Nyhus LM, Condon RE, editors. Hernia. Philadelphia (PA): Lippincott;1989. p. 401–415.
6. Shuhaiber J, Dunn T, Evans A, Fishman D, Merlotti G, Salzman S. Traumatic lumbar hernia with ureteropelvic junction disruption: case report and review of the literature. J Trauma. 2003; 55:985–988.

7. Biotois H, Couinaud C. A case of lumbar hernia favoring the formation of a mass in the pelvic colon. J Chir (Paris). 1969; 98:27–30.
8. Lauritzen JB, Ebbehoj N. Retropancreatic abscess. Intermittent lumbar hernia. Ugeskr Laeger. 1985; 147:526.
9. Zub A, Kozka M. Petit's triangle hernia clinically mimicking gluteal abscess. Przegl Lek. 2003; 60:Suppl 7. 86–87.
10. Skrekas G, Stafyla VK, Papalois VE. A Grynfeltt hernia: report of a case. Hernia. 2005; 9:188–191.

11. Arca MJ, Heniford BT, Pokorny R, Wilson MA, Mayes J, Gagner M. Laparoscopic repair of lumbar hernias. J Am Coll Surg. 1998; 187:147–152.

12. Bickel A, Haj M, Eitan A. Laparoscopic management of lumbar hernia. Surg Endosc. 1997; 11:1129–1130.

13. Moreno-Egea A, Torralba-Martinez JA, Morales G, Fernandez T, Girela E, Aguayo-Albasini JL. Open vs laparoscopic repair of secondary lumbar hernias: a prospective nonrandomized study. Surg Endosc. 2005; 19:184–187.

14. Heniford BT, Iannitti DA, Gagner M. Laparoscopic inferior and superior lumbar hernia repair. Arch Surg. 1997; 132:1141–1144.

15. Shekarriz B, Graziottin TM, Gholami S, Lu HF, Yamada H, Duh QY, et al. Transperitoneal preperitoneal laparoscopic lumbar incisional herniorrhaphy. J Urol. 2001; 166:1267–1269.

16. Meinke AK. Totally extraperitoneal laparoendoscopic repair of lumbar hernia. Surg Endosc. 2003; 17:734–737.

17. Postema RR, Bonjer HJ. Endoscopic extraperitoneal repair of a Grynfeltt hernia. Surg Endosc. 2002; 16:716.

19. Moreno-Egea A, Aguayo JL. Ambulatory laparoscopic repair of inferior lumbar or Petit hernia: a case report. Surg Endosc. 2002; 16:1107.
20. Salameh JR, Salloum EJ. Lumbar incisional hernias: diagnostic and management dilemma. JSLS. 2004; 8:391–394.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download